JARED L. ZEFF, ND, VNMI, LAC
The following is not an article prepared for a medical journal. Not every statement of fact is cited or referenced. This is a commentary on the medicine, a running set of observations about practice in the field. It’s not meant to be a peer-reviewed presentation; rather, these are notes and thoughts from a practicing naturopathic physician, a primary care doc in general practice.
A Challenging Disease
In my last submission, I described a basic prescribing strategy as I learned it from my primary mentor, Dr Harold Dick, of Spokane, WA. I used a case of multiple sclerosis (MS) as an example of this method in its application. We treated this young woman, her lesions decreased, and her symptoms improved in a rather short time. That made the treatment of MS seem almost trivial. MS can be a very difficult disease to treat. Like most health challenges, I have had some success with it, applying our basic therapeutics within the strategy I have outlined. But my success has not been universal. I want to go more deeply into this problem.
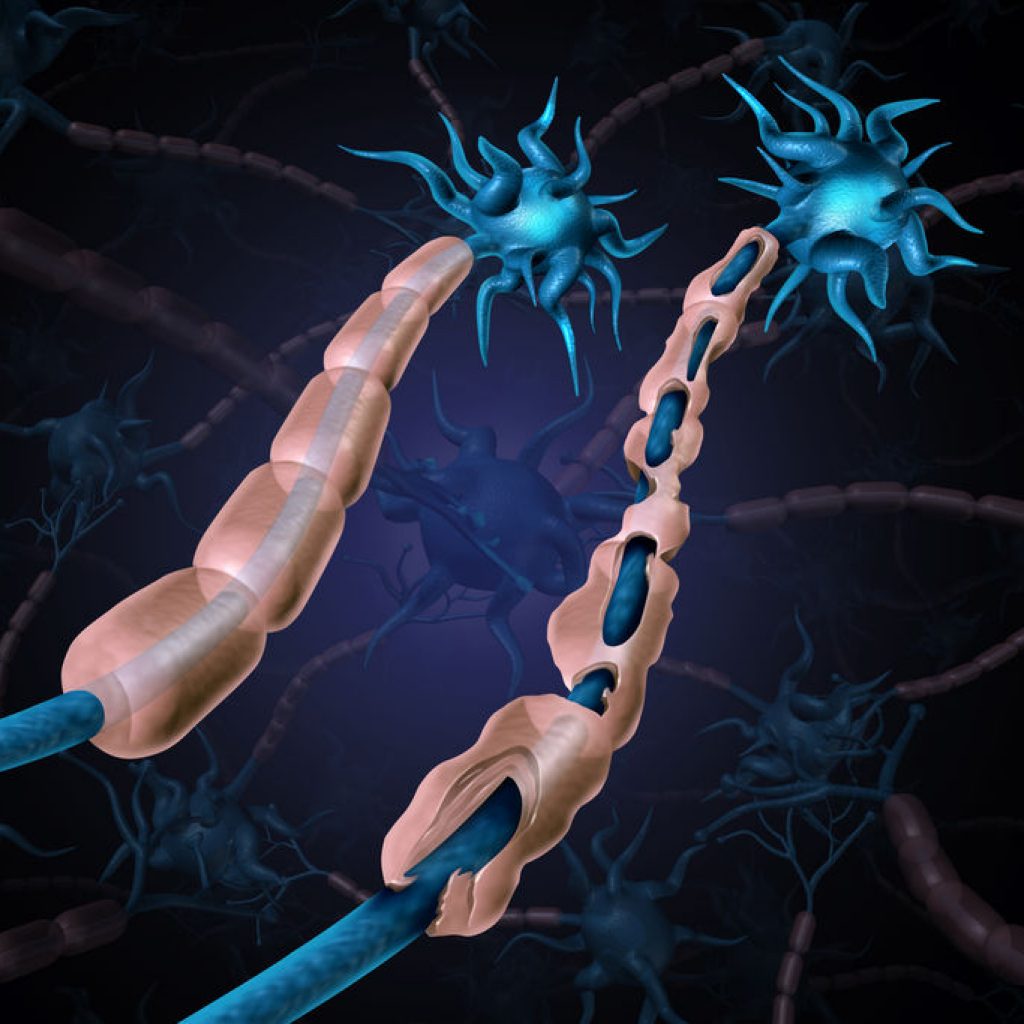
Multiple sclerosis is a disease manifestation of unknown cause. That is to say, there is no specific cause that has ever been identified, though in some cases one can trace the onset to an apparent cause or exciting event. MS does not have a single presentation. There are currently 4 types that are discussed in the literature: Primary Progressive (PPMS), Secondary Progressive (SPMS), Relapsing-Remitting (RRMS), and Clinically Isolated Syndrome (CIS).1 For the most part, these types describe the course of the disease. MS is defined primarily by inflammation and/or demyelination of some aspect of the CNS. MS is partly a diagnosis of exclusion and is partly defined by specific findings, but these may vary. This means that there is no specific finding that determines the diagnosis. The principal finding is MRI evidence of scarring (plaquing) in 2 different areas of the CNS. In about 80% of cases there are CSF findings, primarily oligoclonal protein bands.2 However, the symptom picture can suggest MS without either of these findings. Rather, it is the preponderance of findings, while also ruling out other possible explanations, such as other autoimmune or CNS diseases. Some cases seem to be clearly autoimmune, but there is no general agreement regarding the underlying pathological process that created the MS lesions. The first case I saw, about 40 years ago, was in a woman in her 30s who worked in a viral lab. She explained to me that everyone (5 people) who worked in that lab developed MS, and all of them had died except for her. We treated her as if she had a viral problem, and her MS resolved after about a year.
