The Advance of “Narrative Medicine” in Postmodern Allopathic Curriculum
David Schleich, PhD
Back in 2009, Columbia University, in New York City, partnered with the revered Canossiano Institute in Venice, Italy, to teach MDs, nurses, and other biomedicine professionals relational skills for which the naturopathic profession has held the space in patient care for decades. Their workshop attracted U.S. and European medical credits. They called it “narrative medicine.” The teachers were from Columbia, the University of Toronto (Ontario, Canada), George Washington University (Washington, DC), Technion in Haifa (Israel), and the University of Milan, Italy. They trained participants how to “nourish empathic physician-patient relationships” and to “replace isolation with affiliation.” They presented strategies for establishing a “patient-centered and life-framed practice.” One of their themes was “achieving meaning in clinical practice.” Sound familiar?
A few months ago, the University of Iowa, Iowa City, sponsored a conference called “The Examined Life.” Participants assembled to explore “links between the science of medicine and the art of writing.” I wonder if the American Medical Association leadership noticed the strong interest in that workshop and in others like it. I wonder if they understand why this is happening.
Those elements of excellent naturopathic care—human interaction, information and education, the presence of loved ones or friends and social support in the healing journey, spirituality and inner resources, the importance of human touch, the nutritional and soothing aspects of food, and an ambience that is inviting, safe, and inspiring—that are sustained by thoughtful listening, nurturing, talking, and time spent are now getting conjugated through formal curricula in allopathic venues. This phenomenon is linked to the noisy opportunism of “integrative” medical practice. It may well be another barometer of assimilation. Many years ago, Theodore Roszak (1968) warned the counterculture that kick-started the renewal of naturopathic medicine that the status quo would unrelentingly surround and take as its own the very opposing themes and practices it had for decades rejected, attacked, and punished.
In that regard, so-called narrative medicine, some contend, is more evidence of an accelerating co-opting of the essence of natural medicine. Several of the educational assumptions of this increasingly popular technique are somewhat antithetical to straight-ahead four-on-the-floor biomedicine clinics and health services businesses. Narrative medicine, whatever its patina, is emerging in the front lines of the previously mechanized and rationalized biomedicine landscape. Because the alternative (what NDs do, for example, and have been doing for a century on this continent) is bumping into turf and market share that has been secured for a long time by the orthodox allopathic medical system, more and more MDs are encountering well-informed patients who resent 7-minute prescriptions, emotional distance, and depersonalization.
The biomedicine terrain has been described by those excluded from its orthodoxy as compressed, characterized by quantified time allocations per patient, embarrassed by the uninsured (but not motivated or mobilized at the leadership level to do anything about it), scourged by the tangle of rules for the insured, dominated by health maintenance organizations, and contained by reductionist medical reasoning that “blindly follows statistical likelihoods, regardless of variations such as age, sex, ethnicity, or individual psychologies” (Charon, 2006, p. X).
Dr. Charon (a PhD in English who also became an MD) is the principal architect of narrative medicine, a strategic communications approach that seeks to warm up that terrain. She teaches that clinicians need to “develop a sturdy and clinically useful affiliation with the one who suffers” (Charon, 2008) In such a universe, the biomedicine professionals are “witnesses” and not “judges,” “companions” and not “interrogators.” Dr. Charon never mentions NDs in her many publications, but one would swear she had apprenticed with several to see how it is done.
Charon explains that “narrative medicine had its start in . . . patient-centered care and medical humanities” (2006, p. X). In an allopathic universe, physician time is money (time spent must be quantifiable), insurance and pharmaceutical companies are locked unapologetically in a profit equation, biomedicine students learn between the first year and fourth year that emotional attachment can hurt, and medical training for the longest time objectified the patient enough that “Patch” Adams got famous satirizing the alienation. In her words, the idea is that, by really listening to the patient (for more than the customary 7 minutes), physicians can “receive in full complexity what the patient conveys in words, silences, gestures, positions, and physical findings” (Charon, 2008). Charon suggests that physicians who possess “narrative competence” are able to “bridge the divides of their relation to mortality, the contexts of illness, beliefs about disease causality, and emotions of shame, blame, and fear” (2006, p. X). I like it.
