David Nortman, ND
Docere
We spend 1/4 to 1/3 of our time sleeping (or trying to), yet most medical care is focused on our waking hours. Sound sleep heals and restores the organism on all levels. Poor sleep, on the other hand, may cause, maintain, or exacerbate any chronic complaint. Optimal health is therefore critically dependent on sound sleep. Yet sleep is still a poorly understood phenomenon and a challenging one to address in the clinic. Securing the patient’s cooperation in improving sleep is an ongoing battle, especially in the context of a culture in which sleep is viewed as an unfortunate impediment to the more important strivings of our daytime existence. Despite its immense importance, sleep medicine, which emerged as a distinct medical discipline only in the latter half of the 20th century, is glossed over in medical and naturopathic training, and sleep specialists still represent but a small fraction of the medical profession.
Next to insomnia, breathing-related sleep disorders – collectively referred to as sleep-disordered breathing (SDB) – are the most prevalent of all sleep disorders. SDB encompasses benign snoring, obstructive sleep apnea syndrome (OSAS) and much rarer non-obstructive disorders such as central sleep apnea (CSA), where the actual impulse to breathe is disordered. OSAS, in turn, encompasses the spectrum ranging from airflow limitation (upper-airway resistance syndrome [UARS]), to partial- or full-airway obstruction (obstructive sleep apnea [OSA]). This article is intended as a comprehensive primer on OSAS (ie, obstructive SDB), given that OSAS constitutes the vast majority of SDB.*
Unlike insomnia, with which it is only sometimes associated, OSAS has a non-specific clinical presentation and usually escapes the sleeper’s conscious awareness. As a result, it tends to be under-reported by patients, under-diagnosed by clinicians, and under-treated once diagnosed. Estimates of its prevalence vary widely, ranging from <5% to >20% in men, and somewhat less in women; more than 80% of cases remaining undiagnosed.1-3 Naturopathic patients are not exempt from these statistics, and there is increasing evidence that OSAS is responsible for a sizable portion of the total chronic-disease burden.4
Unobstructed breathing through the night is crucial for our well-being, yet viewing OSAS as a frequent cause of chronic illness is remote from current medical and naturopathic thinking. Considering, however, that patients seek naturopathic care primarily for longstanding chronic issues, it is well worth screening for OSAS, especially when we encounter treatment-resistant conditions. In naturopathic practice we may, of course, inadvertently improve the condition of the airway by addressing the mind-body connection, reducing inflammation, or resolving subtle muscle tension in the throat, but at other times airway health may need to be addressed directly. Developing a working knowledge of the diagnosis and treatment of OSAS is therefore an indispensible addition to our skill-set.
Pathophysiology
The Upper Airway
