Millie Lytle, ND, MPH
As an ND subscribing to the great capacity of preventive medicine, I believe innately that food consumption and mood have a connection. Until a few years ago, possible biological mechanisms were not obvious in the literature. During these years, I started seeing patients with mood disorder as a major part of my practice base. In treating these patients, I have heard many reports of weight gain, night cravings, and binging patterns related to pharmacotherapy intervention. Compared with my other patients, this group was less knowledgeable about nutrition and lifestyle and had fewer coping mechanisms and more disordered eating behaviors. Although patients tended to blame their mood disorder, I assessed that part of the weight gain was owing to lifestyle, mood, and metabolic causes. Many of these patients had high glucose and lipid levels, elevated blood pressure, central obesity, and further carbohydrate cravings coinciding or worsening with the prescription of antidepressant medication (selective serotonin reuptake inhibitors, selective noradrenergic reuptake inhibitors, or atypical antipsychotics).
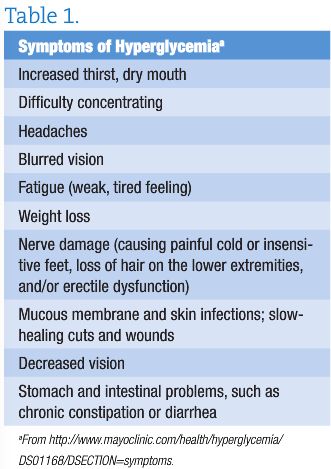
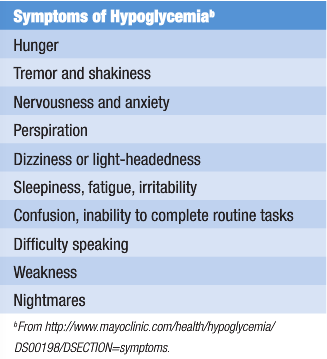
On identifying that hyperglycemia or hypoglycemia symptoms and panic or anxiety symptoms had much overlap, I began to suspect that my patients might not be able to tell where one group of symptoms ended and the other began. So, I decided to include this education in the treatment protocol.
 I was asked by the clinic director to design a diet plan for a cognitive behavior therapy (CBT) group weight loss program that would attempt to prevent weight gain secondary to pharmacotherapy treatment. As I started to research the most effective diet principles for this population, I started to wonder if a nutrition program might not only result in weight loss but also have potential for improvement of the mood disorder itself. In observing and correcting the diets of patients I was counseling, it became clear that a potential biological connection between a diet low in nutrition, high in food sensitivities, and high in simple carbohydrates could worsen mood symptoms. My ultimate goal was that the diet would correct mood via mediation of the metabolic pathways. From this research, the Food for Mood Diet was born, a series of dietary principles that could be taught in a group or individual setting over a series of weeks, along with Judith Beck’s CBT weight loss principles (http://www.beckinstitute.org).
I was asked by the clinic director to design a diet plan for a cognitive behavior therapy (CBT) group weight loss program that would attempt to prevent weight gain secondary to pharmacotherapy treatment. As I started to research the most effective diet principles for this population, I started to wonder if a nutrition program might not only result in weight loss but also have potential for improvement of the mood disorder itself. In observing and correcting the diets of patients I was counseling, it became clear that a potential biological connection between a diet low in nutrition, high in food sensitivities, and high in simple carbohydrates could worsen mood symptoms. My ultimate goal was that the diet would correct mood via mediation of the metabolic pathways. From this research, the Food for Mood Diet was born, a series of dietary principles that could be taught in a group or individual setting over a series of weeks, along with Judith Beck’s CBT weight loss principles (http://www.beckinstitute.org).
The Food for Mood Diet is a series of eating guidelines based on naturopathic nutrition and nutritional research. Between 2008 and 2010, I was involved in piloting the CBT weight loss program with Monica Vermani, PsyD (http://www.startclinic.ca/). Although we have no publication at this point, our preliminary results showed a mean weight loss of 16 lb over a 16-week period among 12 psychiatric patients, male and female. A literature review and dietary guidelines are discussed herein.
