Complex Chronic Disease Saved by a Genetic Hormone Profile
WINNIE SIU, ND
As clinicians, we often come across complex and challenging cases. Many of our patients have been diagnosed with complex chronic conditions such as mast cell activation syndrome (MCAS), chronic fatigue syndrome (CFS), multiple chemical sensitivity (MCS), and fibromyalgia (FM). The Statistics Canada 2005 Canadian Community Health Survey found that 1.2 million Canadians, or 5% of those aged 12 or older, reported having been diagnosed with at least CFS, MCS, or FM.1 These patients usually have been sick for several years and have seen and continue to see multiple health care professionals, including medical doctors, specialists, and integrative and alternative medicine practitioners. When patients are referred for environmental medicine assessments, their symptoms often indicate that many body systems are involved, resulting in immunotoxicity, immune dysregulation, hormone imbalance, and neurotoxicity.2,3 These cases are challenging as patient symptoms are numerous and vary extensively.
From clinical experience, both day to day low-level and significant single-dose exposures contribute to a patient’s total body burden: the total load of toxins and toxicants in our bodies that cause multi-system symptoms. The total body burden must be considered when assessing the underlying cause of a patient’s symptoms. Toxins and toxicants assessed should include both endogenous biological compounds and exogenous chemicals, including medications and exogenous hormones.
Hormone therapy is increasingly used to help patients with endocrine health issues. Though many patients benefit from hormone therapy, not all do, and doctors have the responsibility to identify those who may be harmed by it. Understanding a patient’s underlying functional genomic makeup may help individualize hormone prescription or usage and prevent it from adding to the total body burden.
The case report presented below shows how symptoms of MCAS and MCS can result from improper prescribing of hormones, especially in an estrogen-dominant female with poor hormone clearance and a complex and extensive medical history. This report highlights that prescribing progesterone to address estrogen dominance is not always suitable, especially in patients with more complicated health conditions. The complementary use of functional genomics and urinary hormone metabolite testing can provide insights into analyzing suitability.
Case Presentation
A 21-year-old woman presented to our clinic with severe allergic reactions; anaphylaxis to scented products, histamine foods, and solvents; temperature dysregulation; and hot flashes. She had been diagnosed with MCAS, MCS, FM, and CFS. She was managed by multiple medical doctors, including an allergist, immunologist, psychiatrist, neurologist, and a family doctor. Though she was taking pharmaceutical and natural antihistamine medications, they were proving ineffective at reducing her allergic symptoms or tolerance.
She had an extensive medical history and had not felt well since she was 14 years of age. At that point in time, she started to experience anxiety, depression, and sinus issues. She also reported significant GI Candida albicans overgrowth (for which she had received treatment from her ND for many years). In her teenage years, she progressively got worse. From the ages of 17 to 19, she had panic attacks and regularly went to the hospital for severe pain and fainting episodes. She also received allergy shots during this period of her life. Then, from the ages of 19 to 21, her treatments (dietary changes and supplements) focused on addressing Candida; though lab tests afterward confirmed resolution of Candida, she still did not feel well. She tested positive for small intestinal bacterial overgrowth and was treated with rifaximin; this too resulted in no change in symptoms.
Significantly, her MCAS symptoms would always flare 2-3 days before her menstrual cycle. A urinary hormone metabolite lab test revealed low progesterone and testosterone, and high estrone, estradiol, and the estrogen metabolites 4-hydroxyestrone (4-OHE) and 16-hydroxyestrone (16-OHE). During the following year, she reported that all her symptoms got worse, and her severe allergic and anaphylaxis reactions started. Additionally, her chronic fatigue became so extreme that she had to be in a wheelchair for any activity that required considerable exertion.
Before this patient started progesterone replacement in the form of a topical cream, she had experienced amenorrhea for 6 months. She also had a very strong family history of polycystic ovary syndrome (PCOS). She herself did not have PCOS, though this was suspected at some point.
We completed an environmental assessment and history in the office and established that there were no major significant environmental exposures to pesticides, heavy metals, smoke, polychlorinated biphenyls, mold, solvents, or volatile organic compounds. In addition, we ran a functional genomics hormone panel to see if this patient’s genetic profile could explain her symptoms – not just reactions to scented products, histamine foods, and solvents. We suspected that the progesterone cream was aggravating the patient’s MCS, MCAS, immune reactivity and anaphylactic reactions.
