Tolle Causam
Chris D. Meletis, ND
According to the World Health Organization (WHO)’s International Committee for Monitoring Assisted Reproductive Technology, infertility is a reproductive system disease characterized by failure to achieve clinical pregnancy after 1 year or more of regular sexual intercourse without using contraception. In 8% of couples who are unable to conceive, male infertility is the primary cause.1 In 35% of infertility cases, the problem can be traced back to both the male and female or to unknown causes.1 Reduced semen concentration (indicating the number of sperm), decreased semen volume, increased semen viscosity, poor sperm motility (an indication of how well sperm move to fertilize an egg), vitality, and/or abnormal morphology (the shape and appearance of the sperm) are all diagnostic criteria for male infertility, according to the WHO’ Manual for the Examination of Human Semen and Sperm-Cervical Mucus Interaction, 2010 edition.2,3
The cause of male infertility is likely multifactorial, but evidence indicates that exposure to environmental toxins may play an important role in its etiology. Research has established a relationship between sperm abnormalities and exposure to phthalates; chemicals found in plastic food containers; medical equipment like IV tubing; shampoos, deodorants and other personal care products; and many other sources. Wang and colleagues found a correlation between semen phthalate metabolites and decreases in semen volume, motion parameters, curvilinear and straight-line velocity, and an increase in percentage share of abnormal sperm heads and tails.4 In an earlier study, the same researchers observed higher urinary levels of phthalates correlated with declines in sperm levels and total sperm count.5 Higher urinary concentrations of phthalates were also associated with a greater percentage share of abnormal sperm heads.5 Other studies have found a noteworthy positive association between urinary phthalate levels and decreased sperm concentrations.6,7 Phthalates can alter DNA methylation,8 indicating that they have an epigenetic effect that can inflict damage on both current and future generations.
Benzene is another chemical found to play a role in male infertility. Widespread exposure in the United States occurs due to benzene’s presence in cigarette smoke, gasoline fumes, and vehicle emissions. A study of men exposed to benzene at work observed a decline in total sperm count and sperm motility and an increase in abnormal sperm morphology.9 Another study of men occupationally exposed to benzene noted an increased incidence of chromosomally defective sperm.10 De Celis and associates investigated sperm health in workers exposed to ethylbenzene, benzene, toluene, and xylene.11 Compared to men who were not exposed to these chemicals, men who interacted with these toxins at work had alterations in sperm viscosity, liquefaction capacity (the amount of time required for sperm to liquify after ejaculation), sperm count, sperm motility, and the proportion of sperm with normal morphology.11 Some of these abnormalities corresponded to the number of years the men were exposed to the chemicals.
In this article I will present the case of an infertile man who was exposed to environmental pollutants. This case study will demonstrate how a proprietary fertility formula for men, containing 27 nutrients, was able to overcome obstacles to conceiving in a patient who refused to alter his lifestyle to minimize toxin exposure. As clinicians, it illustrates the need to modify our treatments to accommodate the level of compliance among our patients.
Case Study
Personal History & Concerns at Presentation
A 33-year-old male house-builder presented to my practice on June 6, 2017. He worked hard performing physical labor 5 to 6 days per week. He and his wife had a 4-year-old child and wanted to conceive another. He was unwavering in his consumption of the standard American diet and consumed 1 to 2 alcoholic beverages per night. He enjoyed fishing from a nearby river and eating his fresh catches. He was 40 pounds overweight.
He and his wife of 8 years arrived in my office after 2 years of unsuccessfully trying to conceive a second child. A series of previous tests performed by a local fertility specialist had revealed that the cause of the couple’s inability to conceive was male factor infertility. His wife was willing to implement alternative approaches to conception, although he was reluctant to do so. He was not interested in changing his western diet, which may have been exposing him to toxins linked to infertility and was likely contributing to his overweight, which in itself is a risk factor for reduced fertility.12 He was too tired to do additional exercise or pursue fitness. I educated him and his wife about toxins that can act as hormone disruptors that may affect male and female fertility.
Diagnostic Assessment
The evidence in the medical literature pointing toward a correlation between environmental toxins and infertility provided a sound rationale for ordering an organic acids profile, as well as an environmental pollutant panel that measures metabolites of several common environmental toxins. The patient’s pollutant panel results (Figure 1) showed high levels of benzoate (>12.85; reference range [RR]: <7.00) – an indicator of high toluene exposure. The marker tt-muconic acid was also elevated (0.45; RR: <0.17), indicating a high benzene exposure.