 Mood disorders are among the fastest rising conditions worldwide. It has been estimated that by 2020 depression will rank second in disease burden worldwide and first in developed countries.1 Depression and its comorbidities (general anxiety disorder, social phobia, panic disorder, and obsessive-compulsive disorder) have been linked to obesity and other chronic conditions of metabolism involving glucose, insulin, and lipid abnormalities. Diet is also linked to metabolic disorders, such as type 2 diabetes mellitus and the metabolic syndrome. Although many medical treatments are available for mood disorders, including pharmacotherapy and psychotherapy, there remain gaps in treatment and concern regarding adverse events. However, it is plausible that dietary mediation of metabolic laboratory markers has a role; until recently, there has been a lack of understanding of the biological function of nutrition in patients with mood disorder. As the rates of these chronic diseases increase, it is becoming ever more crucial to address the physiological connection between diet and mood disorders and to explore the metabolic causes. While the literature reflects that effective medical treatments for depression and anxiety exist, obvious gaps in comprehensive care remain. Integrative mental healthcare applies the most effective tools from medicine and complementary and alternative medicine to create the best possible outcomes.2 Research has shown a predictive correlation between the increasing rates of depressive disorders and the group of symptoms that fall under the umbrella of the metabolic syndrome.3 Therefore, a series of dietary principles was compiled as the Food for Mood Diet to attempt a nutritional counseling treatment for patients with depression who are at risk of metabolic disorders.
Mood disorders are among the fastest rising conditions worldwide. It has been estimated that by 2020 depression will rank second in disease burden worldwide and first in developed countries.1 Depression and its comorbidities (general anxiety disorder, social phobia, panic disorder, and obsessive-compulsive disorder) have been linked to obesity and other chronic conditions of metabolism involving glucose, insulin, and lipid abnormalities. Diet is also linked to metabolic disorders, such as type 2 diabetes mellitus and the metabolic syndrome. Although many medical treatments are available for mood disorders, including pharmacotherapy and psychotherapy, there remain gaps in treatment and concern regarding adverse events. However, it is plausible that dietary mediation of metabolic laboratory markers has a role; until recently, there has been a lack of understanding of the biological function of nutrition in patients with mood disorder. As the rates of these chronic diseases increase, it is becoming ever more crucial to address the physiological connection between diet and mood disorders and to explore the metabolic causes. While the literature reflects that effective medical treatments for depression and anxiety exist, obvious gaps in comprehensive care remain. Integrative mental healthcare applies the most effective tools from medicine and complementary and alternative medicine to create the best possible outcomes.2 Research has shown a predictive correlation between the increasing rates of depressive disorders and the group of symptoms that fall under the umbrella of the metabolic syndrome.3 Therefore, a series of dietary principles was compiled as the Food for Mood Diet to attempt a nutritional counseling treatment for patients with depression who are at risk of metabolic disorders.
The metabolic syndrome, formerly known as syndrome X, includes the following criteria4: central obesity (waist circumference ≥102 cm in men or ≥88 cm in women), hypertension (blood pressure ≥130/85 mm Hg or undergoing treatment with blood pressure medications), high fasting blood glucose level (≥110 mg/dL or undergoing treatment with diabetes medications), and lipid instability (high triglycerides level ≥150 mg/dL and low high-density lipoprotein cholesterol level <40 mg/dL in men or <50 mg/dL in women). The chief predictors of mortality are hypertension and high fasting blood glucose level.
Stress and nutrition have important roles in depressive conditions. Wurtman5 found that when under trauma or stress a malnourished or obese individual was susceptible to anxiety and depression. Lustig6 suggests that a likely cause is the effect on blood glucose and insulin levels after stimulation of the hypothalamic-pituitary-adrenal axis (HPA axis). The physiological cascade would look like Table 2:
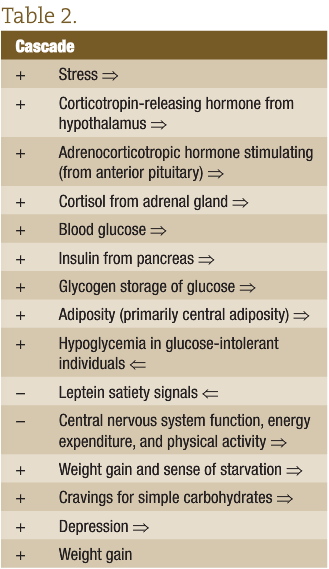
The cascade in Table 2 continues putting increased stress on all endocrine organs, the cardiovascular system, and the liver until diagnosis of the metabolic syndrome, diabetes, or heart disease.6 As shown in the cascade, this results in insulin storage of glucose as glycogen, increasing adiposity and inducing hypoglycemia in glucose-intolerant individuals. The first part of the negative loop shows that leptein satiety signals are diminished, causing a sense of starvation, subsequent cravings for immediate carbohydrates, weight gain, dampened central nervous system function, decreased desire for energy expenditure and physical activity, and increased depression because of a combination of reasons.