Hormone Profile Findings
The results of the patient’s genetic hormone profile established several issues contributing to her symptom picture. For example, she exhibited genetic predispositions to suboptimal methylation, glutathionization, and glucuronidation. However, most significantly, her profile indicated that she was estrogen dominant and was prone to a slow clearance of estrogen metabolites and androgens. Her combination of a fast cytochrome P450 17A1 (CYP17A1) and moderately fast CYP19A1 (aromatase) resulted in an overall fast conversion of progesterone to estrogen. This resulted in low levels of progesterone and high levels of estrogen. Prescribing progesterone to help balance the high estrogen resulted in shunting of the progesterone, increasing both estrogen and estrogen metabolites.
The estrogen metabolites 4-OHE and 16-OHE are highly inflammatory; their presence is linked with MCS and other conditions that exhibit immunotoxic effects.4 Therefore, by adding even more “fuel to the fire,” the increase of progesterone potentially ended up downstream, resulting in significant inflammation based in high levels of harmful estrogen metabolites. This flared her pre-existing MCS/MCAS condition to the point that she was experiencing potentially anaphylactic reactions to allergens she had never reacted to before.
Treatment Plan
- Discontinue progesterone. Purpose: eliminate the cause and aggravation of symptoms.
- Liposomal glutathione – 400 mg in the morning on an empty stomach. Purpose: support phase 2 detoxification.
- Phase 2 detoxification nutrient support blend (B vitamins, vitamin C, magnesium, manganese, selenium, zinc, Silybum marianum, and N-acetylcysteine) – 1 teaspoon in the morning. Purpose: support phase 2 detoxification.
- Colon hydrotherapy – 2 times per week for 3 weeks. Purpose: bring down total body burden. (Note: this was limited by the patient’s schedule)
- Reduce as many everyday environmental exposures / total body burden stressors as possible.
Follow-up
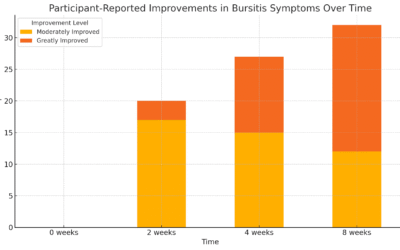
The patient followed the treatment plan for 2.5 months. Upon follow-up, she reported a major improvement in allergic and anaphylactic symptoms. She felt great for the first time in a long time, with almost no reactions to food when eating out at restaurants; she had been unable to do this over the previous year. MCS reactivity was also significantly reduced but not fully resolved.
Conclusion
This case study serves as a reminder of how a person’s genomic hormone profile can lead to significant clinical outcomes. Environmental toxins and toxicants such as hormone disruptors, neurotoxins, and immunotoxins are not the only potential risks to our patients. Doctors also need to thoroughly assess whether exogenous prescription hormones are provoking reactions in our patients.
As clinicians, we need to utilize tools that help us differentiate patient cases and not fall into the trap of using non-specific protocols only. Not all estrogen dominance is suitable for treatment with progesterone therapy, especially for patients with an extensive medical history and complex chronic conditions. Improper use of hormone therapy can result in a symptom profile that presents like MCS and MCAS.
References:
- Lavergne MR, Cole DC, Kerr K, Marshall LM. Functional impairment in chronic fatigue syndrome, fibromyalgia, and multiple chemical sensitivity. Can Fam Physician. 2010;56(2):e57-e65.
- Crinnion WJ, Pizzorno JE. Clinical Environmental Medicine. St. Louis, MO: Elsevier Health Science; 2019.
- National Report on Human Exposure to Environmental Chemicals. Centers for Disease Control and Prevention. https://www.cdc.gov/exposurereport/index.html. Published April 12, 2022. Accessed July 23, 2022.
- Straub RH. The complex role of estrogens in inflammation. Endocr Rev. 2007;28(5):521-574.

Winnie Siu, ND, graduated from Canadian College of Naturopathic Medicine and is a licensed naturopathic doctor. She is the clinical director for The DNA Company, a Canadian-based functional genomics testing company. Dr Siu cofounded (with her husband Aviad Elgez, ND) the EnviroMed Clinic in Toronto, Canada, focused on caring for patients with environmental illnesses. She takes an active stance on educating the public about the ill effects of toxic chemicals in our food, water, body care, cosmetics, and household products. In her spare time, she enjoys leisure reading and going for adventures in nature with her husband locally and internationally.