In 2008, a 51-year-old woman came to see me with a diagnosis of progressive MS. I have treated her regularly ever since then, and her disease has very slowly continued to progress. She was walking when she first came to me. Then she needed a cane, then a walker. She is now in a wheelchair. I guess it is possible that our interventions have slowed the progression of her disease, but there is no way for me to know that. She continues to work with us because we treat her for other things, including some of the sequelae of her MS, and she says this benefits her; however, I consider this case a failure. I can see no effect of our treatment on her MS.
A Cured Case?
In 2014, a 44-year-old woman presented to our office. She had been diagnosed with MS 8 years prior, though she reported having been symptomatic since the age of 15, when she began to suffer from heat intolerance. MRI demonstrated typical MS brain lesions. She said she had always been in pain; migraines began at age 6 and were still occurring. She itched everywhere. She was continually dizzy and her speech would slur when she felt worse. She occasionally suffered from paralysis in her legs, being unable to move them, and occasionally her legs would fail while walking. She reported cognitive disturbance during disease exacerbations. Upon examination, she demonstrated severe nystagmus. Her digestion was quite bad.
We began her treatment with a dietary evaluation (using the Carroll methodology), which demonstrated an egg and gluten intolerance. We gave her an adrenal cortex supplement (300 mg each morning) due to evidence of adrenal fatigue. We recommended 2000 mg/day of fish oil. We gave her a bitter tonic for her stomach and digestion. I gave her a dose of Tuberculinum 200c, after which she reported feeling a lot calmer and less pain. I recommended daily constitutional hydrotherapy, which she planned to do at home, since she lived more than an hour away.
I saw her 1 month later and she reported feeling rather good, better than she could remember. The numbness in her hands was significantly reduced. Her eyes and vision were more stable. She’d had significantly fewer migraines the previous month, and her energy had improved. Her appetite and digestion were much better; she was no longer nauseous. The dizziness had decreased. Her legs had not failed her. I was impressed by her progress.
I heard from her 2 weeks later. This was July, so it had warmed up considerably and the heat bothered her (a common finding with MS). Due to the heat, she had more pain compared to a few weeks earlier. Her eyes and dizziness were not as good.
