JILLIAN STANSBURY, ND
Opiate addiction is an enormous and devastating health problem worldwide, with over 5 million active addicts in the United States alone.1 And not only the addict is affected; marriages suffer or are ruined; jobs are lost; meaningful relationships to people, other hobbies, nature, and the world at large are lost; and, most of all, the mind and body are destroyed bit by bit from heroin use. Many addicts become homeless once loved ones can no longer tolerate the thefts and behaviors, and employers cannot forgive the absenteeism. The homeless population is subject to its own litany of problems, including being at risk for violent deaths among them.
Chasing the Dragon
Prescriptions for opiate-based analgesics have skyrocketed in the last decade, according to DEA statistics,2 which many people report is an inciting factor that ultimately leads to heroin addiction. The opiate industry itself is almost nothing but dark – troubled by the limited availability of raw material, low yields, and the byproduct of toxic wastes, in addition to the addiction, associated crime, and high mortality and morbidity.3 Furthermore, an attempt to gain access to poppy raw materials the United States may be a hidden agenda in the US efforts to muscle its presence into Afghanistan. Canadian economics professor, Michel Chossudovsky, reported that “Heroin is a multibillion dollar business supported by powerful interests, which requires a steady and secure commodity flow. One of the “hidden” objectives of the war [in Afghanistan] was precisely to restore the CIA sponsored drug trade to its historical levels and exert direct control over the drug routes.” 4
Opiate Maintenance Therapy
The Rockefeller Institute performed research on possible pharmacotherapies for long-term opiate addiction in the 1960s, beginning the search for successful therapies for heroin addiction. Professor Vincent P. Dole and his team hypothesized that heroin addiction is a disease of the brain with behavioral manifestations, and not merely a personality disorder or criminal behavior. Research was begun to discover whether a long-acting opioid agonist could improve successful heroine abstinence; however, due to political social stigma reasons, the FDA did not support the development of such pharmacotherapies for nearly 40 years. It was not until the turn of the millennium, following the release of an NIH report supporting long-acting opiates such as methadone maintenance, that the fruits of the Rockefeller research were finally implemented.5
The heroin replacement therapies, commonly referred to as Opiate Maintenance Therapy (OMT) involve the supply of an opioid agonist, such as methadone. The rationale is that it decreases excruciating cravings for heroin, alleviates devastating withdrawal symptoms, and mitigates the need to beg, borrow, and steal the money necessary to maintain the heroin habit, yet is delivered at a controlled dosage below the euphoria threshold. Opiate replacement therapies can improve social and familial functioning and support general survival. Many heroin addicts die from not only overdose, but a variety of causes including greatly accelerated aging, and diseases associated with IV drug use including AIDS, hepatitis-induced liver failure, and endocarditis and heart failure; OMT can help reduce such risks.
Herbal Options as Opiate Replacement Therapies
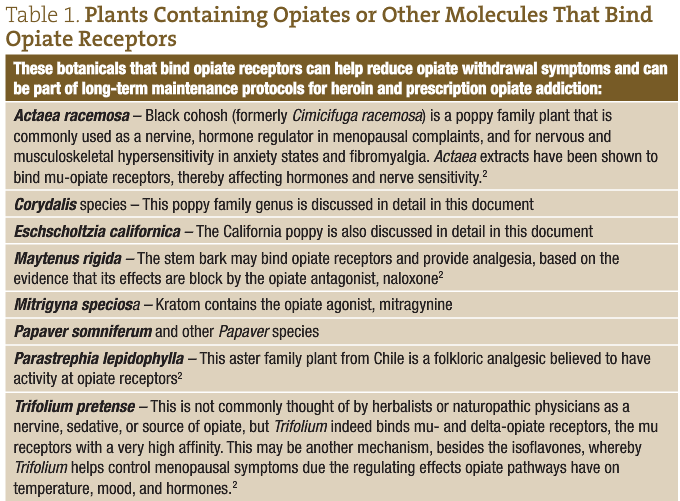
Most of the current therapies for opiate withdrawal involve replacing the short-acting opiates, such as heroin, with a long-acting opiate that reduces craving without producing the euphoric effect. While these opiate maintenance therapies may have many benefits for addicts, a big drawback is that they maintain the upregulated opioid circuitry in the brain. Non-opiate therapies may include GABA and herbs that bind GABA; agents that affect noradrenaline, dopamine, serotonin, and other pathways outside of the opiates; and agents that regulate stress pathways of the HPA axis. Following are herbal suggestions for opiate replacement options, as well as non-opiate options to include in acute withdrawal and long-term maintenance therapies for heroin addicts.
