Naturopathic Strategies for Neuropsychiatric Symptoms
YASAMAN TASALLOTI, ND
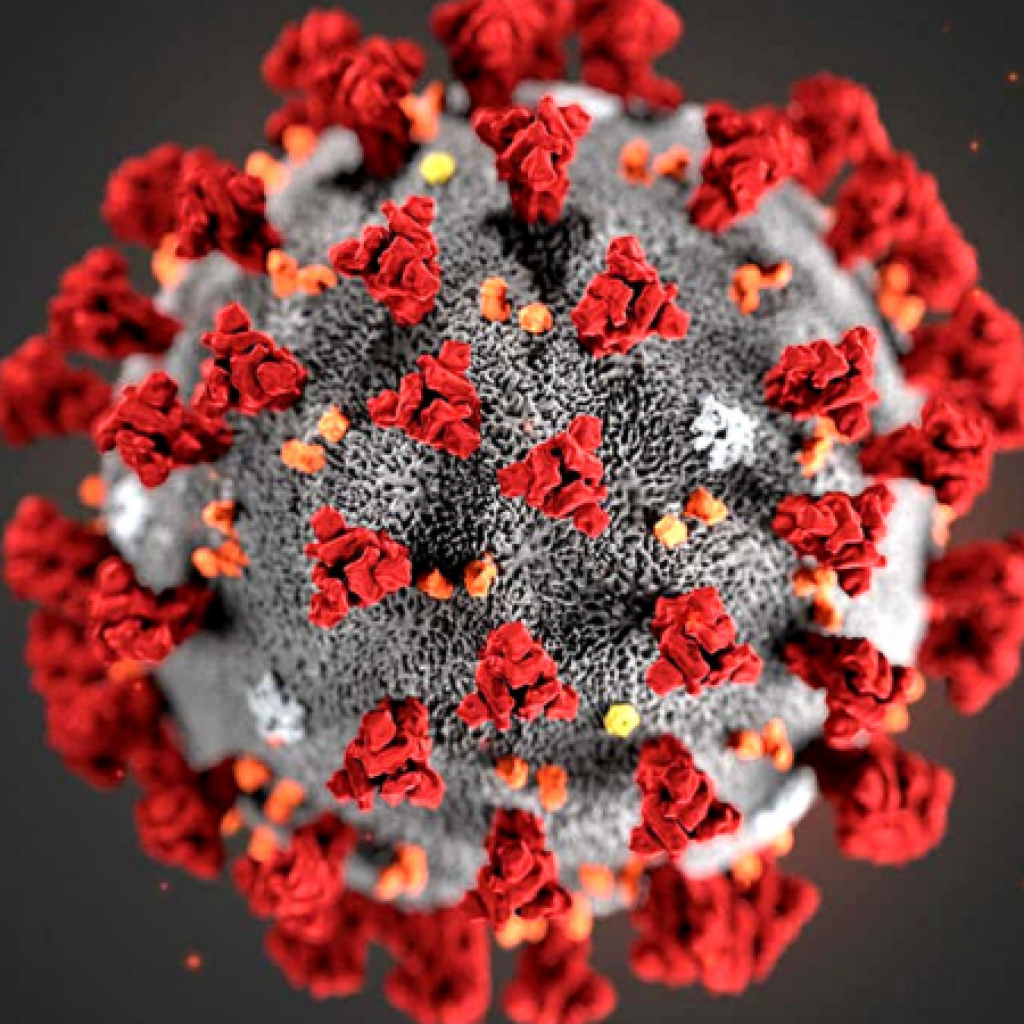
For the last 2 years, the world has been experiencing a multitude of effects from the COVID-19 pandemic. While many individuals have fully recovered, a subset continues to experience the lingering symptoms of the virus known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Symptoms lasting longer than 12 weeks have been coined long COVID. Neuropsychiatric symptoms such as fatigue, brain fog, sleep disturbances, and depression are considered some of the top concerns that long COVID patients face. In the search for treatment solutions that can help these individuals, there are a few naturopathic strategies that have been beneficial. These include improving mitochondrial health, supporting methylation pathways, and fortifying the microbiome.