Figure 1. Environmental Pollutants Profile
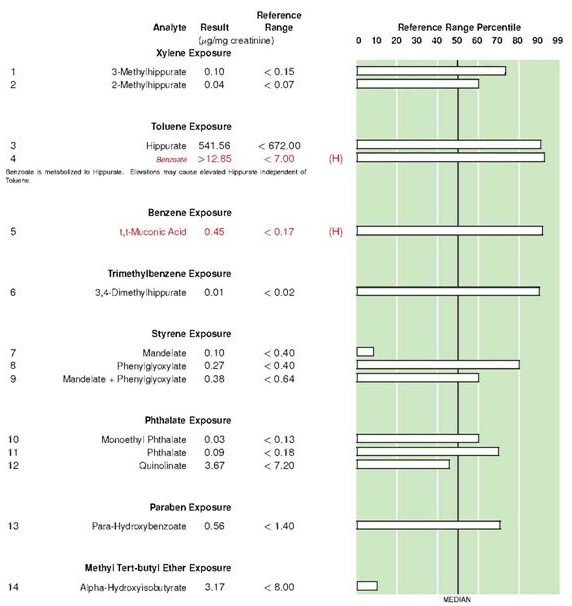
(Lab report courtesy of US BioTek)
A sperm analysis was also undertaken. Sperm concentration was 9 million/mL (lower reference limit: 15 million/mL). Sperm motility was 42% (lower reference limit: 32%). Morphology was 5% (lower reference limit: > 4%). And semen volume was 2 mL (lower reference limit: > 1.5 mL).
From 1999 to 2010 the WHO progressively reduced the lower reference limit for these parameters.13 This means that “normal” levels of sperm health indicators were previously much different than today. For example, the lower reference limit for sperm motility was previously 50%. Measurements higher than the lower reference limit do not ensure fertilization or a successful pregnancy; rather, higher measurements increase the likelihood.
I also ordered a lipid panel, which revealed high total cholesterol, a high concentration of low-density lipoprotein (LDL), a low concentration of high-density lipoprotein (HDL), high triglycerides, and an elevated liver enzyme (ALT: 52; RR: 9-46). The elevated lipid levels were consistent with the findings of a study that observed infertile men having a higher risk of cardiometabolic disease.14 His testosterone levels were within range (639 ng/dL; RR: 250-1100).
Therapeutic Intervention
As noted earlier, the patient refused to alter his diet or implement an aerobic exercise routine. He was also unwilling to begin a detoxification program in order to improve phase 1 and 2 liver detoxification. In phase 1 detoxification, enzymes in the liver catalyze the oxidation, reduction, and hydrolysis of toxins.15 In phase 2, toxins are conjugated and ultimately excreted from the body (Figure 2).15
Figure 2. Hepatic Detoxification
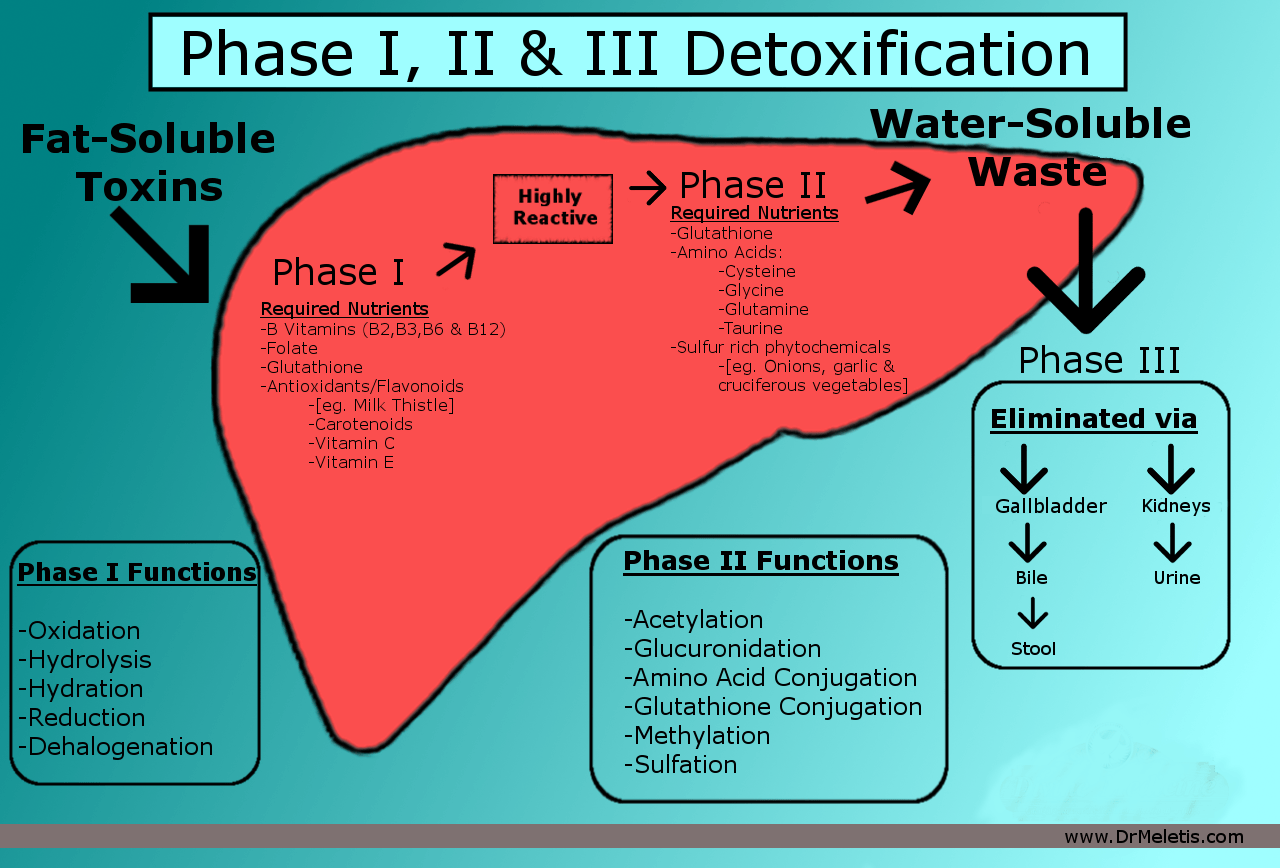
Due to his refusal to undertake a detoxification program, I had to modify my usual protocol to meet the patient on his own terms. With some negotiation and nudging by his wife, he was willing to do 2 things. First, as a simple way support detoxification, he agreed to improve his bowel movement regularity. He began supplementation with magnesium citrate to increase his bowel movements from once every 2-3 days to 2 times per day. The goal was to simply lessen reabsorption of toxins via phase 3 detoxification from the gastrointestinal tract by increasing regularity. I still hold out that he will one day pursue a thorough detoxification protocol.