Corydalis Species: C yanhusuo, C bungeana, C humosa
Corydalis is a genus in the poppy family (Papaveracea), long used as a sedative and analgesic and containing constituents that include many isoquinoline alkaloids, such as tetrahydropalmatine, corydaline, protopine, berberine, palmatine, jatrorrhizine, coptisine, and dehydrocorydaline,6,7 that may affect limbic and reward pathways. These alkaloids are also referred to as protoberberine alkaloids, and some (including palmatine, jatrorrhizine, coptisine, and dehydrocorydaline) may also act as cholinesterase inhibitors, serving to maintain acetylcholine and promote parasympathetic tone.7 Corydalis cava may promote adrenaline breakdown and metabolism, as well as the synthesis of melanin from dihydroxy-phenylalanine (DOPA). The half-life of phenolase enzymes is greatly lengthened by Corydalis.8
The alkaloid tetrahydropalmatine occurs in both Corydalis and Stephania species, and both plants are mentioned as being helpful for opiate addiction. Tetrahydropalmatine has been incorporated into a prescription drug in China. Tetrahydropalmatine has been shown to bind to dopamine receptors and act as an antagonist at D1 and D2, and an agonist at D3, and α-adrenergic and serotonin receptors.9 L-tetrahydropalmatine has been shown to decrease self-administration of heroin in animal models of addiction,10 and prevent heroin-driven changes in the nucleus accumbens and ventral tegmental area.11 Levo-tetrahydropalmatine has been found to diminish activation of the reward pathway in animal models of methamphetamine addiction, suggesting balancing effects on the limbic system.12 Levo-tetrahydropalmatine may also protect the limbic system from stress-induced changes in gene expression,13 and may also bind to GABA receptors.14
L-isocorypalmine is a methylated analog of L-tetrahydropalmatine, and is found to bind dopamine receptors and act as a partial agonist at D1 receptors, and antagonist at D2 receptors, serving to mitigate cocaine withdrawal symptoms.15 Acetylcorynoline is another an alkaloid in C bungeana, shown to prevent dopaminergic degeneration in Parkinson’s disease models.16 Another Corydalis root constituent, the isoquinoline alkaloid, tetrahydroberberine, may help correct the digestive suppression induce by opiate drugs by upregulating gastrointestinal motility via dopaminergic effects at D2 receptors and serotonergic receptor agonism.17
Eschscholtzia californica
Eschscholtzia californica (California poppy) is in the poppy family and native to the west coast of North America where it was used as a sleep aid and pain remedy by indigenous people of the region (Figure 1). Eschscholtzia remains in common use as a gentle nervine and may be considered in herbal formulas for easing opiate withdrawal symptoms and possibly long-term maintenance therapies to reduce the cravings. Eschscholtzia may inhibit the enzymatic degradation of catecholamine, as well as inhibit the synthesis of adrenaline. Inhibition of diamine oxidases and monoamine oxidase are among the mechanisms of action.8

Harpagophytum procumbens
Devil’s claw has shown efficacy in reducing arthritic pain and reducing the need for other pain medications.18 The plant may be anti-inflammatory when applied topically.19 Some research has suggested that, in addition to anti-inflammatory effects, Harpagophytum may be pain-relieving via opiate pathways.20 This plant might especially be considered in formulas for those seeking to wean from opiate prescriptions for pain management.