Long COVID Pathophysiology
As it has been determined thus far, the spike protein of SARS-CoV-2 binds to angiotensin-converting enzyme 2 (ACE2) receptors, present on a variety of cells. Viral entry into the cell then initiates a cascade of inflammatory events, including the activation of proinflammatory cytokines. For long COVID cases, these proinflammatory cytokines persist, contributing to immune dysregulation and even autoimmunity in some cases. Neuroinflammation occurs directly via damage to neural tissue caused by the virus, and indirectly due to inflammatory molecules crossing the blood-brain barrier, thus creating the basis for pathologic neuropsychiatric symptoms.1
SARS-CoV-2 and Neuroinflammation
Mitochondria play an important role in innate immune responses by prompting interferon release and stimulating apoptosis of infected cells.2 Viruses such as SARS-CoV-2 can damage mitochondria in a few ways. First, the considerable amount of oxidative stress that the virus creates can damage the mitochondria directly. Second, once SARS-CoV-2 attaches to the ACE2 receptor, it can disrupt lipid and glucose metabolism that normally occurs in the mitochondria,3 resulting in systemic inflammation and neuroinflammation. Mitochondrial dysfunction has long been associated with neurological disorders such as Alzheimer’s disease,4 Parkinson’s disease, and multiple sclerosis.5 It is not very surprising, therefore, that fatigue and brain fog are among the top concerns reported in long COVID cases.
Epigenetic alterations have been reported as a risk factor in developing long COVID. McCaddon and Regland postulated several mechanisms by which this occurs.6 The significant amount of oxidative stress caused by SARS-CoV-2 can increase the demand for S-adenosylmethionine (SAMe). A decline in SAMe levels results in an elevation in homocysteine levels, which has been linked to a variety of mood and neurological disorders.7 Elevated homocysteine levels may also contribute to the brain fog that long COVID patients experience.6 The decline in SAMe can also reduce the activity of the enzyme cystathionine b-synthase, which is responsible for the production of glutathione. Testing homocysteine levels in these individuals would be beneficial; for a deeper understanding of the patient’s methylation status, a methylation panel may be ordered.
Maintaining the health of the gut microbiome is paramount for immune homeostasis. Gut microbiota can regulate both innate and adaptive immune responses. When dysbiosis is present, intestinal permeability can ensue and promote immune dysregulation.8 Toxic byproducts from the gut can also translocate to the brain, cause neuroinflammation, and ultimately develop into neurological disorders such as Alzheimer’s disease.9 A study found that 212 individuals who experienced severe illness from COVID-19 demonstrated a lower abundance of beneficial gut bacteria.10
In other studies, microbiome alterations were found after infection with SARS-CoV-2 as a result of proinflammatory cytokine elevation and downregulation of ACE2.8 As it relates to the health of the gastrointestinal system, ACE2 plays a role in the synthesis of antimicrobial proteins.10 It is imperative to address the health of the gut microbiome in patients who have contracted COVID-19, particularly to help prevent individuals from developing severe symptoms.
Treatment Approaches
There have been numerous studies documenting the benefits of vitamins C and D and glutathione, so I will not elaborate on these therapies. Below are other methods that address the approaches mentioned above.
Mitochondrial Support
Acetyl-L-carnitine (ALC) offers valuable support for both mitochondrial and immune system health. It can downregulate proinflammatory cytokines such as interleukin-6 (IL-6) and tumor necrosis factor alpha, inhibit nuclear factor kappa B (NF-kB), and reduce ACE1 levels. A study found that 500 mg of ALC prescribed orally per day along with light physical activity was found to improve depression and musculoskeletal pain in patients experiencing long COVID.11 Other studies show dosages of up to 3 000 mg per day to be clinically effective.12-14
Flavonoids possess antiviral, antioxidant, and anti-inflammatory properties. In particular, quercetin, naringenin, and hesperidin provide mitochondrial protection against the effects of SARS-CoV-2.15 For example, quercetin can inhibit the release of proinflammatory cytokines via suppression of the NLRP3 inflammasome.16 Foods high in quercetin include capers, red onions, buckwheat, radicchio, and dill. Naringenin, found in citrus fruits like grapefruit and pomelo, has been found to inhibit NF-kB and ACE2 activity. Hesperidin, found in lemons and other citrus fruits, can attenuate inflammatory responses by binding the spike protein of SARS-CoV-2.17 Other compounds that have been long known to provide antiviral and mitochondrial support are sulforaphanes, curcumin, and epigallocatechin gallate (EGCG).18
Methylation Support
