What are the Nerves Trying to Communicate?
CHRIS D. MELETIS, ND
About 7-10% of the population suffers from neuropathic pain and doctors are often unable to effectively and completely treat this condition.1 Often, this is because we try to address the problem after the fact rather than taking a proactive approach. Neurons are the longest-living cells in the body. Thus, much like an old-growth forest, it seems that conservation should be at the forefront of our clinical minds, ideally before there is a symptomatic presentation whenever possible.
Addressing the whole body will also yield better results when addressing a patient’s neuropathic pain. So much of medicine has become overly focused on systems and tissues, yet there is something to be said for treating the entirety of the human frame. Pain is a definitive sign of cellular dysfunction at an aggregate level.
This article will focus on the types of neuropathic pain and their pathology. It will also address global causes throughout the body and ways to support the health of patients experiencing neuropathic pain.
Types of Neuropathic Pain
Peripheral neuropathy results from injury to the peripheral nerves beyond the brain and spinal cord. It leads to weakness, numbness, and pain, primarily in the hands and feet, but it can also impact bodily functions such as digestion, urination, and circulation. Peripheral neuropathy usually causes stabbing, burning, or tingling pain. There are more than 100 types of peripheral neuropathy including everything from diabetic neuropathy to chemotherapy-induced carpal tunnel syndrome. Certain medications can also cause neuropathy including antimicrobials, cardiovascular drugs, psychotropics, and anticonvulsants.2
Diabetic neuropathy manifests in a variety of ways. It’s estimated that two-thirds of diabetic patients have clinical or subclinical neuropathy.3 Neuropathy becomes more common as the duration of diabetes increases. In a study of patients with diabetes, there was an increase in the incidence of neuropathy from 7.5% on admission to 50% at follow-up after 25 years.3,4 Peripheral neuropathy is the most common type of neuropathy in diabetics. Aside from peripheral neuropathy, there are 3 other forms that warrant discussion here.
- Proximal neuropathy (aka diabetic amyotrophy) is the second most common type of diabetic neuropathy and is associated with muscle weakness, especially in the upper legs, buttocks, and hips. Nerve pain associated with proximal neuropathy often radiates from the back to the leg.
- Autonomic neuropathy affects nerves in the autonomic nervous system, which regulates homeostasis of the body. Diabetic autonomic neuropathy can lead to premature death via silent myocardial infarction. Fully 25-50% of patients diagnosed with diabetic autonomic neuropathy die within 5 to 10 years of its onset.3 Since its symptoms can mimic diabetes and other disorders, autonomic diabetic neuropathy often remains undiagnosed by the physician and unnoticed by the patient.3
- Focal neuropathy (mononeuropathy) involves a single type of nerve, usually in the head, but it can also affect the torso and legs. When it occurs in the legs, the pain is usually located in specific locations, in contrast to proximal neuropathy, which may cause shooting pain throughout the legs.
Although these are common forms of neuropathy in diabetics, this group of patients is susceptible to other forms of neuropathy as well, such as cranial neuropathy (see case study).
Finally, postherpetic neuralgia (PHN) is the most common complication of shingles (aka acute herpes zoster), PHN causes burning, sharp, and jabbing pain that persists even after the rash and blisters of shingles resolve. Approximately 10% of shingles patients develop PHN, and the risk increases with age.5 In one study, 73% of PHN patients were 60 years of age or older.6 PHN can cause allodynia, a condition where pain occurs even after normally nonpainful stimuli, such as a light touch on the skin.
Who Is Susceptible to Neuropathic Pain?
Our bodies regularly deal with countless physiological and biochemical insults – often efficiently and without our knowing. As with any illness, individual susceptibility largely dictates how or if a patient experiences neuropathy. A common example seen in clinical practice is herpes zoster, the trigger to the onset of PHN. Though many individuals experience shingles, a minority of them develop PHN.
What drives neuropathic pain in some people? A deficiency of key nutrients and antioxidants is a significant risk factor. A nutrient-depleted environment throughout the body creates a state I refer to as “pan-nutrient insufficiency.”
