David Schleich, PhD
We well know the central importance to professional formation of our teachers’ skills. Their ability to convey theoretical, didactic, and clinical knowledge, skills, and information is intrinsic to conveying the profession into the future. This priority is showing up in larger professional development budgets in the focus our naturopathic schools and programs have these days as they search for affordable appropriate professional development opportunities to help our full-time and part-time teachers strengthen their teaching repertoire. In the public sector (especially community colleges and 4-year colleges and in many graduate schools that have education programs), there are outstanding examples of workshops, seminars, and training series that can help. In the allopathic professional preparation schools, the issue is also well known (LCME, 2003; ACGME, 2011; Kern, Thomas, Howard, & Bass, 1998).
 The training model (Kurz & Silverman, 1996) referenced last month in this column, for example, focused on training allopathic medical school professors in ways to create and deliver curriculum that would add emphasis to making early connections between patient-physician communication aptitude and clinical reasoning. The methods for this important teaching focus included self-reflection, group discussion, videotaped encounters, role play, and feedback. The project evolved a “Communication Skills Observation Guide,” which the curriculum designers modeled after the “Calgary-Cambridge Reference Observation Guide 23” in which students encountered role-play cases for which barriers became mechanisms by which those same students could work through communication challenges (e.g., patient reluctance to discuss illicit drug use). Such projects are helpful because they effectively train the trainers; however, they do not in themselves constitute a systematic commitment to training medical educators in the basics of teaching methods, curriculum design, and measurement and evaluation.
The training model (Kurz & Silverman, 1996) referenced last month in this column, for example, focused on training allopathic medical school professors in ways to create and deliver curriculum that would add emphasis to making early connections between patient-physician communication aptitude and clinical reasoning. The methods for this important teaching focus included self-reflection, group discussion, videotaped encounters, role play, and feedback. The project evolved a “Communication Skills Observation Guide,” which the curriculum designers modeled after the “Calgary-Cambridge Reference Observation Guide 23” in which students encountered role-play cases for which barriers became mechanisms by which those same students could work through communication challenges (e.g., patient reluctance to discuss illicit drug use). Such projects are helpful because they effectively train the trainers; however, they do not in themselves constitute a systematic commitment to training medical educators in the basics of teaching methods, curriculum design, and measurement and evaluation.
Our overall challenge is to increase the understanding of teaching methodology, not only theoretically but across the broad front of naturopathic teacher preparation. The long-held assumption has been that our teachers will emerge from the profession itself and convey what is necessary in our classrooms and clinics. However, we have learned as we observe more and more teaching challenges among our students (literacy and numeracy issues, inadequate science fundamentals, weak business skills curricula, and more) that it is not enough for our teachers-clinicians just to know the content of their discipline. It is not enough that they are enthusiastic and diligent in talking about that content in a classroom or in a clinic setting, equipped with slide presentations and Web links. Rather, our teachers report that they need more support to become increasingly sophisticated in all the curriculum design and delivery skills expected of them, from knowing how to convert content into learning outcomes, to adjusting measurement and evaluation tools to accommodate special learning needs. What follows herein is a modest proposal, if I may borrow for altogether different purposes the title of Swift’s famous 1729 satirical essay.
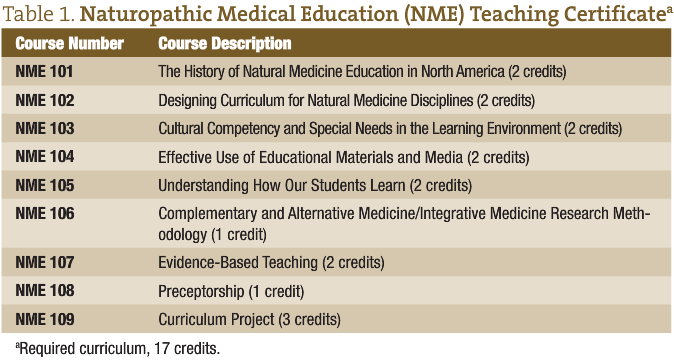
The simple outline of a training program for naturopathic medical educators (NMEs) is intended as a catalyst for discussion about what such a resource could and should look like. This outline might constitute a useful touchstone for discussion among our college or school programs and the Association of Accredited Naturopathic Medical Colleges (AANMC). The framework herein does not include specific learning outcomes and aligned methods and evaluative instruments. Rather, it is a platform that in a modest way may contribute to a frequent conversation our schools and programs and the AANMC have about how NMEs in North America can be supported. We could indeed create and deliver a routinely available “natural medicine educators certificate” to assist in the professional preparation of our teachers.