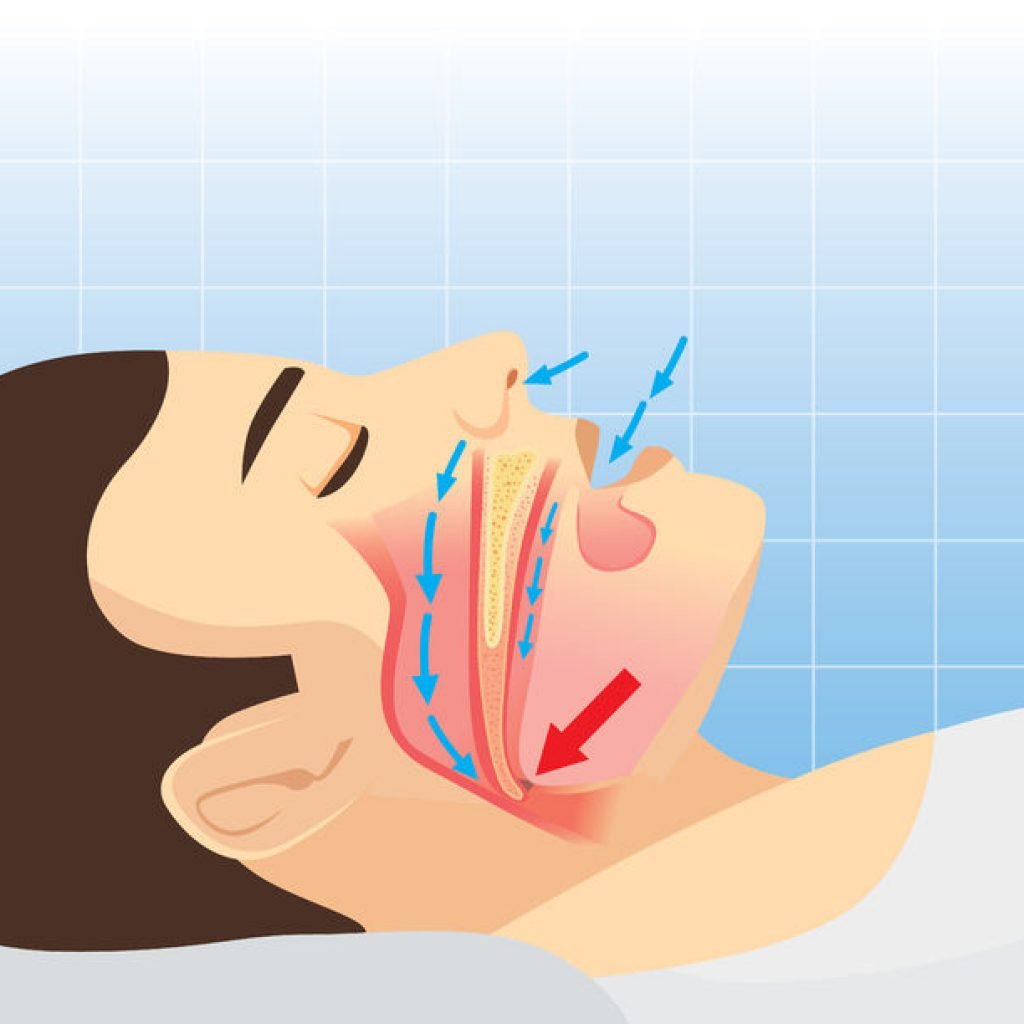
The cause of OSAS is malfunction of the upper airway. Whereas the larynx is a rigid tube dedicated to the task of breathing, the upper airway has to fulfill additional functions that require anatomical freedom and adaptability; this makes it susceptible to failure as a breathing apparatus. Moreover, our recent evolution into upright creatures with a face in the frontal position means that the upper airway – originally straight and less prone to obstruction, as in most other mammals – has to curve around the tongue and soft palate. These factors, when combined with the effects of modern child-rearing practices on dental and facial development, may account for the high prevalence of airway-related sleep disorders, even in apparently healthy individuals.5
Airflow may be interrupted by obstructions in the nasal passages due to structural defects, growths, or inflammation. These tend to be easier to recognize and treat than airway restriction or collapse due to the soft palate, uvula, or tongue, which tend to occur only in sleep and sometimes only in the supine position. Airway patency is determined by the state of the surrounding tissues, namely by muscle tone, degree of inflammation, fat content, and other subtle factors that are still poorly understood. Airway patency is also a function of its size, which is determined by the structure of the upper and lower jaws that collectively anchor the tissues and muscles that constitute its anterior wall. The proper development of the jaw is dependent on physical stimulation throughout childhood, primarily the sucking motion of the infant at the breast, nasal breathing (which allows the tongue to rest forward in the mouth so as to lean against the developing dental arches), and chewing on sufficiently solid foods. Without these stimuli the jaw could end up recessed or narrow, thereby reducing the size of the airway and predisposing it to collapse.
Sleep Fragmentation
Normal sleep architecture involves a gradual descent into deep sleep – stages 3 and 4 (or N3) of non-REM (NREM) sleep** – also known as delta sleep or slow-wave sleep (SWS). This is followed, typically after a transition into lighter NREM sleep, by an episode of REM sleep, before the pattern begins anew, repeating itself several times until waking. The bulk of deep NREM sleep occurs earlier in the night, whereas episodes of REM sleep increase in frequency and duration toward morning.
Sleep fragmentation is the disruption of this normal sleep architecture by arousals from any cause. In OSAS, sleep fragmentation is due to muscle atonia, which is pronounced during deep NREM and maximal during the paralysis of REM sleep. Deep NREM sleep is associated with growth-hormone release and physical recovery, and once interrupted cannot be resumed right away, while REM sleep is associated primarily with mental recovery. Both are crucial for the well-recognized restorative effects of sleep on body and mind. Tragically, the upper airway is most susceptible to collapse precisely when its integrity is most needed.