The Food for Mood Diet
1. Mitigate Stress by Eating Every 3-4 Hours
The cascade continues putting increased stress on all endocrine organs, the cardiovascular system, and the liver until diagnosis of the metabolic syndrome, diabetes, or heart disease.6 As shown in the cascade, this results in insulin storage of glucose as glycogen, increasing adiposity and inducing hypoglycemia in glucose-intolerant individuals. The first part of the negative loop shows that leptein satiety signals are diminished, causing a sense of starvation, subsequent cravings for immediate carbohydrates, weight gain, dampened central nervous system function, decreased desire for energy expenditure and physical activity, and increased depression because of a combination of reasons.
2. Avoid All-Carbohydrate Meals
While trauma, medication, and daily stress have a large role in mediation of the HPA axis, predisposing patients to mood disorders, the metabolic syndrome, and other chronic illness, research shows that daily nutrient intake can alter the ability of an individual to cope, either preempting or facilitating a continuation of the HPA-induced glucose and insulin resistance.7 These findings suggest that a metabolic risk–mediated dietary counseling regimen may be effective in treating depressive disorders by moderating the intake, type, and ratios of carbohydrates, protein, and fats in the diet and the physiological response to these foods. Furthermore, researchers in Canada found that a behavior therapy weight control program for patients with antipsychotic-induced weight gain was effective in normalizing weight and controlling for metabolic risk profile. This shows that dietary approaches to mood disorders can be incorporated into primary treatment in an integrative setting with pharmacotherapy.
3. Fiber is filling; sugar is killing
In a 2002 cross-national epidemiological study of major depression and bipolar disorder, Westover and Marangell8 reported a correlation between sugar consumption (calories per capita per day) and national prevalence of major depression. Although the cause was speculative, 6 countries demonstrated an association of sugar consumption with annual depression rate. High oxidative stress and low β-endorphin production were considered predictive factors. The investigators concluded that further research is needed to elucidate this connection.
4. Eat the vegetables too. No matter what else you eat, never skip the greens.
In a clinical trial, Markus9 found that eating regular meals that include complex carbohydrates (with fiber) results in better performance, improved mood, and increased tryptophan levels. Stress was found to increase cortisol, blood glucose, and insulin levels and to worsen mood and cognitive performance. Wurtman5 also found that dietary (and pharmacological) interventions that increase serotonin activity normalize food intake and diminish depressed mood, suggesting that daily diet can affect future food intake. What one eats 1 day has an effect on one’s dietary choices, portion sizes, and mood up to 11 days later.10
5. Make the best choice you can right now. But don’t beat yourself up for making mistakes.
Flood et al11 observed that eating low-calorie high-fiber vegetables in salads or soups increases satiety without increasing blood glucose levels. In contrast, drinking soda pop and other high-calorie beverages does not increase satiety but increases glucose levels and overall caloric intake.
6. Start a meal with soup or salad
Nabb and Benton12 found that individuals with higher glucose tolerance report better mood. Although the brain functions on glucose, those who eat breakfasts containing greater amounts of simple carbohydrates report fatigue and memory loss. A diet lacking in protein causes fatigue, light-headedness, brain fog, and persistent hunger, which may be concomitant with anxiety and depressive symptoms. Eating complex carbohydrates is beneficial, while eating simple carbohydrates may be detrimental. An excessive intake of carbohydrate-rich foods and a resistance to engaging in physical activity will increase a depressed mood.
7. Eat protein at every meal and snack, including healthy ferments, probiotics, and algae.
Bourre13 summarizes that the quality of fatty acids, amino acids, and carbohydrates consumed in the diet has a compelling effect on the function and structure of the brain. It affects moment-to-moment performance, especially in glucose-intolerant individuals and among older populations.
Research shows a direct link between high sugar consumption in the daily diet and diabetes and mood disorders due to a negative feedback cascade in the HPA axis. Because diseases like diabetes and mental illness are the result of a process that develops over time, the signs, symptoms, and metabolic damage can go on for years or decades before translation into a medical diagnosis. As NDs and other complementary and alternative medicine practitioners know, prevention involves recognizing signs and symptoms of a disease process before its diagnosis.
The Food for Mood Diet is a series of principles delivered in a 2-hour group setting over a 12-week period. During these 12 weeks, study patients learn a series of nutritional principles to apply to their daily food intake. They are counseled using CBT principles on how to control cravings, avoid binge eating, and stop emotional eating. Classes include opportunity for patients to discuss their challenges, share recipes, receive support from the facilitator and other enrollees, and participate in a nutrition lesson on a particular topic of the week.