Allostatic load is another driver of neuropathic pain. This term refers to the cumulative burden of chronic stress and life events on an individual’s health. When stressors exceed a person’s ability to cope, allostatic overload results. During allostatic overload, the body is challenged with the tools it has available to alter or modulate the affected biochemical pathways. Optimal nutrient status is necessary to overcome allostatic overload. Educating patients to preserve homeostasis in the face of seen and unseen insults to the preservation of their body is at the heart of naturopathic medicine.
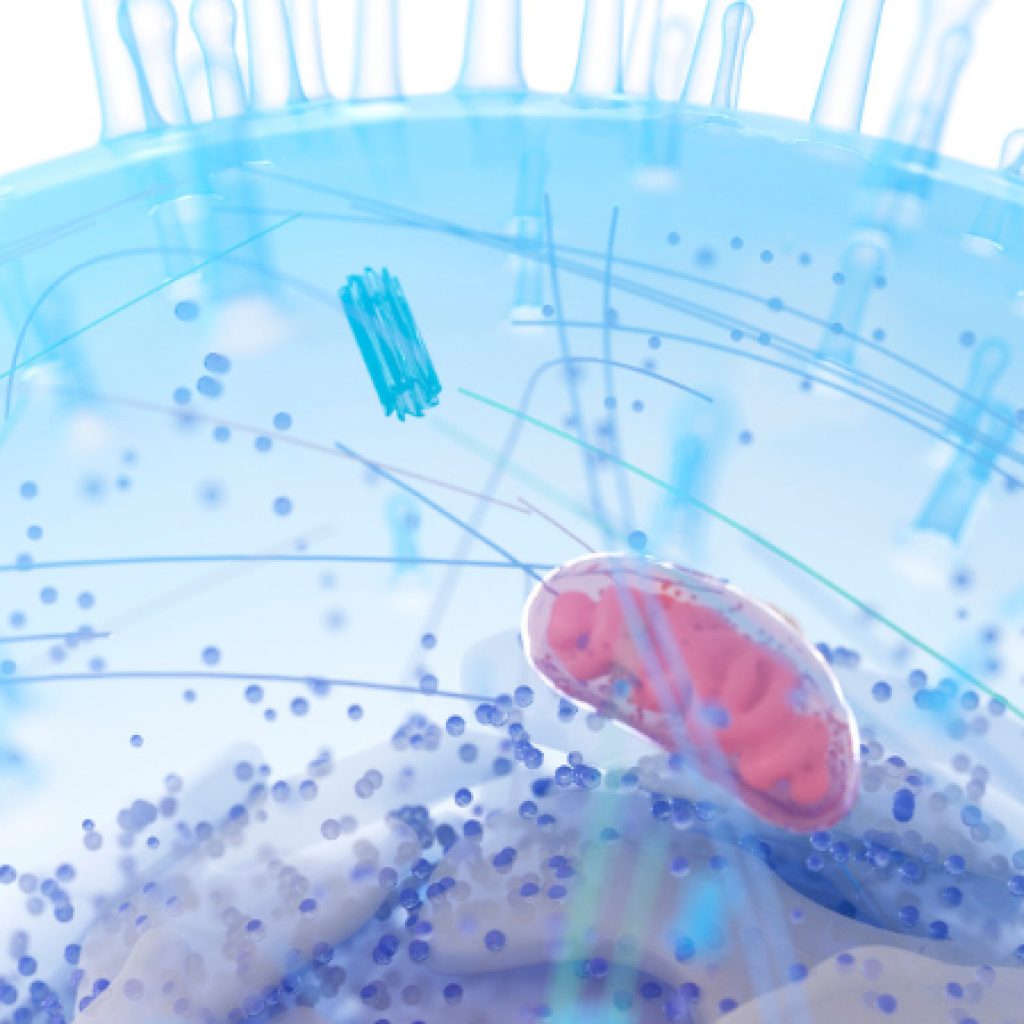
The Critical Role of the Mitochondria
Nutrient deficiencies and insufficiencies and allostatic overload can negatively impact the health of the mitochondria, which can lead to neuropathic pain. This is an important point that I addressed in last year’s NDNR article on neuropathic pain.7 I believe this is such a critical aspect of managing neuropathic pain that it is important to circle back to it.