This is not just some by-product of, say, Angelica Thieriot’s Planetree Alliance approach, transformational as that remarkable nonprofit’s 100-plus hospital, strong organization from Derby, Connecticut, has been in the fuss and rattle of the hospital business in America. Rather, the advent and spread of narrative medicine education signal awareness of the consequences of decades of treating patients as life-support systems with many parts, reflecting a century of understanding patient presentations through the limited reductionist lens.
Frankly, NDs have been practicing narrative medicine for aeons. They do not call it that. They believe they are in a professional, personal relationship with their patients. They understand that relationship to be complete with intention, obligation, commitment, and time spent. In the initial intake and well beyond, NDs relate to their patients rather than grill them with questions, assign a test battery, or zip through medical records and findings to advance a diagnosis, refine a prognosis, or interpret data. The insurance companies do not much like the relational approach of the ND because the time it takes is hard to conjugate through a tab of immediately quantifiable outcomes. Charon puts it this way: “. . . practitioners, be they health care professionals to begin with or not, must be prepared to offer the self as a therapeutic instrument” (2006, p. 215). This is a remarkable image and one that I have never heard the American Medical Association repeat at any state legislative hearing I have ever attended (11 so far). Do they know what their members are up to?
When we check out what is actually happening in narrative medicine training, we might be reminded of earlier manifestations of the same effort for building skills for human contact and communication in the healthcare world, such as Tiffany Field’s “therapeutic touch” (established 20 years ago in Florida at the University of Miami School of Medicine) or Wayne Dyer’s intentionality work. Dr. Dyer proclaimed often that a physician’s “intentions” in the “patient transaction” are part of a “force in the universe” to which everyone and everything is connected (Dyer, 2010). There is more afoot here, however. The very fact that narrative medicine is attracting strong and growing interest and that it has become in many cases a desired allopathic medical school skill is a barometer of what has been missing for a long time in biomedicine training. It is so popular now that Columbia University offers a master’s degree in it. In fact, the New York Times gave Columbia University an award for being first to deliver this “much needed” program. A related June 2011 workshop at the university filled to capacity. The next one (October 2011) has a waiting list. Along the continuum of content and interest in narrative medicine, there is Columbia University in America with its master’s degree, and in England there is the University of London, where last June the School of Advanced Study Institute of English Studies held a conference about the use of “comics in medical and public education and their role in health communication and scholarship.” This is fashionable stuff.
Important to note, from the point of view of curriculum design, is that the Columbia University narrative medicine master’s program is recruiting in the humanities and social sciences, positioning their curriculum to “educate a leadership corps of health professionals” who understand the “intimate, interpersonal experiences of the clinical encounter.” They are serious. They want to attract professionals from numerous clinical fields to become “narratively competent clinicians.” They are building “a different kind of caregiver.” They are building a different kind of caregiver team.
Shucks, so are we. In fact, we have been building a different kind of caregiver profession for a century and have had to watch our backs doing it. The wonderful and oh-too-familiar goals of the narrative medicine programs address the phlegmatic rumples in the fierce marketplace of biomedicine delivery. In the literature of orthodox medicine outcomes and practice, we have often seen concerns raised about the fragmentation of the clinical experience, the impersonal nature of bureaucratic decision processes in healthcare choices, and the loss of individuality and autonomy in the patient encounter.
A sampling of the seminar breakout groups in a recent conference organized by Annette Prince, director of the Oklahoma Palliative Care Resource Center and professor at The University of Oklahoma Health Sciences Center, Oklahoma City, tells the tale:
- Psychoanalysis and Narrative Medicine
- The Therapy of Writing: An Analysis of Medical Prose in JAMA
- The Role of Victor Frankl’s Logotherapy in Teaching Narrative Medicine
- “What Story Am I In?” Times Two: Narrative as a Foundation for Active Patient Participation
- A Perspective on the Role of Stories as a Mechanism of Meta-Healing
- What the Children Said, What the Therapist Answered: The Intersubjective Construction of Narrative in Child Treatment
- Autobiography as Psychotherapy: May Sinclair’s Revisionary Dialogue with Early Psychoanalytical Interpretations of Femininity
- The Polyphonic Nature of the Human Psyche: From an Artistic Intuition to a Therapeutic Goal
- Does Talking Cure Leave Only Talk? A Search for the Place of Cure in Psychoanalytic Theory
The narrative medicine initiative has also taken root at the New York–Presbyterian Hospital/Columbia University, where residents such as Dr. Abigail Ford have said publicly: “Narrative medicine changed my entire approach to medicine. As a physician you are really a coauthor of patients’ experiences and need to hear their story and take it on” (Chen, 2008, ). Other residency programs, such as at Vanderbilt University Department of Surgery (Nashville, Tenn.), are following the same path.