I saw her 1 month later. She reported no leg cramping since starting with us. She said she could really tell if she cheated on her diet (“I feel like crap when I cheat.”) She’d had a constant headache during the previous week. Her pain was mostly back. I started her on 1 grain of USP thyroid, supplemental iodine, betaine HCl with meals, 500 mg/day of N-acetylcysteine (NAC), and I had her continue the adrenal support. Based on her symptoms, I gave her homeopathic Lachesis, to take as needed.
I saw her 1 month later. She began by telling me that she had run out of adrenal support and that when she did, she lost her mind. If she violated her diet, she would get an instant migraine. But she had been doing much better overall. Her double vision had significantly improved. She said she was much better emotionally and that she’d felt an instantaneous difference with the addition of thyroid support. She still had a lot of pain, and did not sleep well, but she felt better on waking in the morning since adding the thyroid. She reported that the Lachesis had really helped by improving her vision and reducing the pain and tingling. “My anxiety has also reduced,” she said. “I used to take an anti-anxiety medicine 3 times daily. Now I only take it occasionally.” She wanted to quit smoking, and asked if I had anything that could help. I continued her on the same regimen and added a smoking remedy, Caladium 30c, to be taken when craving tobacco, and homeopathic Staphysagria, 1LM at bedtime. Staphysagria is, among other things, a remedy that includes any history of abuse of any kind. Most people have some, and I find it often helps people sleep.
I saw her 2 months later. She complained about the pain: “I’m just in a lot of pain – dull, constant, aching, and sharp, shooting pain. And I’m really fatigued all the time.” She had skipped our last appointment because she had become pregnant. She was also complaining of nausea of pregnancy. She had a bladder infection. A dose of Berberis 30c eased her bladder discomfort, and I gave her Symphoricarpos 30c, to take as needed for the nausea.
I did not see her again until after the baby was born, a number of months later. Her primary complaint then was fatigue. I gave her adrenal support, as before, and renewed her thyroid prescription. She had been following her diet and had been taking some of the medicines I had previously prescribed. Her MS had been rather quiescent.
I saw her a year later. She came in with an MS exacerbation. She had been off her diet, and there was a lot of stress in her family. Her legs were hurting again, and her speech was slurry some of the time. She ached all over. I gave her a dose of homeopathic Phosphorus in the office, based on the totality of the symptom picture, and her pain eased. I gave her a botanical combination for stress, and started her on homeopathic Phosphorus, 1LM, to be taken nightly before bed. A week later she reported a significant reduction in pain, and said the slurring had resolved. She was feeling much better.
I saw her a few months later. She thanked me for curing her MS. I questioned whether she was actually cured. She reported that she hardly ever had any pain or weakness, unless she had a diet error. She had no slurring of speech. She felt strong, and her vision was steady. She still needed the thyroid support. She occasionally took adrenal support. But, overall, she was much better than when she had first come to see me. Instead of getting worse and worse, and being in pain and having her legs fail, she was strong, had no pain, and was getting better and better over time.
I have seen her several times since, and she continues to report improvement overall, and no significant MS symptoms. She is still bothered by the summer heat, but she has had no MS exacerbations within the past 3 years. She said that the key piece for her was learning the relationship between her diet and her illness, and that gave her power and control. She is very grateful.
A Case of Symptom Improvement
In my last article, I reported on a young woman whose MS lesions had substantially reduced since we began treating her. A few months before I saw her, I saw another young woman who was awaiting a diagnosis. She had some symptoms suggestive of MS, and had an MRI, and was awaiting the neurologist’s diagnosis. Her chief complaints were dizziness and anxiety, with a feeling that she could faint. She described her dizziness as if she were watching her life in a movie. This began after the birth of her 4-year-old. Her stomach ached. She had brain fog. The original MRI showed lesions on her brain and brain stem. She said, “When I bend my neck, it sends shocks down my legs. My body can be numb. I have headaches on the right side, behind my right eye. I can wake with the headache, and with nausea. I have sinus problems and have had a few infections. I have horrible menstrual cramping. I have numbness and tingling on the left side of my nose.”
