Endogenous and Exogenous
Ronald Steriti, ND, PhD
Testosterone is the major androgen in the body and is the principal male sex hormone. Testosterone is secreted by the testes in males and by the ovaries in females. Small amounts are also secreted by the adrenal glands. In men, testosterone plays a key role in the development of male reproductive tissues such as the testes and prostate, as well as promoting secondary sexual characteristics such as increased muscle, bone mass, and hair growth.1
Testosterone Deficiency
Testosterone is important for a wide number of systems, which can thus be affected by its deficiency. The most common symptoms are sexual dysfunction (low libido or erectile dysfunction) and chronic fatigue.2-5
Age-Related Decline
Serum testosterone levels peak in early adulthood in men, with levels progressively falling with age.6 One study of healthy men (n=1623)7 found a progressive reduction in serum total testosterone levels across age groups, with the mean testosterone value observed for younger men (821.1 ng/ dL; age group ≤ 40 years) being almost twice as high as the levels found for individuals belonging to the older age group (436.6 ng/dL; age group > 70 years).
While gross hypogonadism is uncommon, mild androgen insufficiency may be much more frequent, especially in older men and in those receiving treatment for chronic medical conditions.1 Late-onset male hypogonadism is frequently observed in primary care, with an increasing prevalence in older men. The diagnosis is based on a combination of mostly non-specific signs and symptoms and measurement of testosterone and other hormones.8
Metabolic Syndrome and Type 2 Diabetes
Testosterone appears to have a protective effect on pancreatic beta cells.9 Thus, in men, testosterone deficiency can start a vicious cycle that worsens metabolic syndrome and increase the risk of type 2 diabetes (Figure 1).
In a population-based study of non-diabetic men (n=1896),10 men with free testosterone levels in the lowest tertile had a 3.5-fold increased risk of metabolic syndrome, compared to men with free testosterone levels in the highest tertile; this association was found to be independent of body mass index. Low concentrations of testosterone were also associated with measures of inflammation.
Hyperinsulinemia, insulin resistance, and obesity have also been shown to contribute to declines in testosterone in men.11,12
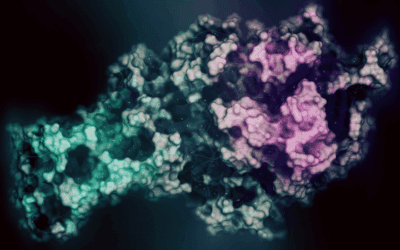
Aromatase
Aromatase is an enzyme that converts testosterone into estradiol (and androstenedione into estrone). The enzyme is highly concentrated in adipose tissue. In men, increased aromatase activity results in reduced testosterone and increased estradiol concentrations, ultimately resulting in a decrease in muscle mass and an increase in total fat mass. Increased fat mass contributes to oxidative stress, inflammation, and a further increase in aromatase activity (Figure 2).13-16
The overall pattern associated with metabolic syndrome, insulin resistance and/or type 2 diabetes and obesity in men can include low testosterone and sex hormone-binding globulin (SHBG) levels, along with high estradiol.17-21 Excessive aromatase activity (hyper-aromatization) can thus be particularly difficult for men because it creates another vicious cycle.
Immune Activation
Studies have suggested an intimate interaction between the immune system and testosterone in males. Animal models have shown testosterone to suppresses the immune system by stimulating the production of interleukin-10, an anti-inflammatory cytokine.22 An “immunocompetence handicap hypothesis” proposes the existence of a trade-off in men between testosterone and immune function. It is thought that the high levels of testosterone required for the full expression of sexual signals may unfortunately also increase the risk of mortality due to their immunosuppressive action. The high cost of these signals has been hypothesized to prevent cheating.23,24
In contrast, a meta-analysis that included various study types found no convincing evidence of a suppressive effect of testosterone on immunity.23 Instead, immune activation was found to have a suppressive effect on plasma testosterone level.
Drug-Induced Testosterone Deficiency
Several agents have been shown to decrease testosterone levels…
Spironolactone
Spironolactone is an aldosterone antagonist and potassium-sparing diuretic. Spironolactone inhibits androgen production and is a potent antagonist of the androgen receptor. Spironolactone significantly decreases plasma testosterone levels and increases the rate of peripheral conversion of testosterone into estradiol, which may cause gynecomastia, among other possible symptoms of excess estrogen.25,26 However, it has been suggested that human data is insufficient at this point to draw definitive conclusions.27
Ketoconazole
Ketoconazole is an “azole” antifungal medication that works by inhibiting sterol production in fungal organisms. In humans, ketoconazole has been found to decrease serum testosterone and sperm motility.28 Currently, it is not known to what extent other “azole” antifungals might have similar effects.27
Metformin
Metformin (850 mg BID for 2 weeks) in normal men resulted in a significant reduction in serum total testosterone, free testosterone, and 17-hydroxyprogesterone. There was also a significant increase in serum SHBG and DHEA-sulphate.29,30
Alcohol
Although animal models have shown ethanol to affect testosterone biosynthesis and aromatase activity, it has been unclear to what extent this applies to humans.