Because of their large surface area, neurons require plenty of energy to maintain their membrane potential.8 Mitochondrial dysfunction leads to reduced aerobic capacity to meet the neuron’s energy demand.9 Over time, mitochondrial dysfunction spawns neuronal and axonal degeneration.9
Evidence indicates that mitochondrial damage due to issues like trauma, chemotherapy, hyperglycemia, and infection with HIV plays a critical role in the development of neuropathy in these conditions.10 Mitochondrial oxidative phosphorylation is a key player in ATP synthesis in neuronal cells, responsible for generating more than 90% of the ATP required for normal cellular function. Consequently, mitochondrial dysfunction can pave the way for a variety of different neuropathies. For example, mitochondrial impairment of neuronal cells is an important factor in the development of chemotherapy-induced peripheral neuropathy due to the induction of nitro-oxidative stress.11 In this type of neuropathy, the mitochondria are unable to generate enough ATP to fuel neuronal actions with high-energy demands.12
Mitochondrial impairment is also involved in diabetic neuropathy, and specifically implicated in damage to dorsal root ganglion neurons, axons, and Schwann cells.13-15 Impaired glucose metabolism in diabetes leads to suppression of mitochondrial oxidative phosphorylation, which can lead to neuropathy.13
Nicotinamide adenine dinucleotide (NAD+) plays a critical role in mitochondrial function. Unfortunately, NAD+ levels have been shown to fall during aging in experimental models of neurogenerative conditions, acute brain injury, obesity, and diabetes.16,17-19 In diabetic peripheral neuropathy, a pathway dependent upon NAD+ is impaired.20 Furthermore, several animal studies have found that declining NAD+ levels result in the axonal degeneration that occurs in peripheral neuropathy.21
Case Study: Resolving Cranial Neuropathy
At our annual family picnic, a relative came to the function with a patch over his right eye. Because he was in his mid-50s and had a history of diabetes, I wondered what was going on. I figured he had possibly injured his eye. With my inquisitive doctor hat on, I asked what was wrong with his eye. He reported that he had gone to an ophthalmologist, as he was experiencing double vision. The proposed solution was to wait and see if his vision returned to normal. The patch was to control the diplopia.
His history was positive for metformin use for the diabetes. He was taking no other medications and had no hypertensive issues. He was a strict vegetarian and walked more than 5 miles a day at his job. A strict, yet not-strategically-balanced vegetarian diet put this patient at a higher risk of B12 insufficiency. Metformin, which is also linked to vitamin B12 deficiency, may have compounded the problem.26
Not being satisfied with the concept of wait-and-see, I was more concerned than he was, so I jumped into the scientific research. Cranial nerve neuropathy fit his clinical picture well.27 This suspicion was confirmed when my wife shared with me that when he was a young man, he also had Bell’s palsy on the same side as the eye that was currently giving him trouble. Coincidence was possible, yet his presentation potentially pointed to susceptibility to neuropathy. I suspected cranial nerve III involvement, especially given his other clinical presentations that included ptosis (droopy eyelid).
I proposed that he try 600 mg alpha-lipoic acid twice a day, 5 000 mcg sublingual vitamin B12 daily, and a co-enzymatic B complex daily. I provided all these supplements to him at no charge, as he did not believe in natural medicine and that was a barrier to this therapeutic trial. I would have liked to have also included NR in his regimen, but because of his skepticism toward dietary supplements, I wanted to keep it simple.
Within 6 weeks of taking the supplements, his vision had returned to normal, and his eye exam was within normal range. His eye may have just returned to normal function with the passage of time, per his doctor’s wait-and-see recommendation. Regardless, he was happy to see again, as he had a long daily commute to work. He discontinued the supplements, and within 7 months his double vision returned. When I provided him the same gifted array of supplements, his vision returned to normal again. At that juncture, he was sold on the concept that the supplements could be working. At the very least, his doctor said the supplements would not hurt him, so he ultimately purchased them himself. Since then, his double vision has not returned.
The reality is that a single clinical case does not validate a therapeutic approach. So let’s look at the scientific literature.
