Deborah Frances, RN, ND
Vis Medicatrix Naturae
A Homeopathic & Herbal Case-Centered Perspective
A 36-year-old white male reported to our clinic with acute cellulitis following a spider bite. The bright-red inflammation that covered much of his left forearm was hot to the touch; however, there were no signs of suppuration and symptoms had come on only a few hours after brushing a spider from his arm. Three doses of Belladonna 200C, 6 hours apart, was all that was needed to clear the symptoms.
Most infected skin wounds involve gram-positive cocci. Staphylococcus aureus is the most common, although other pathogens, including Group A beta-hemolytic Streptococcus (GABHS), have been implicated in infections of the skin. Both S aureus and GABHS can cause cellulitis, abscess, impetigo, bacteremia, and septic shock. Both organisms are showing increasing rates of resistance to antibiotics.
Certain types of GABHS – the same organism implicated in some cases of streptococcal pharyngitis – can result in post-infection complications. Rheumatic fever is now seen in less than 3% of patients following GABHS infection.1 Post-streptococcal acute glomerulonephritis is more common and can occur following Strep pharyngitis or skin infection. The incidence of acute nephritis is higher in children and occurs in 10-15% of patients infected with GABHS.1 Nearly all affected children heal without permanent renal damage, as do most adults.1 Interestingly, antibiotic therapy has little impact on the incidence of nephritis, though it is thought to be responsible for the decline of rheumatic fever.1
In over 25 years of treating streptococcal pharyngitis, impetigo, and skin wounds with homeopathy and herbs, I’ve witnessed only 1 case of post-streptococcal glomerulonephritis. That was an adult male with no prior symptoms of pharyngitis but whose pre-school daughter had been treated for GABHS pharyngitis a few weeks prior. His nephritis resolved quickly with naturopathic therapies. I have not seen a case of rheumatic fever, and I continue to treat GABHS infections with complete confidence using homeopathy and herbs.
The homeopathic remedy Arnica montana is well known among naturopathic doctors for the initial treatment of almost any injury, but this simple remedy also helps prevent infection. By reducing the stagnation of blood and lymph at the site of an injury, Arnica enhances local circulation, thereby increasing transport of immune cells and healing nutrients to the area and preventing toxic waste accumulation. According to Boericke, Arnica can be used for “septic conditions and [is] prophylactic of pus infection.”2
When the wound does become infected, the correct homeopathic remedy combined with appropriate herbs and nutrients speeds rapid resolution. Fortunately, most infected wounds respond well to one of only a few common remedies, making remedy selection easier for the non-homeopath.
Hepar calcarea sulphuricum (Hepar sulph) is the most commonly prescribed remedy for infected wounds in our clinic. Tissues surrounding the wound will be abnormally red and tender to touch, with actual or impending purulent discharge. Boericke recommends Hepar sulph for “abscesses… papules prone to suppurate and acne in youth,” adding that the “tendency to suppuration is most marked.”3 (Figure 2)