Although a small study showed increases in testosterone from alcohol consumption,31 other studies have shown it to depress testosterone levels in men.32,33, 34 Another study found alcoholics to have low-normal testosterone levels, which gradually increased over 3 weeks of abstinence.35
Marijuana
Clinicians at the Tahoma Clinic and Meridian Valley Labs, with experience at recovery centers, state that they have observed an association between chronic marijuana use and decreased testosterone levels in men.
Human trials, however, are inconclusive. One study found no significant correlations between chronic marijuana use and blood levels of testosterone, LH, FSH, prolactin, or cortisol.36 The authors of a recent review37 noted that “all studies that have documented a statistically significant testosterone decrease after cannabis consumption have also found that the measured testosterone levels in these users are still within the normal range, suggesting that this effect is not likely of behavioral significance.” They went on to conclude that “it is clear that cannabinoid-induced inhibition of male sexual behavior is independent of concurrent declines in testosterone levels.”
Zinc Deficiency
In 4 normal young men, dietary zinc restriction for 20 weeks significantly decreased serum testosterone. In this same study, 6 months of zinc supplementation in marginally zinc-deficient normal elderly men resulted in a 2-fold increase in serum testosterone.38
Vitamin D Deficiency
A recent study published in Clinical Endocrinology (Oxford) found that plasma 25(OH)-vitamin D levels were positively associated with total and free testosterone levels.39 There was a linear relationship at lower levels, reaching a plateau at higher levels.
A study of 54 healthy overweight men with low vitamin D and low-normal testosterone levels examined the effects of vitamin D (3332 IU daily) for 1 year.40 Vitamin D significantly increased testosterone levels in the vitamin D group (n=31), but not in the placebo group (n=23).
Licorice
In addition to pseudo-hyperaldosteronism, which causes hypokalemia and hypertension,41 high-dose Glycyrrhiza glabra (licorice) has been shown to decrease serum testosterone and increase 17-hydroxyprogesterone.42 In this study, 7 normal men were given 7 g daily of licorice tablets containing 500 mg of glycyrrhizic acid. This would be equivalent to more than 14 capsules per day.
Increasing Testosterone Naturally
Ashwagandha
A recent study showed that the administration of Withania somnifera (ashwagandha) root powder (5 g/day for 3 months) to 75 infertile men resulted in increased levels of serum testosterone and LH, as well as reduced levels of follicle-stimulating hormone (FSH) and prolactin.43
Bioidentical Testosterone Replacement Therapy
According to The American Society of Andrology,44 “testosterone replacement therapy in aging men is indicated when both clinical symptoms and signs suggestive of androgen deficiency and decreased testosterone levels are present.” They also state that “testosterone replacement may also be warranted in older men with markedly decreased testosterone levels regardless of symptoms, but signs of androgen deficiency should be present. Contraindications to testosterone therapy include a history of prostate cancer, breast cancer, untreated sleep apnea, and untreated and/or severe congestive heart failure.”
In their position statement,44 they make the following recommendations:
Evaluation is recommended at 3 to 6 months after initiation of therapy, and then yearly, based on individual clinical response
A physical examination, including digital rectal examination of the prostate, a prostate-related symptom assessment, prostate-specific antigen (PSA) level, and hematocrit, should be performed at 3, 6, and 12 months, and then annually
Testosterone therapy should be adjusted or stopped if the hematocrit goes over 52%
Testosterone gels and creams are the preferred method for bioidentical testosterone replacement, as they allow for flexibility in dosing.45 A recent study showed that transdermal application to the upper arms/shoulders may offer better bioavailability compared to the abdomen.46
Conclusion
Testosterone levels in men tend to decline with age. Several other factors may contribute to lower levels, including:
Metabolic syndrome, type 2 diabetes, insulin resistance, and obesity
Increased aromatase activity with increased estradiol
Prescription drugs (spironolactone, ketoconazole, and metformin)
Chronic alcohol or marijuana use
Immune activation
Zinc or vitamin D deficiency
High-dose licorice
Increasing testosterone levels naturally can be accomplished with bioidentical testosterone replacement therapy and possibly ashwagandha root powder.