Dietary Supplement Solutions for Neuropathic Pain
Nicotinamide Riboside
A particularly effective way to restore mitochondrial health is through the support of healthy NAD+ levels using nicotinamide riboside (NR). This unique form of vitamin B3 is an NAD+ precursor that has been shown to raise NAD+ levels in humans.22,23 Evidence from animal studies indicates NR can prevent and reverse diabetic peripheral neuropathy, as well as neuropathy in prediabetes.20,21 Results of 2 rodent studies indicate NR is useful in other forms of neuropathy. These studies found NR inhibited chemotherapy-induced peripheral neuropathy caused by the chemotherapy drug paclitaxel.24,25 When NR was administered as 200 mg/kg starting a week before the start of paclitaxel treatment and continued for another 24 days, NR suppressed the development of tactile hypersensitivity.24 NR treatment led to a 50% increase in blood levels of NAD+, and it did not interfere with the effects of paclitaxel.
Alpha-Lipoic Acid
I chose to use alpha-lipoic acid in my relative with cranial neuropathy (see case study) because this antioxidant has much scientific support for its general use in neuropathy. A study of 46 patients with type 1 diabetes and different forms of autonomic neuropathy found that 600 mg of alpha-lipoic acid administered intravenously for 10 days and by tablet for 50 days led to improvement in different forms of autonomic diabetic neuropathy.28
A meta-analysis of 4 trials including 1 258 patients given either placebo or 600 mg of alpha-lipoic acid per day administered intravenously concluded that alpha-lipoic acid “significantly improves both positive neuropathic symptoms and neuropathic deficits to a clinically meaningful degree in diabetic patients with symptomatic polyneuropathy.”29
Vitamin B12
Vitamin B12 is another nutrient known to ameliorate neuropathy, supported by numerous human trials. It may improve symptoms of neuropathy because it is involved in nerve repair and myelination.30 A prospective, double-blind, placebo-controlled trial investigated the use of vitamin B12 in 90 patients with type 2 diabetes.31 The patients had been taking metformin for at least 4 years and their B12 levels were less than 400 pmol/L. Subjects included in the study had both peripheral and autonomic diabetic neuropathy. They were randomized to receive 1 mg of oral methylcobalamin for 12 months (44 patients) or a placebo (46 patients). The study found that plasma B12 levels increased and all neurophysiological parameters, sudomotor function, pain score, and quality of life improved.
Furthermore, a systematic review of vitamin B12, methylcobalamin, or a placebo in painful diabetic neuropathy included 6 randomized controlled trials assessing pain or sensation-related symptoms (such as paresthesia).31 In those studies, B12 and methylcobalamin significantly improved the somatosensory or neuropathic pain symptoms compared with placebo.
There’s indication that vitamin B12 and alpha-lipoic acid each address different symptoms of neuropathy. A study found that neuropathy, as measured by the Toronto Clinical Neuropathy Scoring System (TCSS), total symptom score (TSS), and visual analog scale (VAS) of positive symptoms, was significantly reduced by both vitamin B12 and alpha-lipoic acid.32 However, ALA led to significantly greater reductions in burning and pain while methylcobalamin reduced numbness and paresthesia VAS scores to a slightly greater extent than ALA. Methylcobalamin also reduced abnormal (low-response) points for pressure and pinprick sensation, while ALA had no effect in this area. Both interventions led to a pronounced reduction in vibratory perception threshold.
Other B Vitamins
Other B vitamins, sometimes in combination with vitamin B12, can support nerve health. For example, a mixture of vitamins B1, B6, and B12 improved tactile allodynia in diabetic rats.33 In that same study, vitamin B6 improved sensory nerve conduction, suggesting that B complex vitamins have a role in suppressing pain from diabetic neuropathy. In another study, a combination of the biologically active form of folate, vitamin B12, and vitamin B6 was studied in a randomized controlled trial of 214 patients with diabetic neuropathy.1 Significant improvement occurred based on the Neuropathy Total Symptom Score questionnaire given at 16 weeks.
