Cheryl Burdette, ND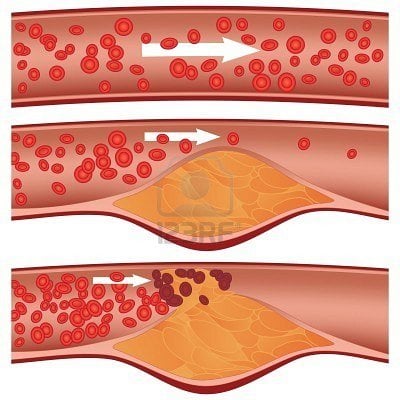
Various biomarkers are believed to be risk factors for cardiovascular disease. Some of these include high serum levels of total cholesterol, low-density lipoprotein cholesterol (LDL-C), and triglycerides, as well as low serum levels of high-density lipoprotein cholesterol (HDL-C). However, it has been repeatedly observed that many individuals with various cardiovascular diseases have test values within the normal range for these potential risk factors. Therefore, the analysis of other biomarkers may be more specific and accurate for predicting and treating cardiovascular disease; these biomarkers need to be investigated. One such biomarker with notable evidence of a role in cardiovascular disease is an elevated level of oxidized LDL-C (OxLDL). Many investigations have confirmed that high OxLDL level is associated with cardiovascular diseases such as atherosclerosis and coronary artery disease; this is particularly owing to the proatherogenic properties of OxLDL. Furthermore, treatments to lower the OxLDL level and to prevent the oxidation of unmodified LDL-C may have a beneficial effect on cardiovascular disease.
Many studies have documented an association between OxLDL level and other diseases. These include diabetes mellitus, metabolic syndrome, polycystic ovary syndrome, multiple sclerosis, stroke, and kidney disease.
Relevance of OxLDL to Cardiovascular Disease
As already stated, OxLDL is a likely biomarker for cardiovascular disease. For example, in a study by Toshima et al,1 the mean (SD) plasma OxLDL levels were significantly higher in 65 patients with coronary heart disease (201.3 [11.2] U/dL) than in 181 control subjects (112.4 [3.3] U/dL) (P < .01). In that study, OxLDL levels were not associated with age, sex, total cholesterol level, or apolipoprotein B level in healthy control subjects.
Increasing evidence also suggests that the OxLDL level (or sometimes the ratio of OxLDL to HDL-C) is a more adequate biomarker for cardiovascular disease than total cholesterol, HDL-C, LDL-C, or triglycerides levels. A 2006 study2 published in The American Journal of Cardiology measured the ratio of OxLDL to HDL-C and the levels of total cholesterol, LDL-C, HDL-C, triglycerides, and lipoprotein-associated phospholipase A2 in 431 healthy men and women without clinical evidence of coronary artery disease and in 490 men and women with coronary artery disease. In that study, the OxLDL level identified more patients with coronary artery disease than the other more widely used biomarkers. Furthermore, the diagnostic accuracy of OxLDL level was 1.43 times greater than that for LDL-C level.
A similar study by Huang et al3 measured blood OxLDL, total cholesterol, LDL-C, HDL-C, triglycerides, and albumin levels in 80 patients with acute myocardial infarction, 80 patients with unstable angina pectoris, 80 patients with stable angina pectoris, 60 healthy control subjects, and 60 control subjects with dyslipidemia. The authors found that the OxLDL level and the oxidation ratio of LDL (OxLDL to total cholesterol, OxLDL to LDL-C, OxLDL to HDL-C, and OxLDL to albumin) were significantly higher among the disease groups than among the controls (P < .001). Among patients having coronary artery disease with comorbid hypertension or diabetes mellitus, the OxLDL level and the oxidation ratio of LDL increased further (P < .001). The mean (SD) ratio of OxLDL to albumin in the acute myocardial infarction group (0.068 [0.017]) was 7 times higher than that in the healthy control group (0.009 [0.007]) (P < .001). These findings demonstrate that the OxLDL level and the oxidation ratio of LDL are better biomarkers than total cholesterol, LDL-C, HDL-C, and triglycerides levels for discriminating between patients with coronary artery disease and healthy individuals.
