Tolle Causam
Hal Brown, ND, DC, RAc
“Maybe I should find another doctor; one who realizes the importance of scars.”
(Rasmenia Massoud, Human Detritus)
Over 20 years ago I attended an IV course taught by Dr Garrett Swetlikoff, which concluded with an introduction to neural therapy. At the time, injecting a scar with procaine did not make sense to me. As is often the case, what we learn on Sunday we put into practice on Monday. That next day, a longstanding 65-year-old female patient presented complaining of sudden onset agonizing upper thoracic pain. For the next two days I treated her with limited success. When she returned on Wednesday, she mentioned through tears that she had not been able to stand straight since a surgery 10 years prior that had left a wide scar from navel to xyphoid process. Not understanding the significance of this history, I had previously discounted it. Now, having just attended the IV course and not knowing what else to do, I suggested injecting the scar. After the treatment the patient felt significant relief. A few weeks later she reported that she had rejoined a choir and was able to resume singing, a passion she had quit following the surgery, due to abdominal tension. Realizing there was something to this, I enrolled in the next neural therapy course, taught by Dr Dietrich Klinghardt. A new and exciting phase in my practice began.
What we experienced that day was sekundenphaenomen (also known as a “lightening reaction” or “Huneke phenomenon”). The Huneke brothers practiced in Germany from 1925 to 1940. A female patient with 5 years of chronic right shoulder pain consulted them. She was unable to get relief with any treatment until a 35-year-old scar on her left shin from osteomyelitis surgery had suddenly become inflamed and painful and she sought help. One of the brothers injected the scar with procaine. As expected, the local scar pain was relieved; however, as legend has it, the shoulder pain also subsided within 5 seconds. This surprising response was dubbed a “Huneke phenomenon.”1(p46)
Dysfunction of Scar Tissue
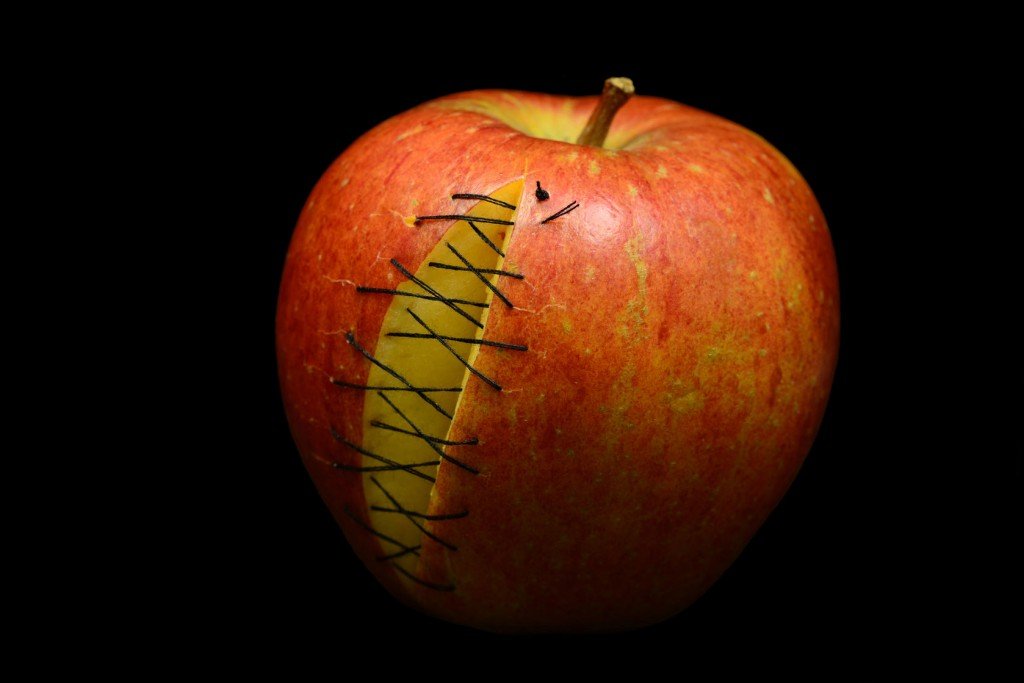
Scar tissue constitutes a natural repair by the body of a wound or cut with dense, fibrous connective tissue. Wounds heal with collagen that has inferior functional quality compared to normal tissue.2 During scar formation, adhesions attach to deeper sliding structures, such as tendons, muscles, fascia and, viscera. French plastic surgeon, Dr Jean-Claude Guimberteau, created an excellent video of scars and adhesions observed during surgeries.3 Among the many fascinating clips, he shows an adhesion from a skin scar attaching and restricting the sliding motion of a tendon. Another clip shows ovarian adhesions from a C-section scar.
