A Case Study
Lina Mockus, ND
Introduction
This case study details the naturopathic approach to treating a 58-year-old male patient, Sam, who presented with a history of osteoarthritis (OA) and eczema. OA is an inflammatory disease of the joints that occurs when the protective cartilage that provides a cushion at the ends of bones begins to wear down faster than the body can repair it1. It most commonly affects the knees, hips, spine, and hands.
Eczema is the most common type of dermatitis that causes irritation and inflammation of the skin. It is characterized by rashes or patches of skin that are thick, dry, cracked, itchy, bumpy, and can undergo flare-ups. Because both of these conditions are caused by inflammation due to gut dysbiosis2, the naturopathic treatment aims to address not only the symptoms of pain and inflammation of the joints and skin but also the underlying systemic issues caused by dietary sensitivities and gut health imbalances.
Patient Information
Name: Sam
Age: 58 years old
Gender: Male
Chief Complaints: Chronic knee pain and swelling for 3 years, eczema, pre-diabetes
Current Medications: Tylenol for pain (3-4 times/day before treatment)
Pain Intensity: 7/10, sharp pain exacerbated by running or playing sports
Medical History: OA, eczema, pre-diabetes
Surgical History: Arthroscopic surgery on both knees, 1 year apart
Family History: Type 2 Diabetes (DM2) and OA
Lifestyle: Works full time, stress levels fluctuate but are not excessive; coaches teen sports after work
Patient’s Goals: Reduce knee pain and swelling, improve mobility, decrease muscle stiffness, and resolve eczema
History of Present Illness
Sam presented with a three-year history of progressive knee pain and swelling. Pain levels were rated at 7/10 and were aggrivated by damp weather and physical activity, such as running while coaching sports. Over-the-counter medications (Tylenol) provided temporary relief, but swelling, especially in the lateral distal quads, was slow to recede (over a month). Sam also reported stiffness in his neck, sides, and toes, especially when stretching.
Sam’s eczema had been a persistent issue since the early 2000s, shortly after his diet changed following his immigration to Canada. In his country of origin, his diet was rich in fish and tropical fruit. After moving to Canada, his diet shifted to more red meat and fewer fresh vegetables. This dietary change, alongside other lifestyle factors, seemed to contribute to the gradual onset of his eczema and subsequent diagnosis of pre-diabetes. His diet lacked consistency, and he had difficulty losing weight, a concern linked to his pre-diabetes.
Sam underwent arthroscopic surgery on both knees in 2019 and 2020 to manage his OA. Despite the surgeries, his knees remained inflamed, particularly in humid weather.
Initial Assessment
Sam’s initial presentation included:
- Leg swelling: Most notable in the distal quads, particularly on the left side.
- Eczema: Lesions were present on the lateral lower legs, approximately 20 cm long, with intermittent itching and dryness, worse on the right side.
- Nutritional Deficiencies and Dietary Sensitivities: Sam’s diet was inconsistent and lacked essential nutrients. He frequently consumed red meat and processed foods but ate little fish or vegetables, both critical in managing inflammation. He also had a known lactose intolerance and possible celiac disease, exacerbating his gut health issues.
- Stiffness and Muscular Imbalances: Sam had noted stiffness in his neck, sides, and toes, which likely contributed to biomechanical issues in the lower body, aggravating his knee pain.
Given the complexity of Sam’s symptoms, the naturopathic treatment aimed to address his pain, inflammation, and nutritional imbalances.
Naturopathic Approach and Treatment Plan
A comprehensive naturopathic plan was developed, addressing Sam’s chief complaints while considering his gut health, inflammation, and musculoskeletal health.
- Dietary Modifications
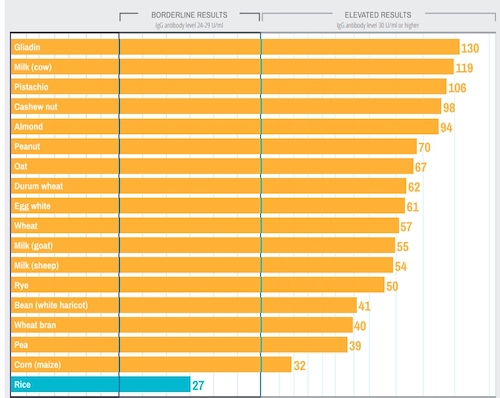
- Gluten-Free Diet: Sam was advised to do an IgG food sensitivity test. Based on the results (Figure 1), Sam was advised to eliminate gluten due to suspected celiac disease (3).
- Fish Oil: Sam was prescribed 1 tsp of fish oil daily to mitigate systemic inflammation and to increase his consumption of omega-3 fatty acids, which declined after his move to Canada due the changes in his diet. He later opted for fish oil capsules for convenience.