Also of note is that folate has been used for the treatment of neuropathy as early as the 1970s.34,35 Folate has attracted interest as an agent to address neuropathic pain since it plays an important role in methylation in the nervous system.1
The Role of Genetic Polymorphisms
Genetic polymorphisms (single nucleotide polymorphisms or SNPs) would appear to further delineate dosing of supplements such as B vitamins. Methylenetetrahydrofolate reductase (MTHFR) polymorphisms, which frequently occur in relationship to folate metabolism, are a well-known and readily tested SNP. This indicates the importance of testing to determine the presence or absence of these SNPs before patients begin their regimen. Patients with MTHFR polymorphisms should always be given 5-methylenetetrahydrofolate – the biologically active form of folate.
Zinc
Zinc plays a role in the activation of more than 300 genes involved in macromolecule and protein synthesis and cell growth and proliferation.1 Zinc has anti-inflammatory properties that explain its ability to reduce pain.1 Inflammation is a trigger of chronic pain, including that caused by neuropathy. In a rat model of neuropathic pain, zinc caused a pronounced reduction in inflammatory hyperalgesia.36 In another study of rats with sciatic nerve damage, zinc led to a dose-dependent decline in thermal hyperalgesia.37
Magnesium
Magnesium is beneficial in neuropathy caused by various conditions. These include diabetic neuropathy, cancer-related neuropathic pain, chemotherapy-induced neuropathy, and PHN.38 Magnesium blocks the N-methyl-D-aspartate (NMDA) receptor, which is involved in the origin of neuropathic pain.39 Some treatments for neuropathic pain target this receptor because NMDA has been found in rodent studies to play a role in central sensitization and many physiological processes in the central and peripheral nervous systems.39,40 This points to the potential usefulness of magnesium as a pain inhibitor via blockage of the NMDA receptor.1
Magnesium’s ability to resolve neuropathic pain has been studied in humans. For example, in a randomized controlled trial, 80 patients with chronic lower back pain that had a neuropathic component were given either a placebo or an intravenous (IV) magnesium infusion for 2 weeks followed by oral magnesium capsules for another 4 weeks.41 The 40 patients in the magnesium group experienced reduced pain intensity compared to the 40 patients given the placebo. In another study of patients with PHN, IV magnesium reduced neuropathic pain in the short term, although not over the long term.42 IV administration of magnesium may overcome absorption issues and more effectively achieve high blood levels of this mineral.
Vitamin D
There is a relationship between vitamin D deficiency and chronic pain syndromes such as chronic widespread pain, which has many of the same pathophysiological and clinical attributes as neuropathic pain.1
Vitamin D may alleviate pain due to its role in the regulation of inflammatory cytokines,43 a relationship that has been shown in patients with diabetic neuropathy.44 Researchers have investigated the effect of raising vitamin D levels in patients with diabetic neuropathy. A prospective study of 143 patients with diabetic neuropathy found that a single dose of intramuscular high-dose vitamin D (600 000 IU) led to a pronounced reduction of pain.45 In a randomized, controlled trial, 57 patients with diabetic neuropathy and low vitamin D levels received either 300 000 IU of vitamin D or a placebo through intramuscular injections.46 Pain scores were significantly reduced in patients given vitamin D compared with placebo.
Curcumin
Curcumin is a botanical compound derived from the spice turmeric (Curcuma longa). Curcumin has anti-inflammatory properties that may make it useful in neuropathic pain. It has been shown to reduce thermal hyperalgesia in a mouse model of diabetic neuropathy.47 In rats with sciatic nerve injury, administration of curcumin soon after nerve damage led to a greater resolution of mechanical allodynia after 7 days compared with placebo, indicating that curcumin may prevent the progression of neuropathic pain to chronic pain after the initial nerve injury.48
Emerging research in humans indicates curcumin could hold promise in alleviating neuropathy. In a randomized, controlled trial, 141 patients were given a formula that contained either 1) curcumin phytosome, piperine (to improve curcumin absorption), and lipoic acid as an adjunct to the nonsteroidal anti-inflammatory drug (NSAID) dexibuprofen, or 2) dexibuprofen alone.49 The patients suffered from neuropathic pain, primarily chronic back pain. Patients given the curcumin formula along with the NSAID experienced a pronounced reduction in neuropathic pain compared with dexibuprofen alone. Patients given curcumin with the NSAID were also able to significantly reduce their dosage of the drug.
