Robin DiPasquale, ND, RH (AHG)
The cough is a symptom, but a symptom of what? Often, a cough will occur with a cold or flu, causing inflammation of the mucous membranes in the throat or bronchi, which can lead to the development of mucus. The cough is the body’s attempt to expel the accumulated mucus. A cold or flu will generally develop because of a lowered resistance to infection, usually related to poor dietary choices, inadequate or disturbed sleep, a lack of exercise, a lack of spending time outdoors in fresh air, and improper elimination. Addressing these lifestyle factors and treating the whole person, not just the cough, will bring optimal outcomes.
The teachings of Samuel Thomson, Jethro Kloss, and John Christopher recommend repeated nasal irrigation and gargling with salt water to clear the nasal passages and throat of any accumulated mucus and microbial contributing factors.1-3 In addition to respiratory causes, these herbalists all suggest that a cough may result from a disorder of the stomach. In a stomach disorder, digestion is impaired, fermentation and putrification occur, and phlegm is formed, resulting in a cough. If a stomach disorder is the cause, the use of an emetic may clear the accumulated phlegm. It seems that the use of emetic herbs is recommended less often in current naturopathic practice than in the past, most likely because of the immediate discomfort to the patient. Returning to the use of emetic herbs for this type of cough can help to clear the accumulations as well as to renew the vital force.
Emetic herbs are given at subemetic doses. The emesis is followed by 2 to 3 cups of hot sage or red sage tea to wash the stomach. Other herbs may also be considered for this same outcome, including hyssop, yarrow, black cohosh, peppermint, and chamomile.
The stomach disorder should also be addressed by enhancing digestion and improving the absorption of nutrients. Composition Powder was formulated by Samuel Thomson as a stimulant and to warm the stomach, increasing the digestive fire and enhancing digestive function. The formula for Composition Powder is:
- 2 lb Myrica cerifera
- 1 lb Tsuga Canadensis
- 1 lb Zingiber officinale
- 2 oz Capsicum minimum
- 2 oz Syzygium aromaticum
All herbs should be powdered and combined. Dosage is one teaspoon in ½-cup boiling water. The tea should be drunk as it cools, and the dose should be repeated every hour for 5 to 6 doses.
Bayberry is an alterative, stimulant, and tonic astringent. Cayenne and ginger are warming and stimulating, as is clove, which is also an aromatic. Hemlock inner bark is astringent and diuretic.1
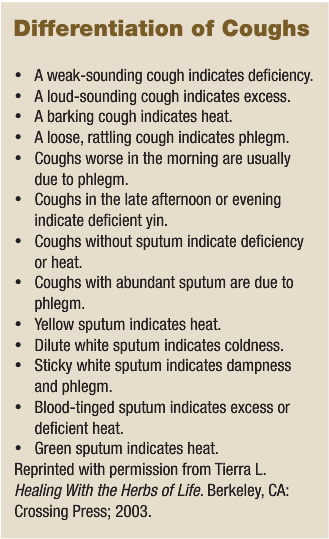
In Traditional Chinese Medicine, the lungs rule the qi. They are the interface where the qi from outside the body meets the qi inside the body. When there is a cough, it involves the lung qi. In TCM, the etiology of a cough is evaluated based on overall organ and qi flow and may include a deficiency, an excess, or imbalances of heat, coldness, dampness, or phlegm. Organs that most commonly influence the lungs are the spleen (deficiency can cause mucus to develop and invade the lungs), liver (liver fire can invade the lungs), and kidneys (kidneys can fail to grasp the lung qi). A cough can be linked to physical or emotional causes. The following are a few patterns to help differentiate the cause of a cough.
Acute coughs can be an exterior pattern or an interior pattern. An example of an exterior pattern is a cough from a cold or flu, described as a breakdown of the protective qi, with invasion of the lungs. There are three patterns of pathogen development involved with invasion of the lungs: wind-cold, wind-heat, or wind-dryness. With the wind-cold pattern, the patient will feel chilly, will be averse to cold, will not sweat, and will have a runny nose with a white discharge. The patient with wind-heat factors will have a fever, will be averse to heat, will be sweating slightly, and will have a runny nose with a yellow discharge. The patient with wind-dryness factors will be averse to wind and cold and will have a dry mouth, dry lips, a dry throat, a stuffy nose, and no discharge..
Interior patterns are lung heat and lung phlegm-heat. Lung heat is a dry pattern with fever, sweating, barking cough, and slight yellow sputum. Patients with lung phlegm-heat will also have a fever, will sweat, and will have a barking cough, but there is profuse expectoration of yellow, sticky mucus as well. Each of these exterior and interior patterns will require different herbs to bring about resolution of the cough.
