Phranq D. Tamburri, NMD
It seems that every 6 months during the past 3 years a different health organization has announced new guidelines for the screening of cancer of the prostate (CaP). Screening refers primarily to a 30-year-old blood test called the prostate-specific antigen (PSA) and to palpation of the prostate known as the digital rectal examination. Each new volley recommendation to curtail PSA screening has typically been met by a contradictory call to screen even more. In late June 2012, this debate had crescendoed with the federal government’s highest medical opinion group, the US Preventive Services Task Force (USPSTF),1 stating that CaP screening is now not needed, regardless of age. This response was deafening to the CaP community in its influence and as a traumatic hit to the proscreening groups. For this reason, the integrative medical community must be aware of this seismic medical shift.
Quick History
Over the course of the prior decade, these 2 polar views on PSA screening (to screen or not to screen) have each attempted to woo the federal government’s opinion toward their side. A decade ago, questioning the PSA efficacy was considered heretical and “quackery” by all mainstream cancer organizations; hence, the USPSTF always supported the standard CaP screen. However, through the years the antiscreening viewpoint has grown with more evidence and has found cautious but supporting new endorsements by converting organizations such as the American Cancer Society and the Prostate Cancer Research Institute. Yet, the official view of the USPSTF had still been to support the old screening standards. However, after years of consistent data on the overall negative effects of standard screening during a time of upheaval in the current medical system (as insurance reimbursements worsen and as the Patient Protection and Affordable Care Act looms to take effect), the USPSTF finally changed their decision on the matter. The effect of having the federal government take this surprising step of reversing their stance to support the radical antiscreen movement has signaled the beginning of the end for the basic CaP prevention screen and the single PSA blood test.
The following is the official response from the USPSTF1:
In October 2011, the USPSTF posted for public comment the draft of its recommendation regarding prostate cancer screening. Since then, Task Force members have read the many comments received and reviewed the most up-to-date evidence.
Based on this work, the Task Force concludes that many men are harmed as a result of prostate cancer screening and few, if any, benefit.
A better test and better treatment options are needed. Until these are available, the USPSTF has recommended against screening for prostate cancer.
The members of the USPSTF face the same concerns and fears about health challenges as other people. This decision was reached only after extensive consideration and thoughtful debate. It is based on science and rooted in the knowledge that while everyone wants to help prevent deaths from prostate cancer, current methods of PSA screening and treatment of screen-detected cancer are not the answer.
Furthermore, USPSTF cochair Michael LeFevre, MD, MSPH, issued the following statement on May 22, 2012: “Prostate cancer is a serious health problem that affects thousands of men and their families. But before getting a PSA test, all men deserve to know what the science tells us about PSA screening: there is a very small potential benefit and significant potential harms. We encourage clinicians to consider this evidence and not screen their patients with a PSA test unless the individual being screened understands what is known about PSA screening and makes the personal decision that even a small possibility of benefit outweighs the known risk of harms.”1
PSA Controversy Synopsis (The Underlying Cause)
The central debate on CaP screening is as follows: although CaP kills many men per year, most of these diagnosed CaP cases are not fatal. Statistically, with the mean age at diagnosis being 67 years, comparing the mortality of all men with CaP and of all CaP stages (indolent to metastatic), the relative survival rates are 100% at 5 years, 98% at 10 years, and 91% at 15 years.2
Most diagnosed CaP is discovered not due to any symptoms caused by the disease but instead owing to an elevated PSA primarily from an enlarged prostate, prostate inflammation, or both. The latter have been determined to be the most common reasons that “fool” the PSA to become slightly elevated (>2 but <10 ng/mL). Therefore, because of the added pressure of lawsuits against physicians for not discovering a cancer, when a PSA rises above 3 or 4 ng/mL, a reflex biopsy is performed. This has resulted in an explosion of CaP diagnoses since the early 1980s due to the use of the PSA screen. Although cancer is being diagnosed, statistically speaking the CaP discovered is of the common nonlethal form (indolent CaP).
This CaP diagnosis would not be as controversial if the treatment resulted in a simple scar. However, CaP treatment typically consists of destruction or removal of the entire prostate gland. This invasive surgery, more often than not, results in life-altering adverse effects such as incontinence or erectile dysfunction. Therefore, the end result of the current state of CaP screening is as follows: a blood test meant to save men’s lives has led to an overdiagnosis of a typically nonlethal cancer because of lawsuit fears, which ultimately leads to serious quality-of-life adverse effects that (from many patients’ perspectives) were for no medically legitimate reason.
Where Does the USPSTF Recommendation Leave the Integrative Physician?
The obvious and immediate question that physicians face is “Now what? What am I supposed to do to rule out CaP?” Most important, “Can I still be held legally accountable if I do not conduct CaP screening?” The answers to these questions are still evolving monthly at this time and will be better illuminated in the coming years as urologic-focused physicians and their progressive urologist brethren detangle this knotted issue.