Hypericum perforatum
St Johnswort is a well-known herb used for depression and anxiety. Extensive research on the plant shows it to have a broad effect on numerous neurotransmitters including serotonin, GABA, and dopamine. Animal studies suggest it may also help ease the symptoms of acute morphine withdrawal. In animal models of addiction, for example, Hypericum was shown to be as effective as clonidine for the symptoms of opiate withdrawal.21 Other researchers report Hypericum perforatum to reduce abdominal spasm and diarrhea in animal models of acute opiate withdrawal.22,23
Jitai Tablets and Jinnui Capsules
Jitai tablets are a TCM herbal marine product containing a dozen ingredients traditionally used for detoxification and acute opiate withdrawal symptoms. In TCM, such symptoms are described as poison-blood stasis, cold and heat complex, and spleen and kidney weakness. Some of the ingredients in this formula include amygdalin, danshensu, ferulic acid, hydroxysafflor yellow A, and salvianolic acids A and B.24 The effects of Jitai tablets are similar to those of clonidine in controlling the withdrawal symptoms of morphine-dependent animals. Clinical studies have further confirmed that Jitai tablets have good efficacy in controlling both acute and protracted opiate withdrawal symptoms. One clinical trial reported equal efficacy to lofexidine for acute heroin withdrawal.25,26 Adverse herb reactions are mild and can be reduced during the treatment or after drug reduction. No significant adverse effects have been found on liver and kidney function in patients.
Mitragyna speciosa
Kratom (also called kratum and ketum) is an Asian plant, often sought after by those looking for a drug-like effect after word spread of this use by villagers in Thailand and Malaysia. Mitragyna leaves contain mitragynine and related alkaloids that have both opiate and cocaine-like effects. Legislation was passed in Malaysia in 2004 to outlaw its sale and consumption, more due to concerns of it being a “gateway” drug than any real toxicity or abuse issues.27 One ethnobotanical survey reported many rural villagers ingesting Mitragyna extracts as tea on a daily basis, with reported effects including simple social and recreational effects, increased stamina and physical endurance, pain relief, and improved sexual performance. Many users reported difficulty in abstaining from consuming the tea so frequently.28 At the same time, many heroin addicts in Thailand and Malaysia report Mitragyna to have helped them wean off heroin.29 Animal studies suggest that Mitragyna induces cytochrome enzymes in the liver and speeds up metabolism of many drugs also metabolized via this pathway.27
Salvia divinorum
The plant is sometimes referred to as “Magic Mint” even though it is a perennial sage; however, it is a member of the mint or Labaitae family, not a family known for its psychedelics, like the poppy and cactus families. Salvia divinorum is native to the Oaxaca area of Mexico where it has been a longstanding sacred plant used in rituals. Salvia divinorum has been used as a treatment for the “semimagical” disease, panzón de borrego. The Mazatec people of Mexico also used Salvia divinorum for rituals and to treat gastrointestinal disorders.30
The effects of Salvia divinorum come on quickly, within 1 minute following ingestion, and last for a relatively short period of time. Researchers report that these rapid effects may be due to the ability of salvinorin A to modulate the P-glycoprotein transporter and gain rapid transport through the blood-brain barrier.31 Human investigations report no cognitive deficits or changes to vital signs with use; however, spikes in prolactin and cortisol occur transiently.32 Other than talking, laughing, and moving more often, no untoward physical symptoms were observed in clinical placebo-controlled trials examining effects of Salvia divinorum ingestion.33 Salvinorin A did not significantly increase heart rate or blood pressure. Participant narratives indicated intense experiences characterized by disruptions in vestibular and interoceptive signals (eg, change in spatial orientation, pressure on the body) and unusual and sometimes-recurring themes across sessions, such as revisiting childhood memories, cartoon-like imagery, and contact with entities.34