Full or partial upper-airway collapse leading to hypoxemia (arterial oxygen desaturation), or in some cases merely increased airflow resistance and respiratory effort, tends to terminate in an arousal event (“microarousal”) – a momentary awakening that almost always goes unnoticed by the patient – that re-establishes respiration at the cost of interrupting sleep at the neurological level. The recurrent sleep fragmentation and increased respiratory effort greatly reduce sleep efficiency, and may prevent restorative sleep regardless of its length.
Mechanisms of Obstruction in OSA & UARS
In classic OSA, sleep is interrupted by a combination of apneas and hypopneas. An apnea is defined as the absence of airflow for at least 10 seconds followed by hypoxemia or arousal. A hypopnea is typically defined as reduced airflow for at least 10 seconds followed by minor hypoxemia or arousal; however, the definition is not standardized and the diagnostic thresholds are subject to variability. In contrast to central apneas or hypopneas, where the respiratory drive is absent, obstructive apneas and hypopneas are associated with ongoing or increased respiratory effort.
Although common sense may suggest that arousals are triggered by a drop in oxygen saturation, they appear instead to be related primarily to increased respiratory effort due to the diaphragm encountering resistance from the compromised airway.6 In fact, the existence of respiratory effort-related arousals (RERAs) unrelated to apneas, hypopneas, or oxygen desaturation has led to the recent proposal of a new diagnostic category, the upper-airway resistance syndrome (UARS).7 There is still disagreement as to whether UARS is an early or mild form of OSAS or a distinct clinical entity; for the time being, it is officially subsumed under OSAS.8
UARS is thought to be caused by airway narrowing that produces airflow limitation sufficient to trigger arousals in sensitive individuals, without collapsing the airway.9 The cause of airway narrowing is more often craniofacial abnormality (eg, recessed or narrow jaw) or mechanical obstruction (eg, enlarged tonsils) than tissue laxity, so the condition does not tend to progress to OSA except with increased body mass index (BMI). Diagnosing UARS is challenging because quantifying airflow limitation is a more intricate matter than counting discrete apneas or hypopneas. Furthermore, UARS seems to affect all ages, including children and younger, fit, low-to-normal BMI females – populations commonly encountered in the naturopathic clinic. For these reasons, in the interest of promoting diagnostic sensitivity it may be helpful to regard UARS as a separate condition.
Consequences of Untreated OSAS
The immediate effects of OSAS are similar to those of sleep deprivation, affecting emotional well-being, cognition, alertness, and physical coordination, and potentially endangering others through car or workplace accidents. The long-term consequences, though insidious, are ultimately severe. On the psychological front, reduced cognition and motivation may over time derail the patient’s entire life course. Chronic sleep deprivation produces body-wide inflammation, elevating the risk of the full range of chronic diseases. Untreated OSAS has been associated with elevated risk of stroke, heart disease, diabetes, obesity, dementia and Alzheimer’s disease, reduced life span, and other pathologies, and is increasingly thought to be a major contributing factor to these conditions.10
Considering how commonly OSAS goes untreated, it should be considered a major public-health priority. As naturopathic physicians, the least we can do is to identify those cases that require airway-specific medical care in addition to the naturopathic care we provide.
Diagnosis
Assuming normal mental health, sleep should terminate in waking up relaxed, sharp, clear-headed, and positively disposed toward the coming day – even after only 6-7 hours of sleep, and even in relatively old age. Chronically unrefreshing sleep might, of course, be due to insomnia, but the possibility of OSAS should always be considered as well. Insomnia unrelated to an organic cause is more often than not sleep-onset insomnia, and is typically associated with factors such as depression, anxiety, periodic limb movement disorder, or exogenous factors such as stimulants, or disruption of the diurnal cycle; sleep onset can also be affected by the anticipation of unrefreshing sleep. The insomnia of OSAS, on the other hand, more often presents as interrupted sleep (sometimes with nocturia) or early-morning waking. Crucially, the insomnia of OSAS tends to be resistant to the usual array of insomnia treatments.