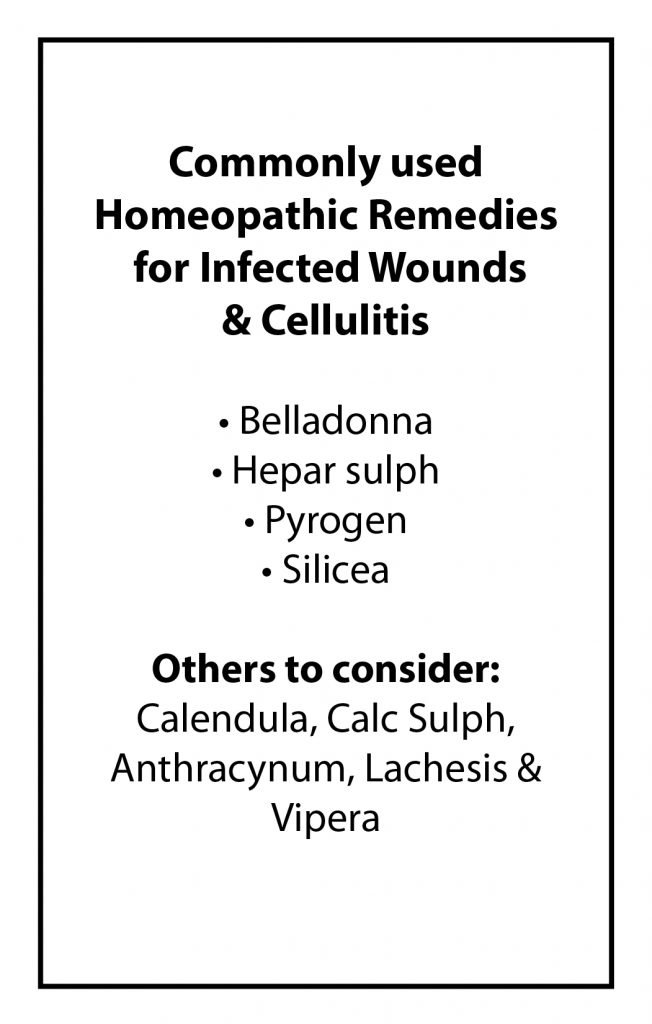
Figure 1. Key Remedies for Infected Wounds
Case Study 1
When a fellow equestrian showed me a jagged laceration incurred a few days earlier while working with rusty barbed wire, the prescription for Hepar sulph seemed clear. A close look at the 3-cm tear on her forearm revealed evidence of a purulent discharge, while adjacent tissues were red, slightly swollen, tender to palpation, and warmer than surrounding skin.
I dispensed a vial of Hepar sulph 200C, with instructions to take it q 4 hours for a couple doses, then q 6 hours as needed. I also recommended regular rinses with Calendula succuss and the application of a drawing poultice of plantain once she got home from her ride. Erythema and tenderness began to subside within 45 min after the first dose of Hepar sulph, and the infection cleared completely with a few more doses.
Calcarea sulphuricum and homeopathic Calendula repertorize strongly for suppurating wounds.4 Calc Sulph is a remedy to consider when purulent discharge has a yellowish color. If onset and progression of symptoms are subacute or chronic, Silicea is the first remedy to consider. It may also be of help when Hepar sulph seems indicated but does nothing.
When infections threaten to become systemic, and symptoms of fever, chills, red streaking, or lymphadenopathy set in, Pyrogen will often cure the case. Clarke says, “Sepsis is the essence of the action of Pyrogen… wherever poisoning by bacterial products is going on, Pyrogen will be likely to do good.” He adds that Pyrogen has been used with good effect for puerperal fever, blood poisoning, diphtheria, and typhoid, and that Pyrogenium is “one of the germinal remedies of the materia medica. When once the idea of its essential action is grasped, an infinity of applications become apparent.”5
I have personally used this remedy with success in more serious cases of urinary cystitis, pelvic inflammatory disease (PID), and dental abscess, as well as infected wounds. The remedy has been useful so often that I think of it now as a polychrest for more serious infections.
Case Study 2
I had occasion to call on Pyrogen myself after an injured cat sank her incisor deep into the tissues of my hand. Cats’ mouths are notorious for being rich reservoirs of pathogenic bacteria; to make matters worse, this was a closed puncture wound. When I arrived at my pharmacy several hours later, my hand was erythematous, hot, swollen, and starting to throb. Fever and shaking chills had set in, and there were already signs of streaking up my arm.
Certain I’d end up in the hospital on IV antibiotics, I tried a dose of Pyrogen 10M. The result was dramatic. The fever, chills, and red streaking disappeared within 10 to 15 min. I continued the remedy at the 10M potency q 4 hr for a few doses, before dropping to q 6 to 8 hr. I also took high doses of Echinacea, vitamins A and C, and zinc in a tablet that included a few other herbs and nutrients in lower doses. Baptisia tinctoria was added to augment the actions of Echinacea, and I took 5 gtt of this tincture 8 times per day. I never needed the antibiotics.