Salvia divinorum’s most studied constituents are its diterpenes. Salvinorin diterpenes are classified as neoclerodane, said to be the first identified non-nitrogenous ligand of the opiate receptor35; and the diterpene salvinorin A, shown to be a kappa-opioid agonist and the first reported psychoactive diterpene known to exist in nature.36 Other naturally-occurring neoclerodanes from a variety of Salvia species may have an affinity for opioid receptors, albeit not with the very strong binding affinity seen with salvinorin.37 Salvinorin may act via both opiate and cannabinoid receptors to mitigate both stress and pain pathways.38 Animal research suggests that salvinorin may reverse depression associated with chronic stress.39 Researchers also report that the ability to limit negative emotional consequences may also cause chronic use of Salvia divinorum to impair memory formation, in general, and affect learning.40 Isolated salvinorin A has therapeutic potential as a treatment for pain, mood and personality disorders, substance abuse, and gastrointestinal disturbances41; the nonalkaloids have also been suggested as potential scaffolds for drug development.42
Like many opiate agonists, S divinorum affects colonic function. Salvinorin A inhibits gastrointestinal peristalsis through activation of kappa-opioid receptors, and reduces neurogenic ion channel transport when overstimulated due to the presence of endotoxins, explaining its historical use for intestinal disorders.43 Additionally, as intestinal inflammation upregulates cannabinoid receptors and endogenous cannabinoids, salvinorin A may improve gastrointestinal symptoms through cannabinoid pathways as well.44
Because there are cannabinoid receptors on immune cells and lymphatic tissue, some of the anti-inflammatory effects of marijuana and Salvia divinorum may be via binding these receptors. Salvia divinorum has been found to have modulating effects on activated macrophages, for example.45
Scopalamine
Scopalamine is a tropane alkaloid found in many nightshades family members, such as Atropa belladonna, Hyoscyamus, and Datura. Isolated scopolamine has been used for decades as a topical patch to prevent acute motion sickness in susceptible individuals. Recent research compared a scopolamine detoxification technique (SDT) with methadone for acute heroin withdrawal symptoms.46 While all patients received methadone from 1 to 3 days, half were switched to SDT for the subsequent 3 days. SDT involves the IV administration of both scopolamine and chlorpromazine for 4 to 6 hours each day. Study participants reported their withdrawal symptoms on a daily basis. Urine samples were collected twice a week following discharge, and a questionnaire for reporting reasons for relapse was collected following opiate-positive urinalyses. Although groups did not differ on retention or the percentage of opioid-positive urine samples, the SDT group reported less heroin craving, depression, and anxiety compared with the methadone group.46 Datura leaves are an ingredient in the traditional Chinese Jitai formula discussed above.
Withania somnifera
Ashwaghanda, or Indian ginseng, has been reported to mitigate the effects of morphine on the CNS and is therefore considered a possible tool in the treatment of opiate addiction.47 Withania has effects on GABA receptors (γ-aminobutyric acid) and may also have weak binding at mu-opioid receptors.47
In recent decades, Withania has also been demonstrated in numerous studies to support protection and regeneration of neurons in various disease and inflammatory models. Withania has been shown to reduce heroin withdrawal symptoms if given chronically prior to withdrawal, but not to ease the symptoms when given upon initial abstinence in animal models of heroin addiction and withdrawal. Further, long-term ingestion of Withania has been shown to fully prevent the loss of dopaminergic density in the nucleus procumbens that typically happens upon opiate withdrawal.48 This suggest that pretreatment with Withania, prior to withdrawal, has possible therapeutic benefits for heroin addicts.
A Bit of History: From Opium to Morphine to Heroin
The English physician, Thomas Sydenham, developed a remedy easier to administer than crude opium, with the advent of an opiate tincture called laudanum, in 1683. Laudanum became the leading pharmaceutical for pain for several hundred years.49 Paracelsus, however, used the term “laudanum” 150 years prior for his own opiate-based pain remedy, and chose the name from the Latin verb “laudare”, meaning “to praise.”
Morphine is said to be the first-ever plant alkaloid to be purified, and was isolated in 1804 by Friedrich Sertürner. He, himself, distributed the substance as an analgesic for a decade until it began to be produced and sold commercially by a small independent chemists’ apothecary that has since grown into the pharmaceutical giant, Merck. The sale of morphine became even more popular after the development of the hypodermic needle in 1857. Heroin was first synthesized from morphine in 1874 and brought to market by Bayer in 1898. In the 1950s, it became possible to synthesize morphine from petrochemicals.
