Rian Shah, ND
About 70% of my practice consists of people in menopause or andropause. Insomnia is usually one of their chief complaints at our initial visit. There are many for whom insomnia has been a lifelong problem, and there are also many women whose insomnia started around perimenopause. The focus of this article will be to discuss the treatment of insomnia and disordered sleep in the aging population.
As we know, aging is not just the decline of tissue turgor and memory and bone density. It starts with the slow unwinding of the hormonal symphony that is the infrastructure by which our body is supported. If we look deeply enough, we will find that most of our aging patients with recent-onset insomnia are dealing with significant hormone imbalance.
Aging and Sleep
While hormones are a huge part of the picture in aging, there is so much to be said about the emotional states of aging individuals. Many are dealing with the close of their lifelong career, divorces, children going off to college, mid-life crises. For many, their stress is just higher than before; thus, supporting stress overall, as well as proper sleep hygiene, is crucial. Since this article is meant to help guide us with those patients who never come in with the singular complaint of insomnia (well, they may initially, but after our first 1-hour office visit, we usually discover about 10 other issues), I will present the bulk of this information in a case format. Patients can be very complicated.
The Case Study of Anna
Anna, a 52-year-old postmenopausal mother of 3, still works full-time and has recently divorced from her husband after 30 years of marriage. She has a teenager still living at home, and her other 2 children are off at college. She is stressed out and still dealing with heartbreak and situational depression that comes with making the decisions she has lately had to make.
Chief Complaints
Anna’s chief complaints include insomnia, hot flashes, restless legs, night sweats, fatigue, and depression. Her insomnia started about 6 years ago, which also happens to be when her periods started changing. This also correlates with her starting dessicated thyroid for her subclinical hypothyroidism, prescribed by a naturopathic physician. She has not had her thyroid function checked in about 3 years, but has maintained her dose of 1 grain per day. She is not on any other medications, she has not been taking her supplements, and she hasn’t been exercising, as she can’t seem to find the energy to go to the gym. She is feeling apathetic and is disinterested in her friends and family or going to social gatherings.
Assessment
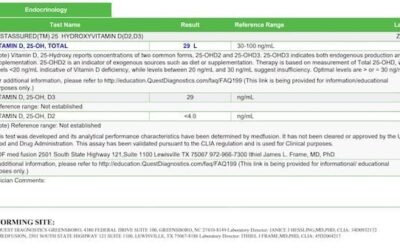
I start with a full blood draw. We look at the following, to evaluate her current hormone balance and to see whether the dessicated thyroid is correctly dosed: CBC, CMP, vitamin D, vitamin B12, pregnenolone, DHEA-S, estradiol, progesterone, and free testosterone. We also check TSH, free T3, free T4, iron, and ferritin.
We’re firm about looking at her vitamin D level, even though it is not covered by most insurance. This is because vitamin D deficiency is our #1 nutrient deficiency, also because vitamin D is a pro-hormone that is responsible for building the hormonal symphony in the body. We check vitamin B12 because we know that B12 deficiency is often a good marker for the other B vitamins, and that B vitamins are critical cofactors in our stress pathways. We look at ferritin because low ferritin (low iron) is a common cause of restless legs.
We ask Anna to provide a diet diary for 3 days and bring it to her next appointment. She agrees.
First Follow-up
A few days later, we get the blood results back (Table 1). (I am only reporting the significant values that may be contributing to her insomnia, simply to stay focused on the topic of this paper):
Table 1. Baseline Lab Results
| Biomarker (serum) | Result | Normal Range |
| Pregnenolone | 20 ng/dL | 13-111 ng/dL |
| DHEA-S | 64 µg/dL | 45-320 µg/dL |
| Estradiol | 10 pg/mL | <31 pg/mL (menopausal range) |
| Progesterone | <0.1 ng/mL | <0.5 ng/mL (menopausal range) |
| Free Testosterone | <0.1 pg/mL | 0.1-6.4 pg/mL |
| 25(OH)-vitamin D | 30 ng/mL | 30-100 ng/mL |
| Vitamin B12 | 353 pg/mL | 231-931 pg/mL |
| Ferritin | 14 ng/mL | 17.9-464 ng/mL |
| Iron | 64 µg/dL | 30-180 µg/dL |
| TSH | <0.02 µIU/mL | 0.45-4.5 µIU/mL |
| Free T4 | 0.9 ng/dL | 0.8-1.8 ng/dL |
| Free T3 | 6.7 pg/mL | 2.3-4.2 pg/mL |
There are a few things to keep in mind here, eg, normal vs optimal, and what might be the deepest cause (per blood info only) of the imbalance. Given that the patient is in menopause, we would expect to see such low values for estrogen, testosterone and progesterone. This is probably why she is having the night sweats – one of the factors keeping her from a full night’s rest. But what about pregnenolone and DHEA? Why are these included? In my experience, you cannot balance the other hormones without first addressing pregnenolone and DHEA. This is because they are pro-hormones that help to make our estrogen, progesterone, and testosterone. I believe that pregnenolone deficiency in our aging population is also one of the main reasons for shallow, difficult sleep. This is because pregnenolone supports the stress pathway by serving as a precursor to DHEA and progesterone.