Supplementation with B vitamins in individuals with methylation concerns improves neuropsychiatric symptoms associated with long COVID. As it relates to immunity, B vitamins can prevent viral binding and replication, lessen pro-inflammatory cytokines, and modulate the responses between the innate and adaptive immune system; additionally, B vitamins can reduce neuroinflammation.19 A study by Ragan et al demonstrated that riboflavin combined with UV light exposure reduced SARS-CoV-2 titers in plasma and whole blood samples.20 Niacin demonstrated lung protective properties due to reducing proinflammatory cytokines.19 Pyridoxal 5′-phosphate can prevent abnormal clot formation and maintain endothelial integrity, reducing the risk of strokes and myocardial infarctions associated with long COVID.19 Folic acid was studied in preventing SARS-CoV-2 from binding to cells by inhibiting the enzyme furin.19 Finally, vitamin B12 is a critical nutrient for overall neurological health; it supports myelin synthesis and affects microbiota homeostasis.19
Microbiome Support
Probiotics exert immunomodulatory effects through a variety of mechanisms. Probiotics upregulate interferon, T cell, and natural killer cell activity; inhibit viral replication; modulate cytokine responses; influence ACE2; and inhibit pathogen binding through the production of mucin.21 They can even increase the absorption of Vitamin D through enhancement of the VDR receptor.21 Several studies have documented various probiotic strains that improved COVID-19 symptoms and reduced the severity of the disease.22-24 Specific strains such as Lactobacillus plantarum, Lactobacillus rhamnosus, and Bifidobacterium longum were helpful not just against COVID-19, but also in improving neurological and psychiatric health.25
Low-Dose Naltrexone
One other therapy to consider is low dose naltrexone (LDN), especially in severe cases. LDN can lower the inflammatory response through several pathways. First, LDN binds to opioid receptors and stimulates the body to increase opioid growth factor (OGF) while increasing receptor sensitivity.26-27 OGF can reduce inflammation, enhance immunity, and promote autophagy. Second, LDN can suppress pro-inflammatory cytokines such as interleukins 1b and 6, monocyte chemoattractant protein-1, and transforming growth factor beta28; these are part of the cytokine storm that causes severe reactions in COVID-19 cases. LDN also reduces levels of certain T cells, especially Th1 and Th17 cells.29 Interestingly, LDN can decrease pro-inflammatory cytokines while increasing anti-inflammatory cytokines.29 Third, LDN can inhibit extracellular signal-related kinases 1 and 2 (ERK1 and ERK2), which are known to contribute to viral replication.30 Additionally, LDN can inhibit the binding of the receptor binding domain of SARS-CoV-2 to ACE2, which is another mechanism by which SARS-CoV-2 affects our cells.30
Final Thoughts
Although COVID-19 has created much disturbance and suffering in our society, there is much we can learn from this pandemic. Our naturopathic philosophy and tools continue to provide invaluable support in providing symptom relief and restoring the health of individuals. Doctors who serve individuals managing long COVID should incorporate strategies including reducing oxidative stress, supporting methylation pathways, and balancing the microbiome.
References
- Hunter P. Viral diseases and the brain: Long COVID puts the spotlight on how viral infections affect the brain: Long COVID puts the spotlight on how viral infections affect the brain. EMBO Rep. 2022;23(1):e54342.
- Elesela S, Lukacs NW. Role of Mitochondria in Viral Infections. Life (Basel). 2021;11(3):232.
- Ganji R, Reddy PH. Impact of COVID-19 on Mitochondrial-Based Immunity in Aging and Age-Related Diseases. Front Aging Neurosci. 2021;12:614650.
- Wilkins HM, Swerdlow RH. Relationships Between Mitochondria and Neuroinflammation: Implications for Alzheimer’s Disease. Curr Top Med Chem. 2016;16(8):849-857.
- Monzio Compagnoni G, Di Fonzo A, Corti S, et al. The Role of Mitochondria in Neurodegenerative Diseases: the Lesson from Alzheimer’s Disease and Parkinson’s Disease. Mol Neurobiol. 2020;57(7):2959-2980.
- McCaddon A, Regland B. COVID-19: A methyl-group assault?. Med Hypotheses. 2021;149:110543.
- Varshney KK, Gupta JK, Mujwar S. Homocysteine Induced Neurological Dysfunctions: A Link to Neurodegenerative Disorders. International Journal of Medical Research & Health Sciences. 2019;8(4):135-146.
- Hussain I, Cher GLY, Abid MA, et al. Role of Gut Microbiome in COVID-19: An Insight Into Pathogenesis and Therapeutic Potential. Front Immunol. 2021;12:765965.
- Reyes REN, Gao L, Asatryan L. Microbiome meets microglia in neuroinflammation and neurological disorders. Neurology and Neuroinflammation. 2020;7:215-233.
- Reinold J, Farahpour F, Fehring C, et al. A Pro-Inflammatory Gut Microbiome Characterizes SARS-CoV-2 Infected Patients and a Reduction in the Connectivity of an Anti-Inflammatory Bacterial Network Associates With Severe COVID-19. Front Cell Infect Microbiol. 2021;11:747816.
- Scaturro D, Vitagliani F, DiBella VE, et al. The Role of Acetyl-Carnitine and Rehabilitation in the Management of Patients with Post-COVID Syndrome: Case-Control Study. Applied Sciences. 2022;12(8):4084.