Upon its initial discovery, morphine was thought helpful for opium addiction and alcoholism, but was quickly discovered to be more addictive than either opium or alcohol. Morphine was used widely during the American Civil War, resulting in some 400 000 soldiers having morphine addiction. Thomas de Quincey published Confessions of an English Opium-Eater in 1821, inciting a national debate on opiate drugs.50

 Jillian Stansbury, ND has practiced in SW Washington for nearly 20 years, specializing in women’s health, mental health, and chronic disease. She holds undergraduate degrees in medical illustration and medical assisting, and graduated with honors in both programs. Dr Stansbury also chaired the botanical medicine program at NCNM and has taught the core botanical curricula for more than 20 years. In addition, Dr Stansbury writes and serves as a medical editor for numerous professional journals and lay publicans, plus teaches natural products chemistry and herbal medicine around the country. At present, she is working to set up a humanitarian service organization in Peru and studying South American ethnobotany. She is the mother of two adult children, and her hobbies include art, music, gardening, camping, international travel, and the study of quantum and metaphysics.
Jillian Stansbury, ND has practiced in SW Washington for nearly 20 years, specializing in women’s health, mental health, and chronic disease. She holds undergraduate degrees in medical illustration and medical assisting, and graduated with honors in both programs. Dr Stansbury also chaired the botanical medicine program at NCNM and has taught the core botanical curricula for more than 20 years. In addition, Dr Stansbury writes and serves as a medical editor for numerous professional journals and lay publicans, plus teaches natural products chemistry and herbal medicine around the country. At present, she is working to set up a humanitarian service organization in Peru and studying South American ethnobotany. She is the mother of two adult children, and her hobbies include art, music, gardening, camping, international travel, and the study of quantum and metaphysics.
References
- Preda A. Opioid Abuse. Medscape Web site. http://emedicine.medscape.com/article/287790-overview. Accessed February 19, 2014.
- Rawool V, Dluhy C. Auditory sensitivity in opiate addicts with and without a history of noise exposure. Noise Health. 2011;13(54):356-363.
- Boonstra B, Rathbone DA, Bruce NC. Engineering novel biocatalytic routes for production of semisynthetic opiate drugs. Biomol Eng. 2001;18(2):41-47.
- Global Research, Center for Research on Globalization. Chossudovsky M. The Spoils of War: Afghanistan’s Multibillion Dollar Heroin Trade. June 14, 2005. Global Research Web site. http://www.globalresearch.ca/the-spoils-of-war-afghanistan-s-multibillion-dollar-heroin-trade/91. Accessed January 15, 2014.
- Kreek MJ. Opioid receptors: some perspectives from early studies of their role in normal physiology, stress responsivity, and in specific addictive diseases. Neurochem Res. 1996;21(11):1469-1488.
- Zheng XK, Li DD, Yan H, et al. Two new alkaloids from Corydalis humosa. J Asian Nat Prod Res. 2013;15(11):1158-1162.
- Xiao HT, Peng J, Liang Y, et al. Acetylcholinesterase inhibitors from Corydalis yanhusuo. Nat Prod Res. 2011;25(15):1418-1422.
- Kleber E, Schneider W, Schäfer HL, et al. Modulation of key reactions of the catecholamine metabolism by extracts from Eschscholtzia californica and Corydalis cava. Arzneimittelforschung. 1995;45(2):127-131.
- Wang JB, Mantsch JR. L-tetrahydropalamatine: a potential new medication for the treatment of cocaine addiction. Future Med Chem. 2012;4(2):177-186.
- Yue K, Ma B, Ru Q, et al. The dopamine receptor antagonist levo-tetrahydropalmatine attenuates heroin self-administration and heroin-induced reinstatement in rats. Pharmacol Biochem Behav. 2012;102(1):1-5.
- Luo SY, Guo P, Qian G, et al. Study on acting mechanism of anti-morphine conditioned place preference between aqueous extract of Corydalis yanhusuo and L-THP and comparison of their effects. Zhongguo Zhong Yao Za Zhi. 2012;37(22):3457-3461.
- Su HL, Zhu J, Chen YJ, et al. Roles of levo-tetrahydropalmatine in modulating methamphetamine reward behavior. Physiol Behav. 2013;118:195-200.
- Ceremuga TE, Shellabarger P, Persson T, et al. Effects of tetrahydropalmatine on post-traumatic stress disorder-induced changes in rat brain gene expression. J Integr Neurosci. 2013;12(4):513-528.
- Henkes H, Franz M, Kendall O, et al. Evaluation of the anxiolytic properties of tetrahydropalmatine, a Corydalis yanhusuo compound, in the male Sprague-Dawley rat. AANA J. 2011;79(4 Suppl):S75-S80.