Why Stand-Alone Nutrients Often Don’t Work
When implementing a dietary supplement regimen in patients with neuropathic pain, it is helpful to remember that employing stand-alone supplements is often not an effective strategy. As we know from the scientific literature, multiple nutrients (vitamins and/or minerals) are often needed to nudge or block a biochemical pathway. Thus, using a standalone intervention of a nutrient like magnesium can fall short of perceived clinical impact. Beyond the limitations of single nutrient parameters, it is well documented that select vitamins and minerals are not all equally bioavailable. Indeed, not even all magnesium is created equal relative to bioavailability or tolerance, and gastrointestinal health of the patient can also impact absorption capacity.
Lastly, there are multiple pathways for pain to manifest, and various cytokines and other factors can affect how quickly a patient will heal. For example, how long will it take for a patient to become nutritionally replete from supplementation? How long will it take for pain to quiet “chatter” at the cellular level so that resolution can be achieved? How many cells in a neuropathic limb must quiet to diminish pain? Each of these issues will contribute to the difference between patients and their healing capacity and speed.
Conclusion
Neuropathic pain is a common complaint of many patients, especially those with diabetes or shingles or individuals who have undergone chemotherapy. My experience in clinical practice mirrors evidence seen in the scientific literature with nutrients such as nicotinamide riboside, alpha-lipoic acid, vitamin B12, other B vitamins, zinc, magnesium, and curcumin providing beneficial effects. While neuropathy is a substantial burden to patients who are suffering from this condition, there is hope that pain related this condition will resolve with the use of these nutrients.
[REFS]
- Abdelrahman KM, Hackshaw KV. Nutritional Supplements for the Treatment of Neuropathic Pain. Biomedicines. 2021;9(6).
- Jones MR, Urits I, Wolf J, et al. Drug-Induced Peripheral Neuropathy: A Narrative Review. Curr Clin Pharmacol. 2020;15(1):38-48.
- Bansal V, Kalita J, Misra UK. Diabetic neuropathy. Postgrad Med J. 2006;82(964):95-100.
- Pirart J. [Diabetes mellitus and its degenerative complications: a prospective study of 4,400 patients observed between 1947 and 1973 (3rd and last part) (author’s transl)]. Diabete Metab. 1977;3(4):245-256.
- Nalamachu S, Morley-Forster P. Diagnosing and managing postherpetic neuralgia. Drugs Aging. 2012;29(11):863-869.
- Yawn BP, Saddier P, Wollan PC, et al. A population-based study of the incidence and complication rates of herpes zoster before zoster vaccine introduction. Mayo Clin Proc. 2007;82(11):1341-1349.
- Meletis CD. Peripheral neuropathy: taking the edge off. Naturopathic Doctor News & Review. 2021;17(7).
- Sasaki Y. Metabolic aspects of neuronal degeneration: From a NAD(+) point of view. Neurosci Res. 2019;139:9-20.
- Chandrasekaran K, Najimi N, Sagi AR, et al. NAD(+) Precursors Repair Mitochondrial Function in Diabetes and Prevent Experimental Diabetic Neuropathy. Int J Mol Sci. 2022;23(9).
- Khuankaew C, Sawaddiruk P, Surinkaew P, et al. Possible roles of mitochondrial dysfunction in neuropathy. Int J Neurosci. 2021;131(10):1019-1041.
- Ma J, Kavelaars A, Dougherty PM, et al. Beyond symptomatic relief for chemotherapy-induced peripheral neuropathy: Targeting the source. Cancer. 2018;124(11):2289-2298.
- Bennett GJ, Doyle T, Salvemini D. Mitotoxicity in distal symmetrical sensory peripheral neuropathies. Nat Rev Neurol. 2014;10(6):326-336.
- Chandrasekaran K, Anjaneyulu M, Inoue T, et al. Mitochondrial transcription factor A regulation of mitochondrial degeneration in experimental diabetic neuropathy. Am J Physiol Endocrinol Metab. 2015;309(2):E132-141.
- Fernyhough P. Mitochondrial dysfunction in diabetic neuropathy: a series of unfortunate metabolic events. Curr Diab Rep. 2015;15(11):89.