Second, he was willing to take a supplement formulated for male infertility. This product includes 27 ingredients studied for their beneficial effects on sperm count, concentration, motility, morphology, and DNA integrity by protecting sperm from the damaging effects of oxidative stress. These ingredients include beta-carotene, vitamin C, bioavailable folate, natural vitamin E, zinc, selenium, L-carnitine, grape seed extract, coenzyme Q10 (CoQ10), lycopene, and N-acetylcysteine, to provide broad-spectrum antioxidant support. Zinc is included to improve sperm motility and reduce sperm DNA fragmentation.16 Selenium and vitamin E also improve sperm motility in addition to morphology.17 Supplementation of these nutrients to infertile men has resulted in an increased rate of spontaneous pregnancy.17 L-carnitine improves sperm motility and elevates sperm count.18 According to a systematic review of the medical literature, L-carnitine improves sperm quality and increases spontaneous pregnancy rates in couples affected by a low sperm count.19 Arginine is included in the formula because it elevates levels of nitric oxide, which is needed for sperm quality and erectile function. Arginine has been shown to improve sperm motility in men with infertility.20 Many of the ingredients in the formula have been found to have synergistic effects.
In one study, CoQ10 together with vitamins C and E led to significantly improved sperm counts and motility among 169 infertile men.21 CoQ10 supplementation combined with the vitamins was associated with a 28.4% conception rate.21 Gual-Frau and colleagues studied 20 infertile males with grade I varicocele (a common cause of low sperm count and sperm quality) who supplemented with L-carnitine, vitamin C, CoQ10, vitamin E, vitamin B9, vitamin B12, zinc, and selenium daily for 3 months.22 Supplementation was associated with a 22.1% decline in sperm DNA fragmentation and a rise in total numbers of sperm cells. Mora-Esteves and Shin found that supplementation of antioxidants by men with infertility who were undergoing assisted reproduction led to a 4.85-fold increase in live-birth rate.23
It is relevant to this case study that some of these nutrients are also required to support phase 1 of the liver’s detoxification pathways. B vitamins, folic acid, and vitamins E and C are all required for optimal detoxification by the liver.