- Xu W, Wang Y, Ma Z, et al. L-isocorypalmine reduces behavioral sensitization and rewarding effects of cocaine in mice by acting on dopamine receptors. Drug Alcohol Depend. 2013;133(2):693-703.
- Fu RH, Wang YC, Chen CS, et al. Acetylcorynoline attenuates dopaminergic neuron degeneration and α-synuclein aggregation in animal models of Parkinson’s disease. Neuropharmacology. 2013 Aug 21. pii: S0028-3908(13)00364-X.
- Lee TH, Kim KH, Lee SO, et al. Tetrahydroberberine, an isoquinoline alkaloid isolated from corydalis tuber, enhances gastrointestinal motor function. J Pharmacol Exp Ther. 2011;338(3):917-924.
- Warnock M, McBean D, Suter A, et al. Effectiveness and safety of Devil’s Claw tablets in patients with general rheumatic disorders. Phytother Res. 2007;21(12):1228-1233.
- Abdelouahab N, Heard CM. Dermal and Transcutaneous delivery of the major glycoside constituents of Harpagophytum procumbens (Devil’s Claw) in vitro. Planta Med. 2008;74(5):527-531.
- Uchida S, Hirai K, Hatanaka J, et al. Antinociceptive effects of St. John’s wort, Harpagophytum procumbens extract and Grape seed proanthocyanidins extract in mice. Biol Pharm Bull. 2008;31(2):240-245.
- Feily A, Abbasi N. The inhibitory effect of Hypericum perforatum extract on morphine withdrawal syndrome in rat and comparison with clonidine. Phytother Res. 2009;23(11):1549-1552.
- Subhan F, Khan N, Sewell RD. Adulterant profile of illicit street heroin and reduction of its precipitated physical dependence withdrawal syndrome by extracts of St John’s wort (Hypericum perforatum). Phytother Res. 2009;23(4):564-571.
- Khan M, Subhan F, Khan AU, et al. Nature cures nature: Hypericum perforatum attenuates physical withdrawal signs in opium dependent rats. Pharm Biol. 2013 Nov 21. [Epub ahead of print]
- Wanga SP, Liu L, Wang LL, et al. Simultaneous determination of six hydrophilic components in rat plasma after oral administration of Jitai tablet by liquid chromatography–electrospray ionization–tandem mass spectrometry: Application to a pharmacokinetic study. J Chromatogr B Analyt Technol Biomed Life Sci. 2013;912:75–84.
- Shi J, Xu GZ, Liu TT, et al. A comparative clinical study of the effects of the traditional Chinese medicine Jinniu capsules and lofexidine on acute heroin withdrawal symptoms. Am J Drug Alcohol Abuse. 2008;34(6):792-800.
- Hao SQ, Zhao M, Zhang RW, et al. The effectiveness comparison of Jitai tablets versus methadone in community-based drug treatment: a 1-year follow-up study. Addict Behav. 2013;38(10):2596-2600.
- Azizi J, Ismail S, Mansor SM. Mitragyna speciosa Korth leaves extracts induced the CYP450 catalyzed aminopyrine-N-demethylase (APND) and UDP-glucuronosyl transferase (UGT) activities in male Sprague-Dawley rat livers. Drug Metabol Drug Interact. 2013;28(2):95-105.
- Ahmad K, Aziz Z. Mitragyna speciosa use in the northern states of Malaysia: a cross-sectional study. J Ethnopharmacol. 2012;141(1):446-450.
- Vicknasingam B, Narayanan S, Beng GT, Mansor SM. The informal use of ketum (Mitragyna speciosa) for opioid withdrawal in the northern states of peninsular Malaysia and implications for drug substitution therapy. Int J Drug Policy. 2010;21(4):283-288.
- Piekielna J, Fichna J, Janecka A. Salvinorin A and related diterpenes–biological activity and potential therapeutic uses. Postepy Biochem. 2012;58(4):485-491.
- Butelman ER, Caspers M, Lovell KM, et al. Behavioral effects and central nervous system levels of the broadly available κ-agonist hallucinogen salvinorin A are affected by P-glycoprotein modulation in vivo. J Pharmacol Exp Ther. 2012;341(3):802-808.