The symptoms of OSAS need not, however, be related to insomnia, nor need they be primarily sleepiness or fatigue, because poor sleep is often compensated for, with minimal symptoms, for many years. Patients become habituated to their baseline waking state, some have never known truly restful sleep, or they may attribute their state to stress, aging, medication side-effects, and the like. Some patients, especially those invested in a healthy lifestyle, may resist or deny the very idea that they are sleeping poorly, even when confronted by evidence, and it is in such younger, fit people that OSAS is most often overlooked.
Screening for SDB
Of the various forms of SDB, only classic OSA is recognized by the public and non-specialist clinicians. The popular image of the OSA patient is that of an overweight, snoring, older man whose breathing is periodically interrupted before resuming with a gasp. In the conventional medical family practice, only the classic OSA is normally screened for, often starting with the Epworth Sleepiness Scale (ESS) or STOP-BANG questionnaires, which pick out the most obvious cases. The following signs and symptoms are typically looked for:
- Loud snoring, especially with irregularities (snorting, gasping, unusual sounds)
- Pauses in breathing
- Daytime sleepiness or fatigue
- Weight gain, high BMI, or increased neck circumference
- Cognitive, emotional, or psychomotor impairment
- Morning headaches
While the classic picture accurately describes the more severe cases, the milder or subtler forms of OSAS need not involve snoring, are collectively more widespread, and may afflict anyone, including children and young, fit females. SDB predisposes patients to the full array of chronic diseases and early demise, so the cost of overlooking it is considerable. OSAS specifically tends to worsen with age when left untreated, so early diagnosis is important.
Only laboratory sleep investigation can provide a definitive diagnosis of SDB, so as naturopathic physicians, our task is to screen for its presence without being concerned about a false-positive diagnosis. The diagnostic strategy should therefore aim at maximizing sensitivity, a task at which we are especially adept, given that adequate screening for OSAS requires the thoroughness of a naturopathic intake. In addition to the usual naturopathic history, it helps to perform a quick airway-centered physical exam and history – the sort that in the ideal world would be performed by a dentist – in order to screen for the following risk factors:
- Recessed jaw, often with overbite/overjet
- Narrow or V-shaped dental arches, crowded or crooked teeth, high-arched palate (indicative of a narrow mandible or maxilla)
- Unreasonable or uneven acid erosion of teeth or reported nocturnal GERD (indicative of nocturnal acid reflux due to increased respiratory effort)
- Bruxism or mechanical erosion of teeth (bruxing helps to open the airway)
- Enlarged tonsils or adenoids
- Scalloped, centrally fissured, or large tongue; poor visibility of the soft palate, uvula, and oropharynx past the tongue (indicative of narrow inferior dental arch or large tongue)
- Tongue tie
- Obstruction of nasal cavity (deviated septum, polyps, allergy, inflammation)
- Mouth breathing (observed or reported)
- Temporomandibular joint (TMJ) issues
- History of tooth extraction as part of orthodontic treatment
Other potential indicators of OSAS include the following:
- Nocturia (antidiuretic hormone [ADH] secretion is reduced when deep sleep is disrupted)
- Nocturnal limb movements or restlessness
- Morning dry mouth or sore throat
- Decreased sleep latency (falling asleep too quickly) at night, or daytime tendency to nap or doze off
- Carbohydrate or caffeine cravings, afternoon sleepiness (ie, secondary adrenal fatigue)
- Persistent or treatment-resistant hypertension
- Depression, anxiety, loss of vigor and motivation
- Persistent obesity, uncontrollable weight gain, or onset of sleepiness after weight gain
- Erectile dysfunction
- Threatening course of an unidentified disease
- Persistent sympathetic over-activation
- Family history of OSAS or its sequelae
When upper-airway resistance rather than obstruction predominates, the following conditions may be encountered11:
- Anxiety disorders
- Chronic fatigue syndrome
- Fibromyalgia
- Irritable bowel syndrome
- Chronic headaches
- Hypotension
Interestingly, such conditions are commonly seen in naturopathic practice and are often difficult to treat, so the possibility of OSAS as their causative factor should be carefully considered. Proper diagnosis is also important, such as in depression secondary to OSAS, given that antidepressants may actually exacerbate the underlying pathology due to weight gain, lower muscle tone, or inhibition of arousals leading potentially to hypoxia.12
The clinical presentation of OSAS is nonspecific and therefore must be confirmed by a sleep study before proceeding to treatment. These topics will be covered in Part 2 of the article.