Essentially, narrative medicine adds back into the transaction between caregiver and patient the relational, respectful dimensions that biomedicine bleached out of the assembly line of the health business a long time ago. It is a curriculum and communication technique that constitutes what Cooke, Irby, and O’Brien mean when they describe the need for a “synthesis of the cognitive and moral aspects of professional work” (2010, p. ix). Cooke and her colleagues, in the important Carnegie Foundation treatise Educating Physicians: A Call for Reform of Medical School and Residency, take great care to delineate the “poor connections between formal knowledge and experiential learning and inadequate attention to patient populations, health care delivery, and effectiveness” (2010, p. 3). Those “poor connections” manifest not only in settling for a report of disease symptoms at the expense of listening for and hearing about the patient’s life and feelings but also in the steep shift in careers of procedural specialties rather than primary care.
These days, the debate gets stronger about how feelings and belief cannot just be biology in medicine. As Foss puts it, “[H]ow can macroscale phenomena like thoughts and feelings be shown to exert downward causal influence over microscale phenomena like biological processes?” (2002, p. 8). Narrative medicine is the tip of an iceberg in this sea of transformation and challenge about what constitutes “health” and what the physician’s role in it must be. The progress of scientific inquiry itself (in such fields, say, as cybernetics, systems theory, biosemiotics, and information theory) has made it less possible for the allopathic profession (really a subset of biology, according to Foss) to avoid what he calls “loop-structured explanations” about the interconnectedness of things. It is the interest in the need for holism in medicine that, Foss explains, makes more acceptable “self-amplifying upward and downward mutual causation (emergentism), rather than upward causation alone (reductionism)” (2002, p. 8).
Foss translates this into a medical context for us:
“This broadening of heuristic directives to accommodate emergentism and self-organization alongside or in place of reductionism and dualism sets the stage for integrating a biologically-oriented medical architecture into a psychosociobiologically-oriented architecture, for succeeding the prevailing biomedical model and doing so on authentic scientific grounds” (2002, p. 8).
What this means, in turn, is that we are living in a time when a postmodern scientific worldview is being closely scrutinized. It means, to cite Foss one last time, “that macroscale properties like a patient’s mental-emotional states might lawfully be said to influence (not dominate) the internal environment in which disease (and health) grows” (2002, p. 8).
There are so many models of the physician-patient relationship in which narrative medicine can have a place. Surprisingly, over a generation ago, medical sociologists were already sounding warning bells about a broader-based approach to healthcare. As Gregory Weiss and Lynne Lonnquist explain,
“Biomedical medicine is essentially disease-oriented or illness-oriented rather than patient-oriented. The key to effective medical care is believed to be correct diagnosis of some physiological aberration followed by proper application of the curative agent. Consideration of social, psychological, and behavioral dimensions of illness has little place in this framework because it appears unnecessary” (1994, p. 246).
Engel reported 2 decades earlier that “medical students typically have completed their training with little introduction to psychological or social bases for disease and illness or to techniques for managing the physician-patient relationship” (1978, p. X). (cited in Weiss & Lonnquist, 1994, p. 247) even advanced four principles that could convey the physician-patient relationship away from that traditional disease-dependent care model:“1.
The patient is addressed as a whole person, whether or not she or he has a disease. 2.
The doctor-patient relationship is continuous, at all stages of the patient’s life, through sickness and health, until either the physician or the patient dies, moves, or decides to terminate the relationship. 3.
The physician utilizes both biotechnical skills and interpersonal skills to help the patient. 4.
Both the patient and the physician make explicit and then negotiate their respective needs and expectations.”