Moreover, from a treatment standpoint, it has been shown in an animal model that pregnenolone increases brain levels of acetylcholine,1 a key neurotransmitter required for optimal brain function and deep sleep. Acetylcholine is not only vital for cognition and memory; it is also involved in controlling sleep cycles, especially the phase of sleep that is associated with memory (called paradoxical sleep, or the random eye movement [REM] phase). Scientists have used this knowledge to study the effects of pregnenolone on sleep cycles and discovered that it dramatically increases memory-enhancing sleep.2
A pregnenolone of 20 ng/dL is normal, but not optimal. For optimal sleep that is both deep and restorative, and to properly balance DHEA, I have found that achieving a pregnenolone level of 50-80 ng/dL is best. It is imperative that patients take pregnenolone at night before bed. I like to start with 10 mg, as the effects are dose-dependent and too much pregnenolone can stimulate the cortisol pathway too much, disrupting sleep.
By supporting pregnenolone, we can also affect progesterone by increasing it at night when it is most needed. Why is low progesterone related to insomnia? Because low progesterone equates to lower levels of allopregnanolone – a breakdown product of progesterone that helps block anxiety by increasing GABA receptor activity levels and increasing a sense of calm.3
DHEA is an important hormone to consider as well, since DHEA, produced from pregnenolone, induces a significant increase in REM sleep. DHEA helps to neutralize cortisol’s immune-suppressant effect, thereby improving resistance to disease. (Cortisol and DHEA are inversely proportional to each other; when one is up, the other tends to go down.) This is an important consideration in Anna’s case, as she is under a lot of stress, with presumably high cortisol. We know that a DHEA-S level of 64 µg/dL is normal, but in my clinical experience, optimal is closer to 120. Supplemental DHEA should be taken in the morning when DHEA is naturally more active in the body. I like to start with a dose of 10 mg. Most women do not need much, and many come to me on 25 mg or higher. These women often have acne, hair loss, and headaches at that level, which are most likely related to DHEA’s conversion to testosterone. So, again, less is more.
Anna’s low ferritin level could be an indication that her restless legs syndrome is caused by low iron. Since she is postmenopausal and hasn’t had a period in about 3 years, this is concerning. She also informs me that she has not had a colonoscopy.
Vitamin D is far too low at 30 ng/mL. An optimal level is 70-90. While we don’t know for sure if vitamin D directly affects sleep, we do know that low vitamin D can increase anxiety and depression,4 either of which can negatively impact sleep.
Let’s talk about her thyroid panel… She is currently taking 1 grain per day of dessicated thyroid, and has been for about 6 years. She hasn’t had it measured in many years and can’t remember the last time she did, but is still able to get refills from her doctor. Her TSH at this level is far too suppressed. Levels below 0.4 µIU/mL usually go along with compromised bone density. Her free T3 is much higher than her free T4, suggesting that her thyroid hormone may not be dosed correctly, and may not be the proper medication, to begin with. It seems that she might be rapidly converting thyroid from T4 to T3. This dose needs to reassessed as a possible contributing factor to her insomnia, as well as her anxiety.
As I said, it’s complicated!
One Week Later
Anna comes back a week later with her food diary. She is drinking coffee in the morning – 2 cups, black. No breakfast. For lunch, she grabs a bagel or sometimes a salad, or whatever she can find. For dinner, she is cooking for herself and her son – usually a meat, and vegetable, and rolls or some other form of carbohydrate. She has a scoop of ice cream before bed each night. She is not drinking water at all. We need to look at food sensitivities, but in an effort to not overwhelm, we decide to file that away as Plan B.
We talk about her labs and her complaints and how they relate, as well as food and lifestyle. We suggest the following…
Plan
Nutrition: Avoid gluten, dairy, and almonds for 4 weeks, as these are the 3 foods that, in my clinical experience, come back the most often with elevated IgG antibodies. Focus on veggies and protein, and restrict eating within 2 hours of bedtime. One cup of coffee in the morning is probably fine.
We decide to discuss food sensitivity on the next visit. Anna is advised against reintroducing foods until we talk again.
Supplementation:
- Multivitamin with iron
- Extra iron and vitamin C, BID
- 10 000 IU vitamin D3 for 4 weeks, then reduce to 5000 IU/day
- Methyl-B12 sublingually, 5000 µg/day
- DHEA, 10 mg each morning
- Pregnenolone, 30 mg at night
- Dessicated thyroid, 0.5 grain per day (half of her previous dose)
- Effervescent magnesium malate/citrate in water, at night
Follow-up: We agreed to follow up in 4 weeks with a blood draw, followed by an office visit to review abnormal lab findings and to determine whether the treatment plan is working to improve her sleep.