- Botanical and Nutritional Supplements
- Curcumin: 1 capsule daily to reduce systemic inflammation.
- Vitamin D3/K2/A: 1 drop daily with food to support immune function, skin, and joint health4.
- Magnesium Bisglycinate: 400 mg daily to reduce muscle stiffness and improve sleep quality.
- Boswellia serrata: Introduced because it is used traditionally to manage OA symptoms by reducing joint inflammation5.
- Physical Therapy and Acupuncture
Electro-acupuncture: Sam received acupuncture treatment during each visit, focusing on knee pain and systemic deficiencies in the stomach (ST), large intestine (LI), and spleen (SP) channels. Points needled were LI4, ST33, Xijan, ST35, and SP10 to reduce knee pain and inflammation and to restore gut health. Magnesium gel was applied post-treatment to reduce swelling and hypertonicity in distal quads.
- Lifestyle and Stress Management
Sleep Improvement: Sam was advised to try 5-HTP for sleep but discontinued it due to feeling “funny.” Despite this, his sleep improved, reporting an increase in average sleep to 6-6.5 hours per night, up from 4-5.5 hours per night.
Physical Activity: Sam was encouraged to continue coaching sports and performing physical therapy exercises to strengthen his left knee and reduce compensation by the right knee.
Gut Health: Sam was prescribed a supplement consisting of demulcent herbs to help heal his gut lining and restore his microbiome.
Follow-Up and Outcome
- Second Visit (3 weeks later):
Sam reported significant improvements in his eczema, noting that the lesions were less itchy, smoother, and not spreading. However, there was no noticeable change in knee pain at this stage, and he continued taking Tylenol 3-4 times per day. Sam started eliminating gluten from his diet after this visit and continued with his supplements. - Third Visit (1 week later):
Sam’s knee pain had lessened to the point where he only took Tylenol once the previous week. He noted a reduction in leg swelling and felt an overall improvement in mood, as reported by his family. Sam had completely eliminated gluten from his diet and was eating more fruit and vegetables. His eczema lesions were slightly smaller and smoother. - Fourth Visit (1 week later):
Sam had stopped taking Tylenol altogether and reported continued improvement in knee swelling. Although the eczema persisted, the lesions continued to shrink slowly. Sam remained optimistic about his progress and adhered to his supplement regimen.
Fifth Visit (3 weeks later):
By the fifth visit, Sam no longer experienced knee pain and had not taken Tylenol for pain relief. He noticed significant improvements in his eczema, with lesions becoming lighter and smaller. Sam also reported better energy levels and significantly reduced reliance on coffee in the morning for energy.
Discussion
This case highlights the benefits of an integrated naturopathic approach to managing chronic knee pain, eczema, and dietary sensitivities. Through dietary modifications, acupuncture, supplements, and lifestyle adjustments, Sam experienced significant improvements in both his knee pain and eczema. His ability to discontinue pain medication, alongside the visible reduction in swelling and inflammation in his legs as well as itching and lesion size on his skin, emphasizes the efficacy of this approach.
Conclusion
The naturopathic treatment successfully addressed both the symptomatic pain and systemic inflammation associated with Sam’s OA and eczema. This case demonstrates the importance of a holistic, individualized treatment plan that includes food sensitivity testing, dietary changes, supplementation, and physical therapy for managing complex, chronic conditions.

Lina Mockus is a naturopathic doctor licensed to practice in Ontario. She divides her time between Toronto and Goderich, Ontario. Her areas of special interest are pain management, mental health, women’s health, and digestive health.
References
- Knights AJ, Redding SJ, Maerz T. Inflammation in osteoarthritis: the latest progress and ongoing challenges. Current Opinion in Rheumatology. 2023; 35(2):128-134.
- Zeng MY, Inohara N, Nuñez G. Mechanisms of inflammation-driven bacterial dysbiosis in the gut. Mucosal Immunology. 2017; 10: 18–26.
- Finn R, Harvey MM, Johnson PM, et al. Serum IgG antibodies to gliadin and other dietary antigens in adults with atopic eczema. Clinical and Experimental Dermatology. 1985;10(3):222–228.
- Kim MJ, Kim SN, Lee YW, et al. Vitamin D Status and Efficacy of Vitamin D Supplementation in Atopic Dermatitis: A Systematic Review and Meta-Analysis. Nutrients. 2016; 8(12):789.
- Ganpeng Y, Wang X, Tianqing Z, et al. Effectiveness of Boswellia and Boswellia extract for osteoarthritis patients: a systematic review and meta-analysis. BMC Complement Medicine and Therapies. 2020; 20(1):225.