- Sifuentes-Franco S, Pacheco-Moisés FP, Rodríguez-Carrizalez AD, et al. The Role of Oxidative Stress, Mitochondrial Function, and Autophagy in Diabetic Polyneuropathy. J Diabetes Res. 2017;2017:1673081.
- Chandrasekaran K, Salimian M, Konduru SR, et al. Overexpression of Sirtuin 1 protein in neurons prevents and reverses experimental diabetic neuropathy. Brain. 2019;142(12):3737-3752.
- Chandrasekaran K, Choi J, Arvas MI, et al. Nicotinamide Mononucleotide Administration Prevents Experimental Diabetes-Induced Cognitive Impairment and Loss of Hippocampal Neurons. Int J Mol Sci. 2020;21(11).
- Fang EF, Lautrup S, Hou Y, et al. NAD(+) in Aging: Molecular Mechanisms and Translational Implications. Trends Mol Med. 2017;23(10):899-916.
- Yoshino J, Baur JA, Imai SI. NAD(+) Intermediates: The Biology and Therapeutic Potential of NMN and NR. Cell Metab. 2018;27(3):513-528.
- Chandrasekaran K, Anjaneyulu M, Choi J, et al. Role of mitochondria in diabetic peripheral neuropathy: Influencing the NAD(+)-dependent SIRT1-PGC-1α-TFAM pathway. Int Rev Neurobiol. 2019;145:177-209.
- Trammell SA, Weidemann BJ, Chadda A, et al. Nicotinamide Riboside Opposes Type 2 Diabetes and Neuropathy in Mice. Sci Rep. 2016;6:26933.
- Martens CR, Denman BA, Mazzo MR, et al. Chronic nicotinamide riboside supplementation is well-tolerated and elevates NAD(+) in healthy middle-aged and older adults. Nat Commun. 2018;9(1):1286.
- Airhart SE, Shireman LM, Risler LJ, et al. An open-label, non-randomized study of the pharmacokinetics of the nutritional supplement nicotinamide riboside (NR) and its effects on blood NAD+ levels in healthy volunteers. PLoS One. 2017;12(12):e0186459.
- Hamity MV, White SR, Walder RY, et al. Nicotinamide riboside, a form of vitamin B3 and NAD+ precursor, relieves the nociceptive and aversive dimensions of paclitaxel-induced peripheral neuropathy in female rats. Pain. 2017;158(5):962-972.
- Hamity MV, White SR, Blum C, et al. Nicotinamide riboside relieves paclitaxel-induced peripheral neuropathy and enhances suppression of tumor growth in tumor-bearing rats. Pain. 2020;161(10):2364-2375.
- Chapman LE, Darling AL, Brown JE. Association between metformin and vitamin B(12) deficiency in patients with type 2 diabetes: A systematic review and meta-analysis. Diabetes Metab. 2016;42(5):316-327.
- Jilani MH, Iqbal H, Huda S, et al. Double Vision: Isolated Third Cranial Nerve Palsy After Cardiac Catheterization. Cureus. 2020;12(7):e9202.
- Tankova T, Koev D, Dakovska L. Alpha-lipoic acid in the treatment of autonomic diabetic neuropathy (controlled, randomized, open-label study). Rom J Intern Med. 2004;42(2):457-464.
- Ziegler D, Nowak H, Kempler P, et al. Treatment of symptomatic diabetic polyneuropathy with the antioxidant alpha-lipoic acid: a meta-analysis. Diabet Med. 2004;21(2):114-121.
- Didangelos T, Karlafti E, Kotzakioulafi E, et al. Vitamin B12 Supplementation in Diabetic Neuropathy: A 1-Year, Randomized, Double-Blind, Placebo-Controlled Trial. Nutrients. 2021;13(2).
- Sun Y, Lai MS, Lu CJ. Effectiveness of vitamin B12 on diabetic neuropathy: systematic review of clinical controlled trials. Acta Neurol Taiwan. 2005;14(2):48-54.
- Han Y, Wang M, Shen J, et al. Differential efficacy of methylcobalamin and alpha-lipoic acid treatment on symptoms of diabetic peripheral neuropathy. Minerva Endocrinol. 2018;43(1):11-18.