I took her history and examined her. Her stomach was disturbed. Her temperature was low, about 97.0 °F. During the interview, after the exam, I gave her a drainage remedy, one usually used to open a case. It stimulates the emunctories, in general, and focuses on the digestion. She reported that the dizziness left her and she felt calmer; the anxiety was gone. I sent her home with a bitter tonic, an initial set of drainage remedies, and a botanical combination of Melissa officinalis, Avena sativa, Bacopa monnieri, and Centella asiatica, at 75 drops in water 3-4 times daily. I gave her dietary advice based on old Dr Carroll’s method. She was intolerant to egg, gluten, and the combination of fruit and sucrose.
I saw her 1 month later. She had received a preliminary diagnosis of MS with active lesions, and the lesions had increased since the first MRI. A CSF analysis was pending. She liked the Melissa combination. She reported less dizziness and fogginess, and her headache had reduced, but she was still nauseous and anxious. I tried her on a different drainage set, one directed at the CNS. As I gave her the remedies in my office, her dizziness totally abated. I sent her home with that set of remedies, alpha-lipoic acid (500 mg twice daily), NAC (500 mg twice daily), and 2000 mg/day of fish oil.
I saw her 1 month later. She reported feeling much better. The dizziness had diminished, and that “out-of-body” sense was way down. She felt worse when she ran out of the drainage remedies. The headache was much improved. She began taking sertraline for anxiety, though she liked the effect of the Melissa drops and wanted to continue them.
I saw her months later. She reported feeling definitely better – no headache – though she’d had some brief episodes of dizziness and nausea. The anxiety was “way better.” She was awaiting the next MRI. We continued the same regimen, with the addition of Natrum muriaticum, 1LM daily, based on her overall picture.
I did not see her again for 6 months. She reports feeling fine now – only slight dizziness or brain fog occasionally, but, again, “way better.” However, the MRI in November showed enhancing lesions in the brain and brain stem. Her neurologist wants to put her on siponimod, and she has decided to start it. In this case, we have improvement in symptoms but a worsening of lesions on MRI.
Conclusion
My rationale in all of these cases is the same. The purpose of the dietary work is to reduce toxemia, a primary cause of inflammation. The hydrotherapy is to improve blood flow to the digestive system, enhance detoxification, and stimulate the vital force. The bitter tonic or the betaine HCl is to improve digestion, which is to enhance nutrition and reduce the toxemia. The homeopathics are to stimulate individualized healing and the vital force. The drainage remedies are to enhance tissue function and open the emunctories, to reduce toxicity. I used some substances to reduce inflammation in the brain and promote brain repair.
Why does one case have dramatic improvement, another have slow and steady improvement, another have slow and steady worsening, and another have no apparent effect from our interventions? MS is a difficult problem, and each case is different and reacts differently, as each person is different and responds differently. The best I can do is to apply the medicine to the best of my ability, stimulate the Vis Medicatrix, and see what happens. Sometimes a miracle occurs.
Respectfully,
Jared L. Zeff, ND, VNMI, LAc
References:
- National Multiple Sclerosis Society. Types of MS. 2020. Available at: https://www.nationalmssociety.org/What-is-MS/Types-of-MS. Accessed January 24, 2021.
- Deisenhammer F, Zetterberg H, Fitzner B, Zettl UK. The Cerebrospinal Fluid in Multiple Sclerosis. Front Immunol. 2019;10:726.

Jared L. Zeff, ND, VNMI, LAc is a licensed doctor of naturopathic medicine and a licensed acupuncturist. In addition to functioning as Medical Director at the Salmon Creek Naturopathic Clinic in Vancouver, WA, Dr Zeff taught on the faculty at National University of Natural Medicine in Portland, OR, where he was also Dean from 1988 to 1993, and holds a professorship in Naturopathic Medicine. Dr Zeff is a graduate of the University of California, NCNM, and the Emperor’s College of Traditional Oriental Medicine. He, along with Pamela Snider, is the author of the AANP’s Definition of Naturopathic Medicine, and the Therapeutic Order concept.