Case Study 3
I had used Pyrogen in several cases when a 59-year-old white male presented to our clinic complaining of a chronic red “rash” on his lower legs. The red discoloration that streaked and peppered his calves and shins was classic for a diagnosis of dermatitis due to poor circulation, but vascular tests performed by his doctors had all come up normal. The patient denied pain or itching, and there was no lymphadenopathy. Both extremities were of a normal temperature to the touch, with strong pedal pulses – 2 findings highly inconsistent with a diagnosis of vascular insufficiency.
I sat back in my chair, as puzzled as any of my allopathic colleagues, and gazed at the eruption with consternation. Something about the dermatitis reminded me of previous cases of acute cellulitis that had responded well to Pyrogen. On a hunch, I prescribed Pyrogen 6C, to be taken QID.
On follow-up 3 wk later, the patient reported significant amelioration of his symptoms. This was validated by PE, which revealed a 40-50% improvement in the dermatitis. The patient continued the remedy for a few more months, increasing to a 12C potency 10 wk into treatment. What was probably a case of chronic cellulitis was completely cleared in 6 to 8 mo and never recurred.
Case Study 4
My cat, Jazz, had a 5-cm laceration on his side some years ago that became grossly infected. My initial prescription of Pyrogen did nothing, and although I quickly moved to the next remedy, the tissues were decomposing rapidly and the wound had enlarged to 7 cm. Purulent exudate discharging from the site was strong-smelling and horribly offensive.
Homeopathic Anthracynum was miraculous. The offensive smell dissipated within 1-2 doses of a 10M potency, given q 4 hr, and the wound quickly began to turn around. Complete resolution took several days, but the infection cleared and the wound did heal.
My cat’s wound brings to mind cases I saw years ago while working as a nurse in hospitals. Patients with disintegrating wounds emanating the same horrible stench of decomposing tissue that the cat’s wound had given off might well have been helped by a few doses of Anthracynum.
Homeopathic Anthracynum is specific for boils, malignant ulcers, abscesses, and wounds with foul malodorous discharges, and is also useful for tissues with blue or black discoloration.6
Case Study 5
Dr Chris Chlebowski of Ashland, OR, reported a case of a 65-year-old woman with acute cellulitis of the lower extremity. Self-prescribed applications of black salve had produced a small ulcer that had become infected. Tissues around the ulcer were hot, swollen, and purple. Discomfort in the leg was ameliorated by elevating the extremity.
Based on the discoloration and Vipera keynote of pain aggravated by allowing the affected limb to hang down,7,8 Dr Chlebowski prescribed Vipera 200C TID. He also packed the ulcer with a silver gel and gave a tincture of Echinacea, 30 gtt q 2 hr. The patient reported significant improvement within 24 hr, and the cellulitis cleared within a few days.