A cough can develop from two lung qi patterns that have emotional etiologies. A significant pattern is injured lung qi secondary to emotional stress, particularly sadness and grief, because grief is the emotion of the lungs. A cough can develop after a significant loss, the death of a loved one, or the ending of a relationship. The second pattern is lung qi attacked by liver qi stagnation, usually the result of long-time unresolved anger, frustration, and resentment.
Two diet- and lifestyle-related lung qi patterns with cough are damp and phlegm settling in the lungs and phlegm and heat settling in the lungs. Individuals with the damp and phlegm pattern usually have a diet consisting of excess sweets, dairy, greasy foods, iced drinks or foods, juices, flour products, and raw foods. Phlegm and heat settling in the lungs can usually be triggered by excess alcohol, spicy foods, and greasy foods.
Chronic cough can be an excess pattern or a deficiency pattern, with various expressions. Often related to chronic illnesses over extended periods of time, chronic cough can have both the lung qi and the kidney qi weak and deficient. The lung qi naturally descends and disperses throughout the body. It is the job of the kidney qi to grasp the lung qi and assist it with descending. A chronic cough can result from failure of the lung qi to descend or a weakened kidney qi being unable to assist the lung qi in its downward motion. If there is difficulty with inhalation, it is more related to kidney qi deficiency. If there is difficulty with exhalation, it is more related to lung qi deficiency.4-6 Weakness or deficiency of the kidney qi can be correlated with dysfunction of the adrenal glands, adrenal fatigue, or exhaustion. Hence, resolution of the cough sometimes occurs through support of the adrenal glands.
In Western herbal medicine, there are various action categories of herbs, each bringing a different aspect of support and resolution when formulated to treat a cough. The following is a limited materia medica by category.
Expectorants clear secretions from the air passages by two mechanisms: thinning the secretions and moving them upward and outward. Demulcents can be considered to have expectorant action because they, too, thin mucus, but they are treated as a separate category. The two types of expectorants, stimulating and warming, can be used together, if indicated.
Stimulating expectorants are movers and shakers, clearing congestion through increasing mucociliary action and essentially acting as an emetic. Examples of strongly stimulating expectorants include Cephaelis ipecacuanha, Urginea maritima, and Lobelia inflata (also a relaxant; dose dependent).
 Plants that are high in saponin levels create an irritation in the pharynx and bronchi, stimulating expectoration. Some herbs included in this group are Primula veris, Bellis perennis, Saponaria spp, Polygala senega, and Glycyrrhiza glabra, which is also a demulcent.
Plants that are high in saponin levels create an irritation in the pharynx and bronchi, stimulating expectoration. Some herbs included in this group are Primula veris, Bellis perennis, Saponaria spp, Polygala senega, and Glycyrrhiza glabra, which is also a demulcent.
Warming expectorants are used for productive coughs with profuse mucus production, usually seen with cold, damp conditions in the body or in cold, damp climates. They increase blood flow, decrease the viscosity of catarrh, and warm the area, diminishing cold. These are the warm, spicy herbs often used in cooking. Examples include: Z. officinale (use fresh to move blood in the periphery; use dry to heat the core), Cinnamomum cassia (also a demulcent; mucilaginous), Pimpinella anisum (sweeter and cooler than fennel), Foeniculum vulgare (a bit warming and carminative on the stomach), and S. aromaticum (very heating).
The sulphur-containing herbs are also considered warming expectorants. They alter the mucopolysaccharide structure, thinning mucus and making it easier to move. These include: Allium sativum, Brassica nigra, Armoracia rusticana, and Capsicum annuum (can be found in this group of stimulating expectorants, as well, but may be too heating for some).
Demulcents are soothing and cooling to mucous membranes, decreasing inflammation and stimulating the flow of mucus, and are indicated for dry coughs that are irritating and nonproductive. These are the mucilaginous herbs, some of which are more specific for a cough because of the other actions they carry. Included in this group are Althaea officinalis (as well as the Malva species), Ulmus fulva, Plantago spp (demulcent and anti-catarrhal simultaneously; antimicrobial), G. glabra (also a stimulating expectorant), Tussilago farfara (antitussive and antispasmodic; contains pyrrolizidine alkaloids [PAs]), Symphytum officinale (contains PAs), and Verbascum thapsus (which some classify as a demulcent; I find it more drying, like a sponge, so it could be considered an anti-catarrhal or a stimulating expectorant; can be irritating to the pharynx with dry coughs).
Doing the opposite work of the demulcents are the anti-catarrhal herbs, which are tonifying and slightly astringent to mucous membranes and diminish puffy tissue, especially when there is a thick, profuse secretion. In addition to the herbs, pineapple, lemon, orange, and grapefruit can all be used to loosen attached phlegm. Herbs in this group are: Euphasia officinalis, Sambucus nigra, Solidago canadensis, V. thapsus, Eriodictyon californica, and Plantago spp.