To yield some insight into this screening quandary, my urologist colleagues (here in the great “Cowboy” state of Arizona) have often equated the PSA to a loaded firearm. If you do not know how to use one, then never touch it. It is harmful to both yourself and others. However, if you have proper training in the use and laws surrounding proper operation of a firearm, then you can be a safe owner. Dismissing any political overtones with this analogy, the PSA is a loaded number. By itself, with no further context (PSA velocity, PSA density, PSA pattern, etc), the PSA will trigger the current medical system into an unnecessary biopsy and then likely an unnecessary surgery, resulting in unwarranted permanent adverse effects. However, with proper training on the use of the PSA, this blood test can still be a valuable tool when used in conjunction with other qualitative factors. This aggregate assessment approach toward CaP diagnosis is precisely what the various CaP organizations have called for on how to properly use the PSA screen in context. Without these assessment modifiers and if the PSA is simply used as a snapshot value, then the current common denominator advice for physicians is to avoid the CaP screen altogether.
In the near future, litigation cases might ensue if a patient is diagnosed as having a metastatic CaP without undergoing a previously accepted proactive CaP screen. Such a liability will likely be first focused on the allopathic medical system and their liability structures; however, now with the endorsement of the USPSTF to avoid screening, liability concerns (especially for NDs) will likely become significantly reduced.
What Newer Options Are Available for Advanced CaP Screening?
Looking toward the next horizon of better CaP tests, no consensus has been reached on a truly reliable primary test screen. Instead, we have discovered more qualitative tests that provide data to better complete the larger aggregate CaP risk picture. The most heralded at this time are transrectal ultrasonography of the prostate (TRUSP) with power color Doppler and modern 3-T endorectal magnetic resonance (MR) imaging. Prostate cancer antigen 3 (PSA3) and galectin-3 are also discussed in this section.
TRUSP With Power Color Doppler
Although TRUSP with power color Doppler was highlighted in the 2007 NDNR men’s health issue, it has become ever more in demand as a low-invasive technique to image not only a potential CaP in real time but also to record the overall patterns and health of the gland. This technique (one that following full disclosure and informed consent is performed at my office daily) not only can help identify a neoplasm but also is the technique best suited to determine other prostate pathology (prostatitis and benign prostatic hyperplasia). Determining the presence and effect of other pathology is crucial to help rule out the true effect of CaP on the PSA kinetics. This is obviously important when confronting the fact that most elevated PSA is from non-CaP causes.
Modern 3-T Endorectal MR Imaging
Similar to TRUSP with power color Doppler, modern 3-T endorectal MR imaging is a reasonably accurate, but not perfect, method for detecting a prominent CaP. Patients are routinely hearing about this “new” MR imaging or, more specifically, an endorectal or “rectal coil” MR imaging. As appealing as MR imaging has recently become, be aware that the current gold standard for imaging of suspected CaP is the use of endorectal MR imaging with the newer (and more expensive) modern 3-T unit. Currently, only a handful of imaging centers nationwide provide this specific use of the machine and have a radiologist trained in the new practice of CaP MR imaging.
Which Is Better? TRUSP With Power Color Doppler or Modern 3-T Endorectal MR Imaging?
The modern 3-T endorectal MR imaging technique yields many benefits over TRUSP with power color Doppler in detail resolution, including better visualization of irregular margins and potential extracapsular extensions that could lead to a metastasis. However, the disadvantage is that it only provides a quantitative snapshot image compared with the real-time imaging of TRUSP that relates qualitative imaging data. TRUSP with power color Doppler is exceptional in observing suspected CaP within the context of the health of the prostate and compared with other pathology. In general, MR imaging is best served when a CaP has significantly worsened or if early metastasis is suspected. It can also best give slightly more accurate suspected CaP dimensions because of the higher resolution. TRUSP with power color Doppler is far better at assessing an overall baseline for a suspected CaP and for determining other pathology associated with PSA, and it is cheaper to use on a regular basis. Therefore, TRUSP is superior for ongoing active surveillance of patients and in determining the efficacy of treatments.
Prostate Cancer Antigen 3
The fairly new PCA3 test was discussed in the November 2008 issue of NDNR; however, it has recently become much more well known by physicians and even requested by patients. The PCA3 test has represented one-third of my entire assessment approach for more than 5 years, yet it is still sometimes either unknown or discounted. It is important that physicians recognize the history and current use of this examination. Although earlier the test had limited use by only a few progressive urologists and NDs, the test began to gain Food and Drug Administration approval in late 2011. The approval of the PCA3 (and hence its linked insurance coverage), coupled with the recent recommendations dissociating the PSA as a primary screening tool, has finally established this test as a mainstream alternative option to the PSA. The only concern about this early support is that, with many patients and physicians not yet well versed on the meaning of the PCA3 results, this test can be questionable in its use when interpreting the CaP aggression risk.
In addition, numerous laboratories have suddenly begun offering the PCA3 test to compete with its sudden post-PSA popularity. Although I have personally not compared laboratory results for PCA3 consistency and accuracy, any new test with various interpretations should be used with caution, especially if the PCA3 test comes from a laboratory that newly offers it. Until enough comparison data from other laboratories are available, I am only using the allopathic urology specialist laboratory that first brought the PCA3 to the United States more than 7 years ago.