- Jolivalt CG, Mizisin LM, Nelson A, et al. B vitamins alleviate indices of neuropathic pain in diabetic rats. Eur J Pharmacol. 2009;612(1-3):41-47.
- Botez MI, Peyronnard JM, Bachevalier J, et al. Polyneuropathy and folate deficiency. Arch Neurol. 1978;35(9):581-584.
- Manzoor M, Runcie J. Folate-responsive neuropathy: report of 10 cases. Br Med J. 1976;1(6019):1176-1178.
- Safieh-Garabedian B, Poole S, Allchorne A, et al. Zinc reduces the hyperalgesia and upregulation of NGF and IL-1 beta produced by peripheral inflammation in the rat. Neuropharmacology. 1996;35(5):599-603.
- Liu T, Walker JS, Tracey DJ. Zinc alleviates thermal hyperalgesia due to partial nerve injury. Neuroreport. 1999;10(7):1619-1623.
- Na HS, Ryu JH, Do SH. The role of magnesium in pain. In: Vink R, Nechifor M, eds. Magnesium in the Central Nervous System. Adelaide (AU): University of Adelaide Press; 2011.
- Zhou HY, Chen SR, Pan HL. Targeting N-methyl-D-aspartate receptors for treatment of neuropathic pain. Expert Rev Clin Pharmacol. 2011;4(3):379-388.
- Xu X, Tao X, Huang P, et al. N-methyl-d-aspartate receptor subunit 2B on keratinocyte mediates peripheral and central sensitization in chronic post-ischemic pain in male rats. Brain Behav Immun. 2020;87:579-590.
- Yousef AA, Al-deeb AE. A double-blinded randomised controlled study of the value of sequential intravenous and oral magnesium therapy in patients with chronic low back pain with a neuropathic component. Anaesthesia. 2013;68(3):260-266.
- Brill S, Sedgwick PM, Hamann W, et al. Efficacy of intravenous magnesium in neuropathic pain. Br J Anaesth. 2002;89(5):711-714.
- Straube S, Andrew Moore R, Derry S, McQuay HJ. Vitamin D and chronic pain. Pain. 2009;141(1-2):10-13.
- Bilir B, Tulubas F, Bilir BE, et al. The association of vitamin D with inflammatory cytokines in diabetic peripheral neuropathy. J Phys Ther Sci. 2016;28(7):2159-2163.
- Basit A, Basit KA, Fawwad A, et al. Vitamin D for the treatment of painful diabetic neuropathy. BMJ Open Diabetes Res Care. 2016;4(1):e000148.
- Sari A, Akdoğan Altun Z, Arifoglu Karaman C, et al. Does Vitamin D Affect Diabetic Neuropathic Pain and Balance? J Pain Res. 2020;13:171-179.
- Sharma S, Kulkarni SK, Agrewala JN, et al. Curcumin attenuates thermal hyperalgesia in a diabetic mouse model of neuropathic pain. Eur J Pharmacol. 2006;536(3):256-261.
- Jeon Y, Kim CE, Jung D, et al. Curcumin could prevent the development of chronic neuropathic pain in rats with peripheral nerve injury. Curr Ther Res Clin Exp. 2013;74:1-4.
- Di Pierro F, Settembre R. Safety and efficacy of an add-on therapy with curcumin phytosome and piperine and/or lipoic acid in subjects with a diagnosis of peripheral neuropathy treated with dexibuprofen. J Pain Res. 2013;6:497-503.

Chris D. Meletis, ND is an educator, international author, and lecturer. He has authored 18 books and more than 200 scientific articles in prominent journals and magazines. Dr Meletis served as Dean of Naturopathic Medicine and CMO for 7 years at NUNM. He was recently awarded the NUNM Hall of Fame award by OANP, as well as the 2003 Physician of the Year by the AANP. Dr Meletis spearheaded the creation of 16 free natural medicine healthcare clinics in Portland, OR. Dr Meletis serves as an educational consultant for Fairhaven Health, Berkeley Life, TruGen3, US BioTek, and TruNiagen. He has practiced in Beaverton, OR, since 1992.