Notwithstanding the potential concerns of regional and programmatic accreditors about the design and delivery of a “credential” that is not the actual ND degree or diploma, what is suggested herein is the beginning of a simple framework for an actual credential that could have usefulness for part-time and full-time NMEs (in terms of skills building and in terms of salary and status). Such a training program, delivered at individual schools or appended to major conference gatherings, such as the American Association of Naturopathic Physicians, Northwest Naturopathic Physicians Convention, Ontario Association of Naturopathic Doctors, Health Fusion, or the British Columbia Naturopathic Association annual conference, could look something like this:
What is proposed is that anyone teaching in any of our ND programs should have the minimum prerequisites for admission to the program outlined herein. As well, the suggestion is that a credential like this one should be commonly accepted by all Council on Naturopathic Medicine Education (CNME)–accredited programs as a valid statement of acquired teaching competencies for which appropriate incremental remuneration applies. It is further suggested that the program should be free for current and potential teachers in the ND programs. Eligibility for the program might include a minimum of 5 years of demonstrated successful full-time clinical practice (including residency education). Applicants who already have master’s degree–level education credits in curriculum design and the teaching arts could be given transfer credit appropriately. In any case, as a departure point for discussion of such a program, the following minimum academic criteria could be considered:
- Doctor of naturopathic medicine degree or diploma from a CNME-accredited program
- Terminal doctoral degree in the appropriate discipline from an accredited postsecondary institution for basic sciences curricula teaching assignments
- Demonstrated experience and affiliation with a health sciences, public health, health delivery, or health education organization or institution
- Qualifying research paper (QRP) on what have been the major challenges in natural medicine education in North America (minimum of 25 pages, using American Psychological Association style format)
The fourth minimum criterion, the QRP, might be a useful screening tool at the entry level for candidates. All applicants to the NME program are required to submit, as part of the acceptance process to a cohort, a scholarly research document on the following topic: What have been the major challenges in natural medicine education in North America? The QRP will demonstrate the following: (1) Awareness of the key challenges to some aspect of natural medicine education in North America. (2) General understating of what the disciplines of natural medicine are and the contexts in which they operate. (3) Scholarly writing skills ability and aptitude.
This certificate program could be made available in some blend of convenient part-time cohort-based delivery modes. These include evening or weekend cohorts, online or distance education, summer intensives, self-directed learning modules, and supervised practicum curricula.
This program would want to recognize the importance of teaching skills and teacher training in achieving medical education excellence in all our CNME-accredited ND programs. Such a program not only can help generate a growing pool of qualified highly motivated medical educators but also can support the branding of our programs as high-quality professional preparation in North America and beyond.