When infection or cellulitis presents with bluish-black or purple discoloration of skin surrounding an infected wound, the homeopathic snake venoms should always be considered. Murphy’s homeopathic repertory lists Lachesis and Vipera under bluish, black, or gangrenous wounds, and Lachesis is included in the rubric for septic wounds.4
Herbal Support
While homeopathy can be miraculous in its ability to stimulate healing, the addition of herbs and nutrients provides an essential foundation of nourishment. Many botanicals provide direct antimicrobial actions, as well as stimulate immune response. (Figure 2)
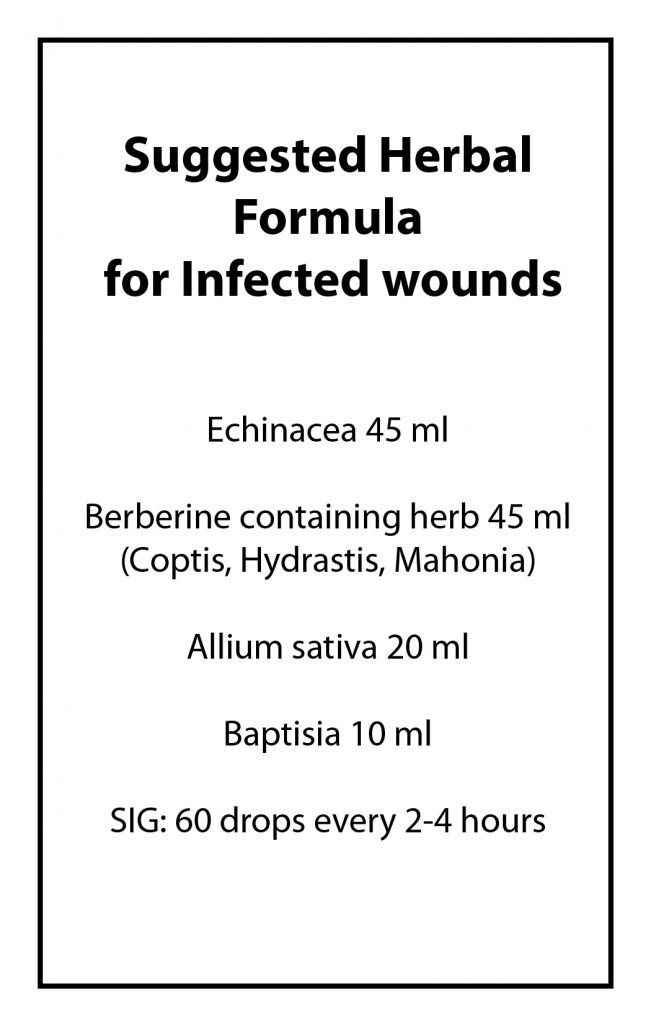
Figure 2. Herbal Formula for Infected Wounds
Traditional use of Echinacea root for sepsis, gangrene, “blood poisoning,” and the bites of venomous snakes and insects9 places this herb high on the list for the botanical treatment of infected wounds. Echinacea can be dosed high and often in acute conditions, without concern for toxicity. Sixty gtt of tincture may be given q 2 hr while awake for the first couple of days, dropping to q 4 hr thereafter unless symptoms call for continued high doses. Echinacea has been highly efficacious in our clinic for the treatment of infected wounds, so I rely on it as my foundational herb in these cases.
Clinical experience has shown that the addition of Baptisia tinctoria enhances the action of Echinacea in these cases. Specific indications for Baptisia include wounds with swollen tissues, dusky inflammation, fetid discharge, and sepsis. Unlike Echinacea, Baptisia is one of our low-dose botanicals and should be dosed judiciously to prevent toxicity: 45 gtt in divided doses over a 24-hr period is a safe maximum dose. Symptoms of overdose include severe vomiting, catharsis, ptyalism, and, eventually, respiratory arrest.9 Low doses of Baptisia may have a mild laxative effect, thereby enhancing elimination of toxins.
Synergy of several antimicrobial alkaloids in berberine-containing plants, such as Hydrastis canadensis and Coptis chinensis, have been shown to be more effective than berberine alone. Efficacy of berberine is also dependent on the multi-drug resistance (MDR) pump inhibition of 5’-methoxyhydnocarpin-D (5’-MHC-D) that is present in these plants, confirming the wisdom of using whole-plant extracts.10-13
Andrographis paniculata has shown significant stimulation of specific and nonspecific immune functions, giving the plant a broad range of activity in treating infection.14 Other herbs, such as Allium sativa and Anemopsis californica, may also be effective against S aureus.15
In those rare instances when naturopathic therapies fail to clear infection, herbal and nutritional therapies should be continued, as studies indicate that the efficacy of antibiotics is enhanced when these therapies are combined.15 In the present era of ever-increasing microbial resistance to pharmaceuticals, naturopathic doctors hold a unique position in their ability to provide safe and effective therapies for the treatment of infection.
References:
- Beers MH, Porter RS, Jones TV, eds. The Merck Manual of Diagnosis and Therapy, 18th Whitehouse Station, NJ: Merck Research Laboratories; 2008:1442-1448.