- Ranganathan M, Schnakenberg A, Skosnik PD, et al. Dose-related behavioral, subjective, endocrine, and psychophysiological effects of the κ opioid agonist Salvinorin A in humans. Biol Psychiatry. 2012;72(10):871-879.
- Addy PH. Acute and post-acute behavioral and psychological effects of salvinorin A in humans. Psychopharmacology (Berl). 2012;220(1):195-204.
- Johnson MW, MacLean KA, Reissig CJ, et al. Human psychopharmacology and dose-effects of salvinorin A, a kappa opioid agonist hallucinogen present in the plant Salvia divinorum. Drug Alcohol Depend. 2011;115(1-2):150-155.
- Prisinzano TE. Neoclerodanes as atypical opioid receptor ligands. J Med Chem. 2013;56(9):3435-3443.
- Casselman I, Nock CJ, Wohlmuth H, et al. From local to global-Fifty years of research on Salvia divinorum. J Ethnopharmacol. 2014;151(2):768-783.
- Fontana G, Savona G, Rodríguez B, et al. Synthetic studies of neoclerodane diterpenoids from Salvia splendens and evaluation of Opioid Receptor affinity. Tetrahedron. 2008;64(43):10041-10048.
- Guida F, Luongo L, Aviello G, et al. Salvinorin A reduces mechanical allodynia and spinal neuronal hyperexcitability induced by peripheral formalin injection. Mol Pain. 2012;8:60.
- Harden MT, Smith SE, Niehoff JA, et al. Antidepressive effects of the κ-opioid receptor agonist salvinorin A in a rat model of anhedonia. Behav Pharmacol. 2012;23(7):710-715.
- Braida D, Donzelli A, Martucci R, et al. Learning and memory impairment induced by salvinorin A, the principal ingredient of Salvia divinorum, in wistar rats. Int J Toxicol. 2011;30(6):650-661.
- Fichna J, Schicho R, Janecka A, et al. Selective natural kappa opioid and cannabinoid receptor agonists with a potential role in the treatment of gastrointestinal dysfunction. Drug News Perspect. 2009;22(7):383-392.
- Cunningham CW, Rothman RB, Prisinzano TE. Neuropharmacology of the naturally occurring kappa-opioid hallucinogen salvinorin A. Pharmacol Rev. 2011;63(2):316-347.
- Fichna J, Dicay M, Hirota SA, et al. Differential effects of salvinorin A on endotoxin-induced hypermotility and neurogenic ion transport in mouse ileum. Neurogastroenterol Motil. 2011 Jun;23(6):583-e212.
- Capasso R, Borrelli F, Cascio MG, et al. Inhibitory effect of salvinorin A, from Salvia divinorum, on ileitis-induced hypermotility: cross-talk between kappa-opioid and cannabinoid CB(1) receptors. Br J Pharmacol. 2008;155(5):681-689.
- Aviello G, Borrelli F, Guida F, et al. Ultrapotent effects of salvinorin A, a hallucinogenic compound from Salvia divinorum, on LPS-stimulated murine macrophages and its anti-inflammatory action in vivo. J Mol Med (Berl). 2011;89(9):891-902.
- Liu S, Li L, Shen W, et al. Scopolamine detoxification technique for heroin dependence: a randomized trial. CNS Drugs. 2013;27(12):1093-1102.
- Ruiu S, Longoni R, Spina L, et al. Withania somnifera prevents acquisition and expression of morphine-elicited conditioned place preference. Behav Pharmacol. 2013;24(2):133-143.
- Kasture S, Vinci S, Ibba F, et al. Withania somnifera prevents morphine withdrawal-induced decrease in spine density in nucleus accumbens shell of rats: a confocal laser scanning microscopy study. Neurotox Res. 2009;16(4):343-355.
- Warolin C. The opiate pharmacopeia in France from its origins to the 19th century. Rev Hist Pharm (Paris). 2010;58(365):81-90.
- Schäfer D. Milk of paradise? Opium and opiates in nineteenth and twentieth century literature. Schmerz. 2007;21(4):339-344, 346.