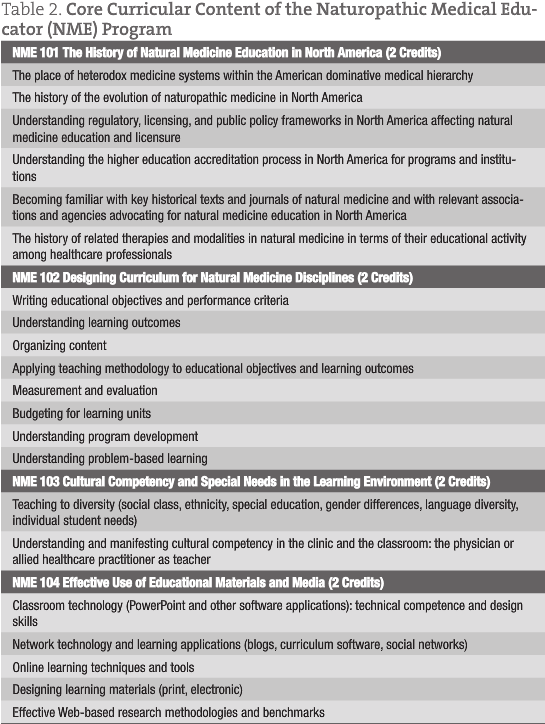
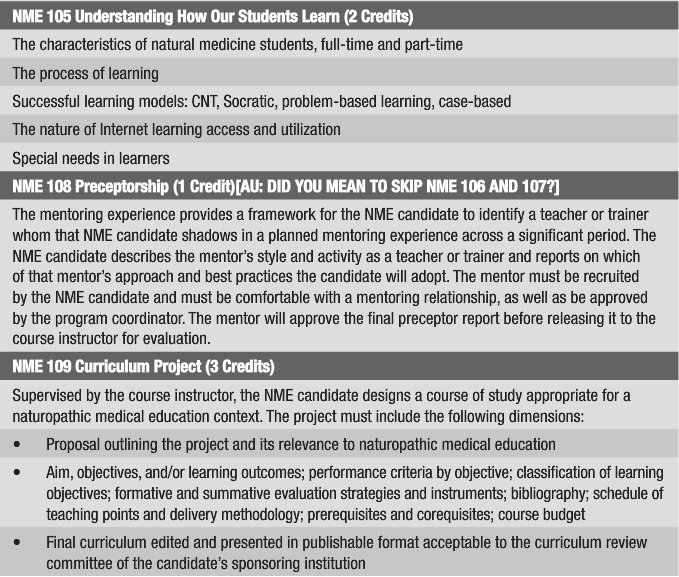
Naturopathic medical educator candidates would develop strong skills in curriculum design, program development, measurement and evaluation, research methodology (including a thorough familiarization with the agencies, priorities, resources, and processes of the complementary and alternative medicine/integrative medicine research environment), and the use for educational purposes of educational and social media. In such a program, NME candidates would also significantly enhance their understanding of evidence-based teaching. Furthermore, professional awareness could be augmented within this program in the urgent areas of cultural competency (especially as this knowledge and sensitivity influences clinical practices) and needs of exceptional learners.
The NME candidates might be expected to have verifiable teaching readiness for present and potential employers. The quality and level of preparedness could be so demonstrated not only by successful completion of the 17-credit program but also by the material example of exemplary curriculum projects and by evidence of skill and competence through comprehensive preceptor reports designed to focus attention on best practices.
Within the NME certificate program, there will be an opportunity to explore teaching methods that are not currently in wide use in CNME-accredited naturopathic programs. A case in point is the problem-based learning (PBL) process (Thomas, 1992; Rogers, Swee, & Ullian, 1991; Menahem & Paget, 1990). In PBL, learners in small groups of six to eight students encounter a problem and attempt to solve it with information they already possess, allowing them to appreciate what they already know. They also identify what they need to learn to better understand what the problem is and how to resolve it. Once they have worked with the problem as far as possible and have identified what they need to learn, the learners engage in self-directed study to research the information needed by finding and using various information resources (books, journals, reports, online information, and a variety of individuals with appropriate areas of expertise).
In this way, learning is personalized to the needs and learning styles of the individual. The learners then return to the problem and apply what they learned to their work with the problem to more fully understand and resolve the problem. After they have finished their problem work, the learners assess themselves and each other to develop skills in self-assessment and the constructive assessment of peers. Self-assessment is a skill that is essential to effective independent learning. The problems used are ill-structured messy situations like those the learner will encounter in the real world. The learning process requires the skills expected of learners when they encounter problems in their lives and careers. The learning process is supplemented by lecture and laboratory sessions to enhance the learning.
The PBL Curriculum
The series of problems encountered by learners in PBL constitute the curriculum. The problems are assembled as a group to stimulate learning of content appropriate to the course. In the PBL process, learners characteristically learn far more in areas that are relevant to their personal needs. The PBL teacher acts as an incubator for the learning process, as a key resource for it, and as a catalyst for its use in specific discipline areas. As learners become more proficient in the PBL process, the tutor becomes less active. This is a new skill for many teachers, and specific training is required.