In addition to restricting motion, a scar interferes with normal physiological exchange between the connected sides. Nerves, blood and lymphatic vessels, meridians, skin, fascia, and other tissues cease to connect or communicate normally across the scar barrier. The temperature of a scar varies ±2 OC, and the electrical resistance has been found to be as much as 10 times higher than normal skin.1,4 A scar may be a direct pain generator when cutaneous and subcutaneous nerves are cut along with skin and deeper tissues; neuromas, nerve entrapment, or inflammatory mediators in scars can also produce pain.5
The transmission of tension from one area of the body to another through the fascia planes is referred to as “fascial drag.” Upledger and Vredevoogd (1983)6 give an example of a patient with chronic migraines produced by an appendectomy scar. When the scar was pressed deeply medially, the headache was reproduced. When the scar was pressed laterally, the headache was relieved.7
The Scar Tissue Interference Field in Neural Therapy
In neural therapy there is the concept of an interference field, or dominant focus, whereby a local disturbance may cause symptoms in unrelated and perhaps distal sites. Common foci may occur in teeth, tonsils, autonomic ganglia and viscera or may be due to subclinical infections. Scars are considered to be very significant interference fields.1,4,8,9
When skin is cut as a result of injury or surgery, so are densely packed sympathetic nerve fibers. These nerves may heal poorly, disrupting the overall function of the autonomic nervous system. Signals may be transmitted improperly or nerves may join in an aberrant fashion. Louisa Williams, ND, describes this condition as “chaotic and noisy sympathetic nerve activity in a scar.”8 According to Williams,8 neurologist Dr Hooshang Hooshmand refers to this as an “island of turbulence” in the scar area.10
Clinical Assessment of Scars
An assessment begins with a thorough case history and inquiry into all surgeries and traumas and their chronology. A physical examination should note every scar, even in areas remote from the chief complaint, as a possible disturbance site or adhesive dysfunction. This includes obvious scars from injuries and surgeries but also tiny laparoscopic or arthroscopic scars. Any scar should be suspect and no scar is too small or insignificant to consider. A commonly overlooked area is perineal scars from episiotomy and tearing from childbirth.
The methods of identifying physiologically disturbed scars are varied. Obviously, any that are painful, itchy, or clearly interfering with movement, such as post-mastectomy scars, require treatment. A non-tender scar may still be a focus. Note any abnormal thickening, tenderness, ticklishness, temperature changes, or texture of the skin.4 The textbook Naturopathic Physical Medicine (2008)7 describes deep palpation near the scar to feel for increased resistance and lack of “end feel.” It is suggested to get a feel for the tethering or floating of the tissue and to observe whether the scar can be moved equally in all directions.7 Palpation of tender spots, or small neuromas, or other tissue changes may help to isolate specific sites that require treatment.
Although highly subjective and controversial, Drs Klinghardt,9 Williams,8(p425) and Kidd4(p38) recommend Autonomic Response Testing as a useful tool. Electrodermal testing is another method that may reveal scar foci.11
Ultimately, it is one’s clinical judgement based on listening to the patient, case history and physical examination that leads to the correct assessment.
Methods of Scar Treatment
Most physical medicine disciplines recognize the importance of treating scar tissue, either as direct or indirect causes of pain. Some examples:
- Acupuncture techniques manipulate scar tissue.12
- Myofascial methods utilize a variety of manual tissue manipulation techniques to treat fascial drag and skin adhesions.13,14
- Cyriax JH developed cross-friction technique as a method of treating scar tissue.15
- Neural prolotherapy involves injections of 5% dextrose and 5% mannitol.16
- Topical treatments of scar include: silicone gel, polyurethane dressing, onion extract, and vitamins A and E creams,17 essential oils, wheat germ and sesame oil.9
- Cosmetically, steroid injections are used to lessen keloid, hypertrophic and unsightly scars.18
- Steroids are used to reduce post-surgical itching, contracture, and pain in scars.18
- Surgical resection of scars is common,19 as is laser and other light treatment.20
- Injections of alcohol into tender points in surgical scars have been found effective at relieving pain.21
- IV Glutathione can enhance the effects of manual therapy.21
Treatment of Scars with Neural Therapy
Clearly, there are many effective methods for treating scar tissue. One might question whether the beneficial effect comes from the anesthetic injection into a scar or the aponeurotomy effect of a needle breaking up adhesions. Lacking clearer evidence, I speculate that each treatment involves various degrees of both a neural and a biomechanical effect.