*The diagnostic approach to non-obstructive SDB is similar to that of obstructive SDB, given that their symptoms are similar and both require a confirmatory sleep study. Obstructive SDB is often associated with conditions such as heart failure and stroke and requires specialized medical attention and highly customized ventilatory therapy. Obstructive and non-obstructive SDB may also coexist within a patient.
** Because stage 3 of NREM sleep is a transitional state between stages 2 and 4, in recent years the 4 stages have been contracted to 3 (N1, N2, N3), with N3 comprising stages 3 and 4 of the older system. Both systems are in current use.
References:
- Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: A population health perspective. Am J Respir Crit Care Med. 2002;165(9):1217-1239.
- Kapur V, Strohl KP, Redline S, et al. Underdiagnosis of sleep apnea syndrome in U.S. communities. Sleep Breath. 2002;6(2):49-54.
- Young T, Evans L, Finn L, Palta M. Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep. 1997;20(9):705-706.
- Phillipson EA. Sleep apnea – a major public health problem. NEJM. 1993;328(17):1271-1273.
- Corruccini RS. An epidemiological transition in dental occlusion in world populations. Am J Orthod. 1984;86(5):419-426.
- Aldrich MS. Sleep Medicine. Oxford, England: Oxford University Press; 1999: 215-216.
- Guilleminault C, Stoohs R, Clerk A, et al. A Cause of Excessive Daytime Sleepiness: The Upper Airway Resistance Syndrome. Chest. 1993;104(3):781-787.
- Guilleminault C, Chowdhuri S. Upper airway resistance syndrome is a distinct syndrome, and Douglas NJ Upper airway resistance syndrome is not a distinct syndrome. Am J Respir Crit Care Med. 2000;161(5):1412-1416.
- Arora N, Meskill G, Guilleminault C. The role of flow limitation as an important diagnostic tool and clinical finding in mild sleep-disordered breathing. Sleep Sci. 2015;8(3):134-142.
- Fu Y, Xia Y, Yi H, et al. Meta-analysis of all-cause and cardiovascular mortality in obstructive sleep apnea with or without continuous positive airway pressure treatment. Sleep Breath. 2017;21(1):181-189.
- Gold AR. Functional somatic syndromes, anxiety disorders and the upper airway: A matter of paradigms. Sleep Med Rev. 2011;15(6):389-401.
- Winkelman JW, Plante DT, eds. Foundations of Psychiatric Sleep Medicine. Cambridge, England: Cambridge University Press; 2010: 120.
Image Copyright: <a href=’https://www.123rf.com/profile_logo3in1′>logo3in1 / 123RF Stock Photo</a>
 David Nortman, ND, studied at the University of Toronto before graduating from CCNM in 2004. More recently he completed a master’s degree in Philosophy of Science from Tel-Aviv University. Dr Nortman has completed extensive training in classical homeopathy, utilizing it to address the full spectrum of chronic conditions. He practices locally in Toronto and worldwide on a long-distance basis, and serves as a homeopathic consultant and mentor to naturopathic colleagues. Dr Nortman has published numerous articles in homeopathic journals and has lectured to both lay and academic audiences. Currently, he is writing a book on homeopathy and its interaction with modern science and philosophy. Website: www.homeopathyzone.com.
David Nortman, ND, studied at the University of Toronto before graduating from CCNM in 2004. More recently he completed a master’s degree in Philosophy of Science from Tel-Aviv University. Dr Nortman has completed extensive training in classical homeopathy, utilizing it to address the full spectrum of chronic conditions. He practices locally in Toronto and worldwide on a long-distance basis, and serves as a homeopathic consultant and mentor to naturopathic colleagues. Dr Nortman has published numerous articles in homeopathic journals and has lectured to both lay and academic audiences. Currently, he is writing a book on homeopathy and its interaction with modern science and philosophy. Website: www.homeopathyzone.com.