Proatherogenic Mechanism of OxLDL
Oxidized LDL-C is highly atherogenic in vitro and in vivo; it is a plaque-specific protein that is not detected in healthy arteries. It stimulates the differentiation of macrophage cells into lipid-laden foam cells, induces apoptosis of vascular endothelial cells, and stimulates the production of many proinflammatory molecules such as monocyte chemotactic protein 1, high-sensitivity C-reactive protein, interleukin 6, and tumor necrosis factor.4,5
Unmodified LDL-C becomes oxidized through enzymatic and nonenzymatic reactions by endothelial cells and macrophages in arterial tissue.6,7 Modified LDL-C is taken up by scavenger receptors. Lectin-like oxidized LDL receptor 1 (LOX-1), which is increasingly thought to be a biomarker for cardiovascular disease, is the primary scavenger receptor of OxLDL; as a receptor, it differs from the unmodified LDL receptor. The uptake of OxLDL through the LOX-1 receptor results in the conversion to foam cells, which results in plaque formation. In addition, LOX-1 expression has been observed to be high within vascular lesions and may be diagnostic of patients with acute coronary syndrome.8,9
OxLDL and Other Diseases
Oxidized LDL-C has been linked to various other conditions and diseases. As one would anticipate, antioxidants are therapies of choice when treating elevated OxLDL. Successful treatments for oxidized LDL-C include cocoa,10 resveratrol,11 olive oil,12 walnuts,12 a gluten-free diet,13 the Mediterranean diet,14 vitamin E,15 pistachios,16 lycopene,17 green tea,18 l-carnitine,19 vitamin C,20 coenzyme Q10,21 and hazelnuts.22
Conclusion
Biomarkers need to be researched and evaluated for their role in cardiovascular disease. Oxidized LDL-C seems to offer more predictive value than other biomarkers being tested, including total cholesterol, HDL-C, LDL-C, and triglycerides levels. In addition to more accurately predicting risk for heart disease, OxLDL guides treatment in a way that is therapeutically meaningful. The use of this biomarker aids the clinician in distinguishing therapies to block the production of cholesterol vs treating the oxidation of LDL with antioxidant therapies.
 Cheryl Burdette, ND is the president and educational director of NutraTest Laboratories, Dunwoody, Georgia. She is a graduate of Bastyr University, Kenmore, Washington. She is in private practice in Atlanta, Georgia, at Progressive Medical. She serves on institutional review boards, teaches at the University of Bridgeport (Bridgeport, Connecticut), and lectures internationally. Dr Burdette serves on the board of advisors for XYMOGEN (Orlando, Florida). She has contributed chapters to Laboratory Evaluations of Molecular Medicine and has published articles in medical journals as well.
Cheryl Burdette, ND is the president and educational director of NutraTest Laboratories, Dunwoody, Georgia. She is a graduate of Bastyr University, Kenmore, Washington. She is in private practice in Atlanta, Georgia, at Progressive Medical. She serves on institutional review boards, teaches at the University of Bridgeport (Bridgeport, Connecticut), and lectures internationally. Dr Burdette serves on the board of advisors for XYMOGEN (Orlando, Florida). She has contributed chapters to Laboratory Evaluations of Molecular Medicine and has published articles in medical journals as well.
References
- Toshima S, Hasegawa A, Kurabayashi M, et al. Circulating oxidized low density lipoprotein levels: a biochemical risk marker for coronary heart disease. Arterioscler Thromb Vasc Biol. 2000;20:2243-2247.
- Johnston N, Jernberg T, Lagerqvist B, Siegbahn A, Wallentin L. Improved identification of patients with coronary artery disease by the use of new lipid and lipoprotein biomarkers. Am J Cardiol. 2006;97:640-645.
- Huang H, Mai W, Liu D, Hao Y, Tao J, Dong Y. The oxidation ratio of LDL: a predictor for coronary artery disease. Dis Markers. 2008;24:341-349.
- Levitan I, Volkov S, Subbaiah PV. Oxidized LDL: diversity, patterns of recognition, and pathophysiology. Antioxid Redox Signal. 2010;13:39-75.