A scar is a chaotic neural phenomenon, with a sympathetic-dominant charge firing in a disturbed “fight or flight” manner. The intention of a neural therapy injection is to alter the autonomic nerve conduction that creates the disturbance by normalizing the membrane potential. When procaine is injected into a nerve, anesthesia occurs due to temporary hyperpolarization4 (fig3-1, p39) (inhibition). When the anesthetic wears off, the nerve repolarizes with a now-normal membrane potential. I often explain to my patients that this is like having an irritatingly slow and erratic computer: the solution we all know is to reboot, and upon starting, it now works fine. Neural therapy treatment might be regarded as an “autonomic reboot”.
The following treatment procedures are based on Dr Klinghardt’s instructions.9 A syringe is drawn up with a 1% procaine solution. Homeopathic injectables are a common addition, the selection depending on the case. For most scars, a 25-guage, 1 ½” needle is used. For smaller scars, a 27-guage, 1 ¼” needle may suffice. Using the sterile cap, the needle is bent to an almost 90-degree curve. The skin is stretched with one hand and a cutaneous injection is made. The entry should not be deep; the intention is to see the surface of the scar rise and the local anesthetic infiltrate the adjacent portion of the healthy skin. Even small cross-stitches should be injected. After injection, the gliding function of the tissues beneath the scar should be assessed manually. Wherever there is restriction the needle is inserted perpendicularly and deeper adhesion is infiltrated. The scar is then manually mobilized to detach it from underlying tissue. It is also suggested to have the patient massage wheat germ oil and manipulate the scar daily for a month. I have posted a demonstration online of a scar injection.23
Training in Neural Therapy
Dr Dietrich Klinghardt originally introduced neural therapy to North America and still teaches through the Klinghardt Academy. Other excellent instructors are Jeff Harris, ND, in Seattle and Robert Kidd, MD, in Ontario, Canada.
My 39 year-old-patient’s own words and experience illustrate the importance of identifying scar tissue as a causal factor in chronic pain:
“As well as many other treatments, including pelvic floor work, I have been seeing Dr Brown for the past year for the treatment of lower back pain and pelvic instability, which has its origins in competitive gymnastics but which flared after the birth of my son 1 year ago. At 16 weeks post-partum, I was virtually immobile, (pain level 10/10). We began an extensive course of spinal adjustments, neural therapy [Frankenhauser, pelvic injection] and prolotherapy on my back and pelvis, and saw modest results (7-8 /10). We then began a course of neural prolotherapy, which decreased the pain (2-3/10) initially, but increased after a week (6/10). Finally, we did 2 treatments of neural therapy on the perineal scar that occurred as a result of tearing at childbirth. At the time of the first treatment, I felt a twinge in my low back, at exactly the location that has created so much discomfort. We were working on the perineum, not my back, yet the connection was clear. After that first treatment, I had a substantial improvement in both my low back pain (2/10), but also, importantly, pain that had been occurring with intercourse since giving birth. Two weeks later, we did a second treatment on the scar. Again, I have felt improvement in both my back and pelvic region with respect to pain levels (2/10). The situation has not yet completely resolved, but I am amazed at how much positive improvement has occurred since treating the scars.”
Recently, my patient received a third treatment to the deeper adhesions of the scar tissue. At one point during the injection she felt the reproduction of a longstanding rectal spasm that she experienced with orgasm. Since writing these comments, she has reported that the pain that had been occurring with intercourse decreased about 50% and that her libido increased. The rectal spasms on orgasm have ceased and her chronic incontinence is beginning to change. Although there is still back pain of 2-3/10 with normal activity, she is beginning to experience periods of no pain. Continued progress is expected.
The recto-vaginal fascia lies transversely and shallowly across the perineum between the vagina and rectum and extends through the pelvis. Fascial drag from deep adhesions in this area can affect any organ or structure in the pelvis. In spite of all the previous treatments, it was not until the biomechanical release of these tissues, combined with the correction of the autonomic disturbance field in the scar, that effective healing for this patient could progress.
 Hal Brown, ND, DC, RAc is a graduate of CMCC (1977), CCNM (1989), and ICTCM (1993). He is a cofounder and partner in Integrative Healing Arts (1983), where he practices in Vancouver BC. He is a former chair of Physical Medicine and instructor at BINM and served as Chair of the Manipulation Advisory Committee, CNPBC (2005). Dr Brown is a contributor to the Textbook of Naturopathic Physical Medicine (2007) and NDNR (2007). Past presentations include: NW Naturopathic Convention (2008), BCNA (2004), and the Third International Fascia Research Congress (2012).
Hal Brown, ND, DC, RAc is a graduate of CMCC (1977), CCNM (1989), and ICTCM (1993). He is a cofounder and partner in Integrative Healing Arts (1983), where he practices in Vancouver BC. He is a former chair of Physical Medicine and instructor at BINM and served as Chair of the Manipulation Advisory Committee, CNPBC (2005). Dr Brown is a contributor to the Textbook of Naturopathic Physical Medicine (2007) and NDNR (2007). Past presentations include: NW Naturopathic Convention (2008), BCNA (2004), and the Third International Fascia Research Congress (2012).