One Month Later
Four weeks later, Anna comes back smiling. Her hot flashes are gone and she is sleeping deeply for the first time in a long time. Her restless legs syndrome has disappeared, her mood is lifted, and her energy during the day is much improved. She is dreaming and remembers her dreams vividly.
Her food challenge has been fine. It was hard at first, but she consulted our nutritionist on staff and was given breakfast/lunch/dinner suggestions for 4 weeks, which were easy. She has not yet reintroduced foods.
When we look at her blood work, we see several changes (Table 2).
Table 2. Follow-up Lab Results
| Biomarker (serum) | New Result | Prior Result | Normal Range |
| Prenenolone | 87 ng/dL | 20 ng/dL | 13-111 ng/dL |
| DHEA-S | 120 µg/dL | 64 µg/dL | 45-320 µg/dL |
| Estradiol | 20 pg/mL | 10 pg/mL | <31 pg/mL |
| Progesterone | 1.1 ng/mL | <0.1 ng/mL | <0.5 ng/mL |
| Free Testosterone | 1.6 pg/mL | <0.1 pg/mL | 0.1-6.4 pg/mL |
| 25(OH)-vitamin D | 86 ng/mL | 30 ng/mL | 30-100 ng/mL |
| Vitamin B12 | >1000 pg/mL | 353 pg/mL | 231-931 pg/mL |
| Ferritin | 24 ng/mL | 14 ng/mL | 17.9-464 ng/mL |
| Iron | 86 µg/dL | 64 µg/dL | 30-180 µg/dL |
| TSH | 0.56 µIU/mL | <0.02 µIU/mL | 0.45-4.5 µIU/mL |
| Free T4 | 1.0 ng/dL | 0.9 ng/dL | 0.8-1.8 ng/dL |
| Free T3 | 5.0 pg/mL | 6.7 pg/mL | 2.3-4.2 pg/mL |
Her DHEA supplementation appears to have increased both her estradiol and testosterone, which is most likely why her night sweats are gone. Her pregnenolone level has come up nicely and has likely brought up her progesterone; the ratio between the two is now nicely balanced. TSH looks much better, which means she is at less risk of osteoporosis due to her thyroid medication being overdosed. Ferritin is still not at the target level of 60 ng/mL, but it’s much better and is most likely contributing to the restless legs syndrome disappearing.
We discuss food reintroduction, and she decides that she misses dairy the most, so will test it first. The next day she has dairy with breakfast, in her gluten-free cereal, and then has cheese on some gluten-free pasta at night with dinner. The next day she emails me and tells me that her sleep was much more restless that night and that she started developing gas and bloating. This was interesting to her because it wasn’t until the gas and bloating came back that she realized what a problem this had previously been for her.
Following the dairy, Anna reintroduced her other foods, and noticed nothing. She has decided to stay off of the dairy.
Closing Comments
Anna has now been a patient of mine for about 3 years, and she is doing great. She maintains a dairy- and gluten-free lifestyle, and sleeps well. She is off her restless legs syndrome medication, and has great energy and a renewed zest for life. Anna’s case is a great example of how a problem as complicated and intricate as insomnia, can be solved.
 Rian Shah, ND, maintains a practice (Cascade Integrative Medicine) in Issaquah, WA, specializing in anti-aging medicine, bio-identical hormone replacement, thyroid imbalance, and heart disease. She graduated in 2004 from Bastyr University and since then has worked for Doctors Data Laboratory, Longevity Medical Clinic, and in a collaborative practice with other specialties. When not seeing patients, she spends time in the mountains with her husband and their 2 young children. For more information, check her website at CascadeIntegrativeMedicine.com
Rian Shah, ND, maintains a practice (Cascade Integrative Medicine) in Issaquah, WA, specializing in anti-aging medicine, bio-identical hormone replacement, thyroid imbalance, and heart disease. She graduated in 2004 from Bastyr University and since then has worked for Doctors Data Laboratory, Longevity Medical Clinic, and in a collaborative practice with other specialties. When not seeing patients, she spends time in the mountains with her husband and their 2 young children. For more information, check her website at CascadeIntegrativeMedicine.com
References:
- Darnaudéry M, Koehl M, Piazza PV, et al. Pregnenolone sulfate increases hippocampal acetylcholine release and spatial recognition. Brain Res. 2000;852(1):173-179.
- Goepp JG. Enhancing Cognitive Function with Pregnenolone. November, 2007. Life Extension Magazine. LEF Web site. http://www.lef.org/magazine/2007/11/report_pregnenolone/Page-01. Accessed December 15, 2014.
- Reddy DS. Pharmacology of endogenous neuroactive steroids. Crit Rev Neurobiol. 2003;15(3-4):197-234.
- Maddock J, Berry DJ, Geoffroy MC, et al. Vitamin D and common mental disorders in mid-life: cross-sectional and prospective findings. Clin Nutr. 2013;32(5):758-764.