The objectives of PBL are to produce learners who will:
- Engage the problems they face in life and career with initiative and enthusiasm
- Problem-solve effectively using an integrated, flexible, and usable knowledge base
- Use effective self-directed learning skills to continue learning as a lifetime habit
- Continuously monitor and assess the adequacy of their knowledge, problem-solving, and self-directed learning skills
- Collaborate effectively as a member of a group
There is little doubt that the efforts to integrate basic sciences, biomedical sciences. and the applied modalities of naturopathic medicine require substantial teaching skill, beginning with a deep understanding of how to design curricula that can work in a world where naturopathic medicine is continuously confronted by the dominant orthodox medical system and its massive resources. Our allopathic (also known increasingly as biopsychosocial medicine) colleagues are equally challenged by the complexities of curriculum reform at a time when trained teachers of medicine are rare. The problems they encounter are familiar. For example, Schmidt and his colleagues found that, despite attempts at curriculum reform, “Basic science dominates; at best, biopsychosocial issues are treated as separate but equal—and often as separate and not equal” (Schmidt, 1998, p. X). Professional educators with a deep love for naturopathic medicine are essential in an already overburdened curriculum delivered by too few teachers, few of whom have formal training in how to teach.
 David Schleich, PhD is president and CEO of NCNM, former president of Truestar Health, and former CEO and president of CCNM, where he served from 1996 to 2003. Other previous posts have included appointments as vice pres-ident academic of Niagara College, and administrative and teaching positions at St. Lawrence College, Swinburne University (Australia) and the University of Alberta. His academic credentials have been earned from the University of Western Ontario (BA), the University of Alberta (MA), Queen’s University (BEd) and the University of Toronto (PhD)
David Schleich, PhD is president and CEO of NCNM, former president of Truestar Health, and former CEO and president of CCNM, where he served from 1996 to 2003. Other previous posts have included appointments as vice pres-ident academic of Niagara College, and administrative and teaching positions at St. Lawrence College, Swinburne University (Australia) and the University of Alberta. His academic credentials have been earned from the University of Western Ontario (BA), the University of Alberta (MA), Queen’s University (BEd) and the University of Toronto (PhD)
References
Accreditation Council for Graduate Medical Education (ACGME). (2011). Outcome project: Enhancing residency education through outcomes assessment. Retrieved January 18, 2011, from http://www.acgme.org/Outcome.
Kern, D. E., Thomas P. A., Howard D. M., & Bass E. B. (1998). Curriculum development for medical education: A six-step approach. Baltimore: Johns Hopkins University Press.
Kurtz, S. M. & Silverman, J. D. (1996). The Calgary-Cambridge Referenced Observation Guides: An aid to defining the curriculum and organizing the teaching in communication training programmes. Medical Education, 30(2), 83-89.
Liaison Committee on Medical Education (LCME). (July 2003). Functions and structures of a medical school: Standards for accreditation of medical education programs leading to the M.D. degree. Retrieved January 12, 2011, from http://www.lcme.org.
Menahem, S. & Paget, N. (1990). Role play for the clinical tutor towards problem-based learning. Medical Teacher, 12, 57-61.
Rogers, J. C., Swee, D. E., & Ullian, J. A. (1991). Teaching medical decision making and students’ clinical problem solving skills. Medical Teacher, 13, 157-163.
Schmidt, H. (1998). Integrating the teaching of basic sciences, clinical sciences, and biopsychosocial issues. Academic Medicine, 73(9)(suppl), S24-S31.
Swift, Jonathan. (1729). A modest proposal for preventing the children of poor people in Ireland from being a burden to their parents or country, and for making them beneficial to the public. Retrieved from http://www.gutenberg.org/ebooks/1080.
Thomas, R. E. (1992). Teaching medicine with cases: Student and teacher opinion. Medical Education, 26(3), 200-207.
