References
- Dosch P. Manual of Neural Therapy According to Huneke. 2nd ed. New York, NY: Thieme Medical Publishers; 2007.
- Sherratt JA. Mathematical Modelling of Scar Tissue Formation. Edinburgh, UK: Heriot-Watt University, Department of Mathematics; 2010. http://www.ma.hw.ac.uk/~jas/researchinterests/scartissueformation.html. Accessed August 20, 2010.
- Guimberteau JC. Skin, Scars and Stiffness. [DVD]. Endovivo Productions; http://www.endovivo.com/en/cicatrices,inflammation,dvd.php. Accessed September 15, 2012.
- Kidd RF. Interference Fields. In: Neural Therapy. Renfrew, ON: Custom Printers of Renfrew Ltd; 2005.
- Dellon AL. Painful Scars. In: Schmidt RF, Gebhart GF, eds. Encyclopedia of Pain. (Currently in development for publication of the 2nd ed.) London, UK: Springer-Verlag. http://www.springerreference.com/docs/html/chapterdbid/334007.html. Accessed April 24, 2013.
- Upledger JE, Vredovoogd J. Craniosacral Therapy. Seattle, WA: Eastland Press; 1983.
- Chaitow L, Russ D, Shipley DJ. Assessment/Palpation Section: Skills. In: Chaitow L, ed & co-author. Naturopathic Physical Medicine: Theory and Practice for Manual Therapists. Elsevier; 2008:125-197.
- Williams L. Blocks to Healing: Chronic Dominant Foci. In: Radical Medicine: Cutting-Edge Natural Therapies That Treat the Root Causes of Disease. Rochester, VT: Healing Arts Press; 2007:402-420.
- Klinghardt D. Neural Therapy Course A: Scars [seminar notes]. American Academy of Neural Therapy, Seattle Wash; 1993.
- Hooshmand H. Chronic Pain: Reflex Sympathetic Dystrophy, Prevention, and Management. Boca Raton, FL: CRC Press; 1993.
- Cass R. Progressive Clinical ElectroDermal (EAV/EDS) Screening Skills, Techniques & Protocols: 2013 Course Syllabus. London, ON: Academy of International BioEnergetic Sciences. http://www.aoibs.com/flyers/2013-Academy%20Syllabus.pdf.
- Gardner-Abbate S. The Art of Palpatory Diagnosis in Oriental Medicine. Philadelphia, PA: Churchill Livingstone; 2001:167-176.
- Jones TA. Rolfing. Phys Med Rehabil Clin N Am. 2004;15(4):799–809.
- Brook M. The Importance of Scar Tissue Release Therapy. Massage Today. June, 2009;9(6). http://www.massagetoday.com/mpacms/mt/article.php?id=14020. Accessed April 24, 2013.
- Friction massage. August 5, 2013. Criax Web site. http://www.om-cyriax.com/info.asp?language=en&pagina=Friction%20massage#. Accessed April 24, 2013.
- Lyftogt J. Neural Prolotherapy: Extinguishing Neuropathic Pain [seminar notes]. From: Neural Prolotherapy workshop; April 12-14, 2013; Seattle, WA.
- Zurada JM, Kriegel D, Davis IC. Topical treatments for hypertrophic scars. J Am Acad Dermatol. 2006;55(6):1024-1031.
- Baker R, Urso-Baiarda F, Grobbelaar A. Cutaneous scarring: a clinical review. Dermatol Res Pract. 2009;2009:625376.
- Mustoe TA, Cooter RD, Gold MH, et al. International clinical recommendations on scar management. Plast Reconstr Surg. 2002;110(2):560–571.
- Hultman CS, Edkins RE, Lee CN, et al. Shine on: Review of Laser- and Light-Based Therapies for the Treatment of Burn Scars. Dermatol Res Pract. 2012;2012:243651.
- Defalque RJ. Painful trigger points in surgical scars. Anesth Analg. 1982;61(6):518-520.
- MacAllister N, Fleck-D’Andrea T, Sallovitz K, et al. Clinical Evidence Suggests IV Glutathione Enhances Myofascial Manipulative Effects [abstract]. In: 6.2 Abstracts from Paper/Oral Session on Surgery and Scars, Third International Fascia Research Congress. Munich, Germany: Kiener Press; 2012:113.
- Dr Hal Brown. Neural therapy injection of scar tissue, Vancouver
. July 30, 2012. YouTube website. http://www.youtube.com/watch?v=yqQ29G6CnzM.