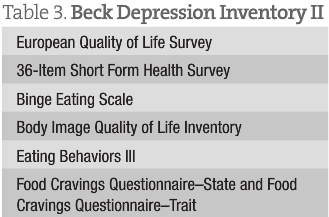 Our initial Food for Mood Diet study has the following inclusion criteria for patients at entry, midpoint, and end of the study: (1) Participants must report symptoms of depression or have physician-diagnosed depression, and their Beck Depression Inventory II score must indicate mild to moderate depression (score, 14-28). (2) Participants must meet criteria for 1 or more symptom of the metabolic syndrome (the symptoms by Mozaffarian et al4 are listed at the beginning of the article).
Our initial Food for Mood Diet study has the following inclusion criteria for patients at entry, midpoint, and end of the study: (1) Participants must report symptoms of depression or have physician-diagnosed depression, and their Beck Depression Inventory II score must indicate mild to moderate depression (score, 14-28). (2) Participants must meet criteria for 1 or more symptom of the metabolic syndrome (the symptoms by Mozaffarian et al4 are listed at the beginning of the article).
Patients must agree to the following: (1) Laboratory workup, including fasting early morning blood draw to determine cortisol, fasting glucose, and fasting lipid levels (high-density and low-density lipoprotein cholesterol levels, their ratio, and triglycerides level). (2) Physical examination, including weight for body mass index calculation and waist circumference measurement at the umbilicus. (3) Suggested subjective scales to be administered at the pre-post visits. (4) Signed consent to change their diet for 12 weeks.
Exclusion criteria for the Food for Mood Diet study include patients who are deemed too ill to make lifestyle changes and patients who unwilling to participate in the study.
 Millie Lytle, ND, MPH, is an advocate in the natural health industry with over 20 years experience. She is a licensed Naturopathic Doctor (District of Columbia and Certified Nutrition Specialist living and practicing in New York and D.C.. She also has a Master in Public Health (Germany).
Millie Lytle, ND, MPH, is an advocate in the natural health industry with over 20 years experience. She is a licensed Naturopathic Doctor (District of Columbia and Certified Nutrition Specialist living and practicing in New York and D.C.. She also has a Master in Public Health (Germany).
She is the founder the Eating for Meaning, a paradigm shift into individual nutrition teaching the consumer to eat according to their own wisdom. She is also the founder of Wellpath.me, a blockchain-based tech company focusing on self-help advocates and users of alternative medicine who’s mission is to reduce the top 6 chronic diseases by 50% over 25 years. She is a published researcher and author. She has a goal of living healthy until 120 years using Eating for Meaning at www.drmillie.com
References
1. Canadian Psychiatric Association. Mental Illness Awareness Week Guidebook. Ottawa, ON: Canadian Psychiatric Association; 2001.
2. Lake J. Integrative mental health care: from theory to practice, part 2. Altern Ther Health Med. 2008;14(1):36-42.
3. Skilton MR, Moulin P, Terra JL, Bonnet F. Associations between anxiety, depression, and the metabolic syndrome. Biol Psychiatry. 2007;62(11):1251-1257.
4. Mozaffarian D, Kamineni A, Prineas RJ. Metabolic syndrome and mortality in older adults: the Cardiovascular Health Study. Arch Intern Med. 2008;168(9):969-978.
5. Wurtman JJ. Depression and weight gain: the serotonin connection. J Affect Disord. 1993;29(2-3):183-192.
6. Lustig RH. The ‘skinny’ on childhood obesity: how our Western environment starves kids’ brains. Pediatr Ann. 2006;35(12):898-902, 905-907.
7. Poulin MJ, Chaput JP, Simard V, et al. Management of antipsychotic-induced weight gain: prospective naturalistic study of the effectiveness of a supervised exercise programme. Aust N Z J Psychiatry. 2007;41(12):980-989.
8. Westover AN, Marangell LB. A cross-national relationship between sugar consumption and major depression? Depress Anxiety. 2002;16(3):118-120.
9. Markus CR. Effects of carbohydrates on brain tryptophan availability and stress performance. Biol Psychol. 2007;76(1-2):83-90.
10. Rolls BJ, Roe LS, Meengs JS. The effect of large portion sizes on energy intake is sustained for 11 days. Obesity (Silver Spring). 2007;15(6):1535-1543.
11. Flood JE, Roe LS, Rolls BJ. The effect of increased beverage portion size on energy intake at a meal. J Am Diet Assoc. 2006;106(12):1984-1991.
12. Nabb SL, Benton D. The effect of the interaction between glucose tolerance and breakfasts varying in carbohydrate and fiber on mood and cognition. Nutr Neurosci. 2006;9(3-4):161-168.
13. Bourre JM. Effects of nutrients (in food) on the structure and function of the nervous system: update on dietary requirements for brain, part 2: macronutrients. J Nutr Health Aging. 2006;10(5):386-399.