 At times, it is necessary to stop the cough. This can be especially important at night, to allow for a good night’s sleep, which can enhance recovery. The antitussive herbs are used for severe, persistent, or nervous coughs when expectorants are not working effectively. The cyanogenic glycosides have the ability to depress the cough reflex and are found in some remedies in the Rosaceae family, including Prunus serotina and Prunus amygdalus. The opiates, found in small amounts in Lactuca spp and Eschscholzia californica, can also be considered when the cough lingers and prevents recovery.
At times, it is necessary to stop the cough. This can be especially important at night, to allow for a good night’s sleep, which can enhance recovery. The antitussive herbs are used for severe, persistent, or nervous coughs when expectorants are not working effectively. The cyanogenic glycosides have the ability to depress the cough reflex and are found in some remedies in the Rosaceae family, including Prunus serotina and Prunus amygdalus. The opiates, found in small amounts in Lactuca spp and Eschscholzia californica, can also be considered when the cough lingers and prevents recovery.
Spasmolytic herbs work through the nervous system, relaxing the smooth muscles of the air passages. These herbs are used for tight, nonproductive coughs. The plants in the Solanaceae family, which contain atropine, work in this way and were used extensively by the eclectic and pysiomedical physicians. Atropa belladonna, Hyoscyamous niger, Datura stramonium, and Solanum dulcamara all act to quiet a cough, although their anticholinergic action can make them too drying. Other plants in this group are Ephedra sinica, Petasites officinalis (spasmolytic and sedative), Hyssopus officinalis, Thymus vulgaris (antimicrobial, as well), Grindelia robusta, Marrubium vulgare (extremely bitter; works for the stomach and digestion), L. inflata (relaxant through antispasmodic action; emetic in larger doses), and Inula racemosa (antimicrobial; trophorestorative to the respiratory system).
One last group to keep in mind when formulating for a cough is antimicrobial herbs. There are many to choose from, and several of the following have specificity for the lungs: Ligusticum porteri, Lomatium dissectum, I. racemosa, Commiphora molmol, and Populus spp. (the most active aspect of the tree is the high level of resin coating the buds in the spring).
The materia medica is extensive when it comes to treating a cough. Understanding the cause of a cough will allow for more specific and more effective therapeutic outcomes.
 Robin DiPasquale, ND, RH (AHG) earned her degree in naturopathic medicine from Bastyr University in 1995 where, following graduation, she became a member of the didactic and clinical faculty. For the past eight years, she has served at Bastyr as Department Chair of Botanical Medicine, teaching and administering to both the naturopathic medicine program and the bachelor’s of science in herbal sciences program. Dr. DiPasquale is a clinical associate professor in the department of biobehavioral nursing and health systems at the University of Washington in the CAM certificate program. She loves plants, is published nationally and internationally, and teaches throughout the U.S. and in Italy about plant medicine. She is an anusara influenced yoga teacher, teaching the flow of yoga from the heart. She currently has a general naturopathic medicine practice in Madison, Wis. and is working with the University of Wisconsin Integrative Medicine Clinic as an ND consultant.
Robin DiPasquale, ND, RH (AHG) earned her degree in naturopathic medicine from Bastyr University in 1995 where, following graduation, she became a member of the didactic and clinical faculty. For the past eight years, she has served at Bastyr as Department Chair of Botanical Medicine, teaching and administering to both the naturopathic medicine program and the bachelor’s of science in herbal sciences program. Dr. DiPasquale is a clinical associate professor in the department of biobehavioral nursing and health systems at the University of Washington in the CAM certificate program. She loves plants, is published nationally and internationally, and teaches throughout the U.S. and in Italy about plant medicine. She is an anusara influenced yoga teacher, teaching the flow of yoga from the heart. She currently has a general naturopathic medicine practice in Madison, Wis. and is working with the University of Wisconsin Integrative Medicine Clinic as an ND consultant.
References
- Moore L. Classical Formulas in the Western Herbal Tradition. Shortsville, NY: Author; 2002.
- Kloss J. Back to Eden. Santa Barbara, CA: Woodbridge Press Publishing; 1975.
- Christopher JR. School of Natural Healing. Provo, UT: Christopher Publications; 1976.
- Tierra L. Healing With the Herbs of Life. Berkeley, CA: Crossing Press; 2003.
- Kaptchuk T. The Web That Has No Weaver. New York, NY: Congdon & Weed; 1983.
- Bensky D, Barolet R. Chinese Herbal Medicine Formulas & Strategies. Seattle, WA: Eastland Press; 1990.