Results of Treatment
Six months after the initiation of the male fertility supplement, the patient’s semen parameters were significantly improved (Table 1). Sperm concentration increased from 9 million/mL before supplementation to 58 million/mL after supplementation. Sperm motility increased from 42% to 68% after supplementation. Sperm morphology improved from 5% to 10%. Semen volume increased from 2 mL to 3.4 mL. Nine months after the patient started the supplement, his wife became pregnant.
Table 1. Semen Analysis Results Before & After Supplementation
| Before | After | |
| Sperm concentration | 9 million/mL | 58 million/mL |
| Sperm motility | 42% | 68% |
| Sperm morphology | 5% | 10% |
| Semen volume | 2 mL | 3.4 mL |
Discussion
Infertility is a widespread problem among modern couples. There is increasing evidence that toxins are involved in both male and female infertility, as well as adverse health outcomes in newborns and children exposed to chemicals in utero. The surge in autism and other childhood maladies, including cancer, is widely attributed to toxin exposure in the womb and postnatally. These chemicals not only impair fertility; they also induce epigenetic changes that can impact many generations.
Antioxidants are known to protect against oxidative stress, which is induced by environmental toxins. For example, phthalates were shown in mice to cause liver and kidney damage by means of oxidative stress, and the antioxidant vitamin E protected against this damage.24 In a rodent study, the antioxidants vitamin E and vitamin C reduced oxidative stress and improved spermatogenesis, which had been impaired by phthalate administration.25 And in mice exposed to phthalates, L-carnitine maintained the sperm’s normal morphology and chromatin quality and normalized the sperm count, supporting the idea that nutrient supplementation can protect the sperm from environmental pollutants.26 This may explain, in part, antioxidants’ beneficial effects on sperm health in a world where men are continually exposed to harmful chemicals.
In the case study presented here, a fertility supplement containing antioxidants was associated with successful conception after 9 months of use. This success was achieved despite the fact the patient was unwilling to change his lifestyle in any way. Since he had high levels of metabolites of 2 common environmental pollutants (benzene and toluene), it is possible that the success of the supplementation was due to a protective effect of the nutrients against these environmental toxins. This case study illustrates the beneficial effects of antioxidants in male infertility. Furthermore, it is an example of what clinicians can accomplish when we adapt our protocols to match a patient’s compliance level.
References:
- Centers for Disease Control and Prevention.Infertility FAQs. Last reviewed January 16, 2019. CDC Web site. https://www.cdc.gov/reproductivehealth/infertility/. Accessed September 8, 2019.
- World Health Organization.WHO laboratory manual for the examination and processing of human semen, 5th ed. 2010. WHO Web site. https://apps.who.int/iris/handle/10665/44261. Accessed September 8, 2019.
- Kumar N, Singh AK. Trends of male factor infertility, an important cause of infertility: A review of literature. J Hum Reprod Sci. 2015;8(4):191-196.
- Wang YX, Zeng Q, Sun Y, et al. Semen phthalate metabolites, semen quality parameters and serum reproductive hormones: A cross-sectional study in China. Environ Pollut. 2016;211:173-182.
- Wang YX, Zeng Q, Sun Y, et al. Phthalate exposure in association with serum hormone levels, sperm DNA damage and spermatozoa apoptosis: Across-sectional study in China. Environ Res. 2016;150:557-565.
- Kranvogl R, Knez J, Miuc A, et al. Simultaneousdetermination of phthalates, their metabolites, alkylphenols and bisphenol A using GC-MS in urine of men with fertility problems. Acta Chim Slov. 2014;61(1):110-120.
- Pan Y, Jing J, Yeung LYW, et al. Associationsof urinary 5-methyl-2′-deoxycytidine and 5-hydroxymethyl-2′- deoxycytidine with phthalate exposure and semen quality in 562 Chinese adult men. Environ Int. 2016;94:583-590.
- Moody L, Kougias D, Jung PM, et al. Perinatal phthalate and high-fat diet exposure induce sex-specific changes in adipocyte size and DNA methylation. J Nutr Biochem. 2019;65:15-25.
- Katukam V, Kulakarni M, Syed R, et al. Effect ofbenzene exposure on fertility of male workers employed in bulk drug industries. Genet Test Mol Biomarkers. 2012;16(6):592-597.
- Marchetti F, Eskenazi B, Weldon RH, et al. Occupational exposure tobenzene and chromosomal structural aberrations in the sperm of Chinese men. Environ Health Perspect. 2012;120(2):229-234.