- Verhoye E, Langlois MR. Circulating oxidized low-density lipoprotein: a biomarker of atherosclerosis and cardiovascular risk? Clin Chem Lab Med. 2009;47:128-137.
- Yoshida H, Kisugi R. Mechanisms of LDL oxidation. Clin Chim Acta. 2010;411:1875-1882.
- Parthasarathy S, Raghavamenon A, Garelnabi MO, Santanam N. Oxidized low-density lipoprotein. Methods Mol Biol. 2010;610:403-417.
- Ogura S, Kakino A, Sato Y, et al. LOX-1: the multifunctional receptor underlying cardiovascular dysfunction. Circ J. 2009;73:1993-1999.
- Reiss AB, Anwar K, Wirkowski P. Lectin-like oxidized low density lipoprotein receptor 1 (LOX-1) in atherogenesis: a brief review. Curr Med Chem. 2009;16:2641-2652.
- Baba S, Osakabe N, Kato Y, et al. Continuous intake of polyphenolic compounds containing cocoa powder reduces LDL oxidative susceptibility and has beneficial effects on plasma HDL cholesterol concentrations in humans. Am J Clin Nutr. 2007;85:709-717.
- Castilla P, Echarri R, Dávalos A, et al. Concentrated red grape juice exerts antioxidant, hypolipidemic, and antiinflammatory effects in both hemodialysis patients and healthy subjects. Am J Clin Nutr. 2006;84(1):252-262.
- Cortés B, Núnez I, Cofán M, et al. Acute effects of high-fat meals enriched with walnuts or olive oil on postprandial endothelial function. J Am Coll Cardiol. 2006;48:1666-1671.
- Elkan AC, Sjöberg B, Kolsrud B, et al. Gluten-free vegan diet induces decreased LDL and oxidized LDL levels and raised atheroprotective natural antibodies against phosphorylcholine in patients with rheumatoid arthritis: a randomized study. Arthritis Res Ther. 2008;10(2):R34. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2453753/?tool=pubmed. Accessed July 28, 2012.
- Fitó M, Guxens M, Corella D, et al. Effect of a traditional Mediterranean diet on lipoprotein oxidation. Arch Intern Med. 2007;167:1195-1203.
- Gutierrez AD, de Serna DG, Robinson I, et al. The response of gamma vitamin E to varying dosages of alpha vitamin E plus vitamin C. Metabolism. 2009;58:469-478.
- Kay CD, Gebauer SK, West SG, Kris-Etherton PM. Pistachios reduce serum oxidized LDL and increase serum antioxidant levels [abstract]. FASEB J. 2007;21:847.19. http://www.fasebj.org/cgi/content/meeting_abstract/21/6/A1091-a. Accessed July 28, 2012.
- Kim OY, Yoe HY, Kim HJ, et al. Independent inverse relationship between serum lycopene concentration and arterial stiffness. Atherosclerosis. 2010;208:581-586.
- Lee W, Min WK, Chun S, et al. Long-term effects of green tea ingestion on atherosclerotic biological markers in smokers. Clin Biochem. 2005;38(1):84-87.
- Malaguarnera M, Vacante M, Avitabile T, et al. l-Carnitine supplementation reduces oxidized LDL cholesterol in patients with diabetes. Am J Clin Nutr. 2009;86:1-6.
- Newsom SA, Paxton RJ, Rynn GM, et al. Influence of ascorbic acid on the thermic effect of feeding in overweight and obese adult humans. Obesity. 2008;16:1749-1754.
- Yubero-Serrano EM, Delgado-Casado N, Delgado-Lista J, et al. Postprandial antioxidant effect of the Mediterranean diet supplemented with coenzyme Q10 in elderly men and women. Age.2011;33:579–590
- Yücesan FB, Örem A, Kural BV, et al. Hazelnut consumption decreases the susceptibility of LDL to oxidation, plasma oxidized LDL level and increases the ratio of large/small LDL in normolipidemic healthy subjects. Anadolu Kardiyol Derg. 2010;10:28-35.