- Boericke W. Materia Medica with Repertory. 9th Santa Fe, NM: Boericke and Tafel, Inc; 1927:61.
- Boericke W. Materia Medica with Repertory. 9th Santa Fe, NM: Boereike and Tafel, Inc; 1927:261-263.
- Murphy R. Homeopathic Clinical Repertory. 3rd Blacksburg, VA: Lotus Health Institute; 2005:494-497.
- Clarke JH. A Dictionary of Practical Materia Medica, Vol. III. New Delhi, India: Jain Publishers; 2005:931-937.
- Clarke JH. A Dictionary of Practical Materia Medica, Vol I. New Delhi, India: Jain Publishers; 2005:118-119.
- Clarke JH. A Dictionary of Practical Materia Medica, Vol III. New Delhi, India: Jain Publishers; 2005:1553-1556.
- Boericke W. Materia Medica with Repertory. 9th Santa Fe, NM: Boericke and Tafel, Inc; 1927:543.
- Felter H. The Eclectic Materia Medica, Pharmacology, and Therapeutics. Sandy, OR: Eclectic Medical Publications; 1985(Reprint):347.
- Stermitz FR, Lorenz P, Tawara JN, et al. Synergy in a medicinal plant: antimicrobial action of berberine potentiated by 5’-methoxyhydnocarpin, a multidrug pump inhibitor. Proc Natl Acad Sci U S A. 2000;97(4):1433-1437.
- Sternitz FR, Tawara-Matsuda J, Lorenz P, et al. 5’-Methoxyhydnocarpin-D and pheophorbide A: Berberis species components that potentiate berberine growth inhibition of resistant Staphylococcus aureus. J Nat Prod. 2000;63(8):1146-1149.
- Lewis K. In search of natural substrates and inhibitors of MDR pumps. J Mol Microbiol Biotechnol. 2001;3(2):247-254.
- Ball AR, Casadei G, Samosom S, et al. Conjugating berberine to a multidrug efflux pump inhibitor creates an effectual antimicrobial. ACS Chem Biol. 2006;1(9):594-600.
- Sodhi V. Ayurvedic Herbs: The Comprehensive Resource for Ayurvedic Healing Solutions. Lithia Springs, GA: New Leaf Distributing Co Inc; 2014:25-39.
- Snowden R, Harrington H, Morrill K, et al. A comparison of the anti-Staphylococcus aureus activity of extracts from commonly used medicinal plants. J Altern Complement Med. 2014;20(5):375-382.
Image Copyright: <a href=’https://www.123rf.com/profile_13smile’>13smile / 123RF Stock Photo</a>
 Deborah Frances, RN, ND, practiced homeopathy and nutrition as a nurse before graduating from NCNM (now NUNM) in 1993. She practiced in rural OR for several years before returning to Portland to teach at NCNM. Dr Frances has been a popular lecturer at conferences across the country and has taught as adjunct faculty at both NCNM and Bastyr. She has also taught classes on herbal medicine, acute prescribing for NDs, dream work, and shamanic healing. She is strongly influenced by the traditional teachings of her Lakota ancestry. Dr Frances is the author of Practical Wisdom in Natural Healing, available at: drdeborahfrances.wordpress.com. She is currently on sabbatical while resurrecting out of Lyme disease.
Deborah Frances, RN, ND, practiced homeopathy and nutrition as a nurse before graduating from NCNM (now NUNM) in 1993. She practiced in rural OR for several years before returning to Portland to teach at NCNM. Dr Frances has been a popular lecturer at conferences across the country and has taught as adjunct faculty at both NCNM and Bastyr. She has also taught classes on herbal medicine, acute prescribing for NDs, dream work, and shamanic healing. She is strongly influenced by the traditional teachings of her Lakota ancestry. Dr Frances is the author of Practical Wisdom in Natural Healing, available at: drdeborahfrances.wordpress.com. She is currently on sabbatical while resurrecting out of Lyme disease.