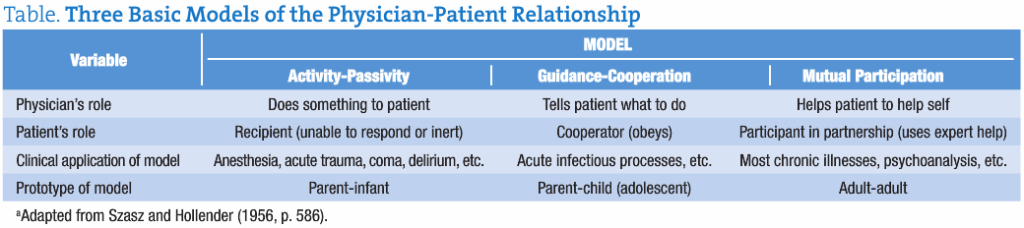
As shown in the Table, the generalized model of physician-patient relationship has many entry points for narrative medicine:
Table. Three Basic Models of the Physician-Patient Relationshipa
Narrative medicine, wherever it lands in the continuum between activity-passivity and mutual participation, is about integrating the patient’s story (complete with his or her values and perceptions) into the clinical application chosen by the physician. Narrative medicine implies an ethical framework within which the physician can suss out more than a report of disease symptoms. Narrative medicine helps link the patient back to the physician in ways biomedicine has discouraged for a long time. Whether it’s the “Parsonian model” of that relationship—with its professional prestige dimension, its situational authority implications, or its situational dependency factors (Weiss & Lonnquist, 1994, p. 243)—or some other modification (e.g., the Szasz-Hollender model [1956, p. 586], reproduced herein, or Robert Veatch’s 1972 model that emphasized the capture of the “moral relationship” between physicians and patients), incorporating patients’ life stories, including their unique underlying value system, into medical treatment options that fit each individual is a very good idea. Even though NDs have been busy doing exactly that forever, we should note that allopathic physicians are paying attention to this essential ingredient in the naturopathic repertoire. The MD is in, getting trained how to talk and listen, and is imitating what NDs have done all along. Triggered though I am these days by the assimilation sorties of biomedicine into natural medicine vistas, I have to admit that imitation has been known to be a sincere form of flattery.
 David Schleich, PhD is president and CEO of NCNM, former president of Truestar Health, and former CEO and president of CCNM, where he served from 1996 to 2003. Previous posts have included appointments as vice president academic of Niagara College, and administrative and teach-ing positions at St. Lawrence College, Swinburne University (Australia) and the University of Alberta. His academic credentials have been earned from the University of Western Ontario (BA), the University of Alberta (MA), Queen’s University (BEd), and the University of Toronto (PhD).
David Schleich, PhD is president and CEO of NCNM, former president of Truestar Health, and former CEO and president of CCNM, where he served from 1996 to 2003. Previous posts have included appointments as vice president academic of Niagara College, and administrative and teach-ing positions at St. Lawrence College, Swinburne University (Australia) and the University of Alberta. His academic credentials have been earned from the University of Western Ontario (BA), the University of Alberta (MA), Queen’s University (BEd), and the University of Toronto (PhD).
References
Charon, R. (2006). Narrative medicine: Honoring the stories of illness. Oxford: Oxford University Press.
Charon, R. (2008). Narrative medicine creates alliance with patients. Retrieved April 22, 2011, from http://www.medscape.com/viewarticle/520704
Chen, P. W. (2008, October 23). Stories in the service of making a better doctor. New York Times. Retrieved June 29, 2011, from http://www.nytimes.com/2008/10/24/health/chen10-23.html
Cooke, M., Irby, D. M., & O’Brien, B. C. (2010). Educating physicians: A call for reform of medical school and residency. San Francisco: Jossey-Bass.
Dyer, W. (2010). The power of intention: Learning to co-create your world your way. New York: Hay House.
Engel, G. L. (1978). The biopsychosocial model and the education health professionals. Annals of the New York Academy of Sciences, 310, 169-181.
Foss, L. (2002). The end of modern medicine: Biomedical science under a microscope. Albany: State University of New York Press.
Roszak, T. (1968). The making of a counter culture: Reflections on the technocratic. Berkeley: University of California Press.
Szasz, T. S., & Hollender, M. H. (1956). The basic models of the doctor-patient relationship. Archives of Internal Medicine, 97, 585-592.
Weiss, G. L., & Lonnquist, L. E. (1994). The sociology of health, healing and illness. Upper Saddle River, NJ: Prentice-Hall.