Nevertheless, more data overall are needed to better vet the PCA3 test as a primary screening tool. As it exists currently, it is an integral part of a comprehensive CaP assessment.
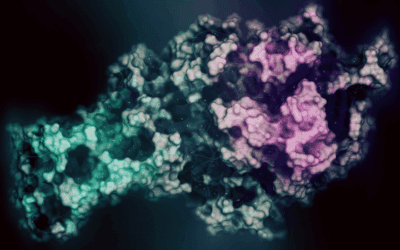
Galectin-3
Galectin-3 is within the protein category known as galectins and binds by carbohydrate-recognition domains to certain carbohydrates. Galectins also interact with certain cell surface receptors and extracellular receptors. Therefore, they have an important role in disease mechanisms and intracellular pathways. The galectin-3 test has been primarily used as a marker for heart failure by signaling cardiac remodeling and inflammation.3 However, recent evidence suggests that galectin-3 is elevated in patients with certain advanced cancers, including CaP.4 It has been found to be essential in cell growth, adhesion, differentiation, angiogenesis, and apoptosis, yet for some tumors (such as CaP) the expression of galectin-3 is inversely correlated with metastatic potential.4 Although this early and experimental use of galectin-3 should be interpreted with caution, it is promising as part of the armamentarium in an aggregate assessment approach to CaP screening.
Aggregate Assessment Strategy and Patient Education
Completing these post-PSA screening suggestions brings us back to the most accurate screening tool available, the aggregate assessment. The bottom line is that, with more data available on a patient’s prostate health, a better risk determination can be made regarding his CaP and its potential to be of an indolent variant. As stated earlier, the PSA test is not a poor test method if used in tandem with multiple data points and in conjunction with other qualitative CaP assessment data.
A quick summary list of indicators to consider when assessing a potential CaP includes the following: PSA total, percentage free PSA, PSA density, PSA pattern, PSA velocity, American Urological Association Symptom Score, urinalysis, digital rectal examination, prostatic acid phosphatase, complexed PSA, PCA3, and biopsy report, if performed, all preceded by a complete urinary, family, and chemical history. Further details on CaP aggregate assessment can be found in prior NDNR men’s health issues from September 2007, November 2008, and November 2009.
Conclusion
Regardless of how the physician uses the PSA to rule out CaP, the most important point is that both the advised assessment strategy and the PSA debate concerns are discussed with the patient, who must participate in the decision making and understand the screening concerns. Although this concept of educating patients is not novel for NDs, it is precisely what is needed to protect the patient from the risks of CaP metastasis and unnecessary surgery and to guard the physician from liability concerns until a more accurate screen is determined.
 Phranq Tamburri, NMD graduated from SCNM in 2001. He has since earned recognition as an expert in the field of prostate cancer assessment, diagnosis and treatment utilizing a balanced natural and allopathic perspective. His urology experience was earned as SCNM chief resident under Tom Kruzel, ND, and through ongoing rotations with Mayo-trained urologist Bernard Gburek, MD at Kapner and Associates, Scottsdale North Hospital. Currently, Dr. Tamburri sits as the only ND Board Member on the AZ State Supported Southwest Prostate Cancer Awareness Council. He is also head professor of clinical urology at SCNM, and is a contributing author to the upcoming Foundations of Naturopathic Medicinetextbook. He practices with an international patient clientele at Naturopathic Family Care in Phoenix.
Phranq Tamburri, NMD graduated from SCNM in 2001. He has since earned recognition as an expert in the field of prostate cancer assessment, diagnosis and treatment utilizing a balanced natural and allopathic perspective. His urology experience was earned as SCNM chief resident under Tom Kruzel, ND, and through ongoing rotations with Mayo-trained urologist Bernard Gburek, MD at Kapner and Associates, Scottsdale North Hospital. Currently, Dr. Tamburri sits as the only ND Board Member on the AZ State Supported Southwest Prostate Cancer Awareness Council. He is also head professor of clinical urology at SCNM, and is a contributing author to the upcoming Foundations of Naturopathic Medicinetextbook. He practices with an international patient clientele at Naturopathic Family Care in Phoenix.
References
- US Preventive Services Task Force. Screening for prostate cancer. http://www.uspreventiveservicestaskforce.org/prostatecancerscreening.htm. Accessed September 19, 2012.
- American Cancer Society. Prostate cancer. February 2012. http://www.cancer.org/Cancer/ProstateCancer/DetailedGuide/prostate-cancer-survival-rates. Accessed September 19, 2012.
- Lok DJ, Van Der Meer P, de la Porte PW, et al. Prognostic value of galectin-3, a novel marker of fibrosis, in patients with chronic heart failure: data from the DEAL-HF study. Clin Res Cardiol. 2010;99(5):323-328.
- Takenaka Y, Fukumori T, Raz A. Galectin-3 and metastasis. Glycoconjugate J. 2004;19:543-549.