- De Celis R, Feria-Velasco A, González-Unzaga M, et al. Semen quality of workers occupationally exposed to hydrocarbons. Fertil Steril. 2000;73(2):221-228.
- Škurla M, Rybář R. Obesity and reduced fertility of men. Ceska Gynekol. Winter 2018;83(3):212-217.
- Cooper TG, Noonan E, von Eckardstein S, et al. World Health Organization reference values for human semen characteristics. Hum Reprod Update. 2010;16(3):231-245.
- Kasman AM, Li S, Luke B, et al. Male infertility and future cardiometabolic health: Does the association vary by sociodemographic factors? Urology. 2019 Aug 1. pii: S0090-4295(19)30697-1. doi: 10.1016/j.urology.2019.06.041. [Epub ahead of print]
- Grant DM. Detoxification pathways in the liver. J Inherit Metab Dis. 1991;14(4):421-430.
- Omu AE, Al-Azemi MK, Kehinde EO, et al. Indications of the mechanisms involved in improved sperm parameters by zinc therapy. Med Princ Pract. 2008;17(2):108-116.
- Moslemi MK, Tavanbakhsh S. Selenium-vitamin E supplementation in infertile men: effects on semen parameters and pregnancy rate. Int J Gen Med. 2011;4:99-104.
- Moradi M, Moradi A, Alemi M, et al. Safety and efficacy of clomiphene citrate and L-carnitine in idiopathic male infertility: a comparative study. Urol J. 2010;7(3):188-193.
- Shang XJ, Wang LL, Mo DS, et al. Effect and safety of L-carnitine in the treatment of idiopathic oligoasthenozoospermia: a systemic review. Zhonghua Nan Ke Xue. 2015;21(1):65-73. [Article in Chinese]
- Scibona M, Meschini P, Capparelli S, et al. L-arginine and male infertility. Minerva Urol Nefrol. 1994;46(4):251-253. [Article in Italian]
- Kobori Y, Ota S, Sato R, et al. Antioxidant cosupplementation therapy with vitamin C, vitamin E, and coenzyme Q10 in patients with oligoasthenozoospermia. Arch Ital Urol Androl. 2014;86(1):1-4.
- Gual-Frau J, Abad C, Amengual MJ, et al. Oral antioxidant treatment partly improves integrity of human sperm DNA in infertile grade I varicocele patients. Hum Fertil (Camb). 2015;18(3):225-229.
- Mora-Esteves C, Shin D. Nutrient supplementation: improving male fertility fourfold. Semin Reprod Med. 2013;31(4):293-300.
- Chen Y, Li C, Song P, et al. Hepatic and renal tissue damage in Balb/c mice exposed to diisodecylphthalate: The role of oxidative stress pathways. Food Chem Toxicol. 2019;132:110600.
- Shen L, Tang X, Wei Y, et al. Vitamin E andvitamin C attenuate Di-(2-ethylhexyl) phthalate-induced blood-testis barrier disruption by p38 MAPK in immature SD rats. Reprod Toxicol. 2018;81:17-27.
- Zare Z, Mohammadi M, Eimani H, Shafaroudi MM. Prevention of di (2-ethylhexyl) Phthalate-induced Testicular Disturbance in Mice by Co-administration of L-carnitine. Int J Fertil Steril. 2011;5(3):186-192.
 Chris D. Meletis, ND, is an educator, international author, and lecturer. He has authored over a dozen books and more than 200 national scientific articles in prominent journals and magazines. Dr Meletis served as Dean of Naturopathic Medicine and CMO for 7 years at National University of Natural Medicine (NUNM). He was recently awarded the NUNM Hall of Fame award by OANP, as well as the 2003 Physician of the Year by the AANP. Dr Meletis spearheaded the creation of 16 free natural medicine healthcare clinics in Portland OR. Dr Meletis serves as an educational consultant for Fairhaven Health. His personal mission is “Changing World’s Health One Person at a Time.”
Chris D. Meletis, ND, is an educator, international author, and lecturer. He has authored over a dozen books and more than 200 national scientific articles in prominent journals and magazines. Dr Meletis served as Dean of Naturopathic Medicine and CMO for 7 years at National University of Natural Medicine (NUNM). He was recently awarded the NUNM Hall of Fame award by OANP, as well as the 2003 Physician of the Year by the AANP. Dr Meletis spearheaded the creation of 16 free natural medicine healthcare clinics in Portland OR. Dr Meletis serves as an educational consultant for Fairhaven Health. His personal mission is “Changing World’s Health One Person at a Time.”