- Vaziri-Harami R, Delkash P. Can l-carnitine reduce post-COVID-19 fatigue?. Ann Med Surg (Lond). 2022;73:103145.
- Keshani M, Alikiaii B, Askari G, et al. The effects of L-carnitine supplementation on inflammatory factors, oxidative stress, and clinical outcomes in patients with sepsis admitted to the intensive care unit (ICU): study protocol for a double blind, randomized, placebo-controlled clinical trial. Trials. 2022;23(1):170.
- Fathizadeh H, Milajerdi A, Reiner Ž, et al. The effects of L-carnitine supplementation on indicators of inflammation and oxidative stress: a systematic review and meta-analysis of randomized controlled trials. J Diabetes Metab Disord. 2020;19(2):1879-1894.
- Kicinska A, Jarmuszkiewicz W. Flavonoids and Mitochondria: Activation of Cytoprotective Pathways?. Molecules. 2020;25(13):3060.
- Saeedi-Boroujeni A, Mahmoudian-Sani MR. Anti-inflammatory potential of Quercetin in COVID-19 treatment. J Inflamm (Lond). 2021;18(1):3.
- Cheng FJ, Huynh TK, Yang CS, et al. Hesperidin Is a Potential Inhibitor against SARS-CoV-2 Infection. Nutrients. 2021;13(8):2800.
- Ghidoli M, Colombo F, Sangiorgio S, et al. Food Containing Bioactive Flavonoids and Other Phenolic or Sulfur Phytochemicals With Antiviral Effect: Can We Design a Promising Diet Against COVID-19?. Front Nutr. 2021;8:661331.
- Ragan I, Hartson L, Pidcoke H, et al. Pathogen reduction of SARS-CoV-2 virus in plasma and whole blood using riboflavin and UV light. PLoS One. 2020;15(5):e0233947.
- Shakoor H, Feehan J, Mikkelsen K, et al. Be well: A potential role for vitamin B in COVID-19. Maturitas. 2021;144:108-111.
- Kurian SJ, Unnikrishnan MK, Miraj SS, et al. Probiotics in Prevention and Treatment of COVID-19: Current Perspective and Future Prospects. Arch Med Res. 2021;52(6):582-594.
- Gutiérrez-Castrellón P, Gandara-Martí T, Abreu Y Abreu AT, et al. Probiotic improves symptomatic and viral clearance in Covid19 outpatients: a randomized, quadruple-blinded, placebo-controlled trial. Gut Microbes. 2022;14(1):2018899.
- Singh K, Rao A. Probiotics: A potential immunomodulator in COVID-19 infection management. Nutr Res. 2021;87:1-12.
- Antunes AEC, Vinderola G, Xavier-Santos D, et al. Potential contribution of beneficial microbes to face the COVID-19 pandemic. Food Res Int. 2020;136:109577.
- Dolan KE, Finley HJ, Burns CM, et al. Probiotics and Disease: A Comprehensive Summary-Part 1, Mental and Neurological Health. Integr Med (Encinitas). 2016;15(5):46-58.
- Donahue RN, McLaughlin PJ, Zagon IS. Low-dose naltrexone targets the opioid growth factor-opioid growth factor receptor pathway to inhibit cell proliferation: mechanistic evidence from a tissue culture model. Exp Biol Med (Maywood). 2011;236(9):1036-1050.
- Toljan K, Vrooman B. Low-Dose Naltrexone (LDN)-Review of Therapeutic Utilization. Med Sci (Basel). 2018;6(4):82.
- Parkitny L, Younger J. Reduced Pro-Inflammatory Cytokines after Eight Weeks of Low-Dose Naltrexone for Fibromyalgia. Biomedicines. 2017;5(2):16. Published 2017 Apr 18.
- El Shehaby DM, Mohammed MK, Ebrahem NE, et al. The emerging therapeutic role of some pharmacological antidotes in management of COVID-19. The Egyptian Journal of Bronchology. 2022;16(1).
- Choubey A, Dehury B, Kumar S, et al. Naltrexone a potential therapeutic candidate for COVID-19. J Biomol Struct Dyn. 2022;40(3):963-970.

Yasaman Tasalloti, ND, is passionate about helping women get to the bottom of their health concerns with an individualized naturopathic medical approach so they can focus on what matters most to them. She emphasizes mental and emotional aspects of illness to uncover toxic thought patterns that may contribute to an internal state of imbalance. Dr Tasalloti firmly believes it is possible for every woman to attain her greatest level of health, given appropriate treatment options and her willingness to take part in her health journey. Her website is www.DrYasND.com, and her Facebook page is www.facebook.com/dryasnd.