Figure 1
Low testosterone contributes to the development of blood sugar metabolism dysfunction (ie, insulin resistance, metabolic syndrome). Excess insulin and obesity lead to a further reduction in testosterone production.
Figure 2
In men, increased aromatase activity results in reduced testosterone and increased estradiol, in which contributes to a decrease in muscle mass and an increase in total fat mass. Increased fat mass contributes to oxidative stress, inflammation, and increased aromatase activity.
 Ronald Steriti, ND, PhD is a graduate of Southwest College of Naturopathic Medicine, and is the researcher for Dr Jonathan V. Wright of the Tahoma Clinic and Meridian Valley Labs in Tukwila, WA.
Ronald Steriti, ND, PhD is a graduate of Southwest College of Naturopathic Medicine, and is the researcher for Dr Jonathan V. Wright of the Tahoma Clinic and Meridian Valley Labs in Tukwila, WA.
References
Mooradian AD, Morley JE, Korenman SG. Biological actions of androgens. Endocr Rev. 1987;8(1):1-28.
Traish AM, Guay A, Feeley R, Saad F. The dark side of testosterone deficiency: I. Metabolic syndrome and erectile dysfunction. J Androl. 2009;30(1):10-22.
Traish AM, Saad F, Guay A. The dark side of testosterone deficiency: II. Type 2 diabetes and insulin resistance. J Androl. 2009;30(1):23-32.
Traish AM, Saad F, Feeley RJ, Guay A. The dark side of testosterone deficiency: III. Cardiovascular disease. J Androl. 2009;30(5):477-494.
Traish AM, Miner MM, Morgentaler A, Zitzmann M. Testosterone deficiency. Am J Med. 2011;124(7):578-587.
Swerdloff RS, Wang C. Androgens and the ageing male. Best Pract Res Clin Endocrinol Metab. 2004;18(3):349-362.
Nardozza Junior A, Szelbracikowski Sdos S, Nardi AC, Almeida JC. Age-related testosterone decline in a Brazilian cohort of healthy military men. Int Braz J Urol. 2011;37(5):591-597.
Brunton SA, Sadovsky R. Late-onset male hypogonadism and testosterone replacement therapy in primary care. J Fam Pract. 2010;59(7 Suppl):S1-S8.
Zitzmann M. Testosterone deficiency, insulin resistance and the metabolic syndrome. Nat Rev Endocrinol. 2009;5(12):673-681.
Laaksonen DE, Niskanen L, Punnonen K, et al. Sex hormones, inflammation and the metabolic syndrome: a population-based study. Eur J Endocrinol. 2003;149(6):601-608.
Pitteloud N, Hardin M, Dwyer AA, et al. Increasing insulin resistance is associated with a decrease in Leydig cell testosterone secretion in men. J Clin Endocrinol Metab. 2005;90(5):2636-2641.
, Matsumoto AM, Fujimoto WY, Boyko EJ. Association of bioavailable, free, and total testosterone with insulin resistance: influence of sex hormone-binding globulin and body fat. Diabetes Care. 2004;27(4):861-868.
Cohen PG. Aromatase, adiposity, aging and disease. The hypogonadal-metabolic-atherogenic-disease and aging connection. Medical hypotheses. 2001;56(6):702-708.
Cohen PG, Holbrook JM. Other pathways to the manifestations of the metabolic syndrome in males. Obesity research. 2004;12(9):1536.
Cohen PG. The hypogonadal-obesity cycle: role of aromatase in modulating the testosterone-estradiol shunt–a major factor in the genesis of morbid obesity. Med Hypotheses. 1999;52(1):49-51.
Yazici G, Sayin M. Role of aromatase inhibitors in glucose intolerance of obese men. Medical hypotheses. 2008;71(4):612-613.
Vikan T, Schirmer H, Njolstad I, Svartberg J. Low testosterone levels and sex hormone-binding globulin levels and high estradiol levels are independent predictors of type 2 diabetes in men. Eur J Endocrinol. 2010;162(4):747-754.
Muraleedharan V, Jones TH. Testosterone and the metabolic syndrome. Ther Adv Endocrinol Metab. 2010;1(5):207-223.
Oh JY, Barrett-Connor E, Wedick NM, Wingard DL. Endogenous sex hormones and the development of type 2 diabetes in older men and women: the Rancho Bernardo study. Diabetes Care. 2002;25(1):55-60.
Stellato RK, Feldman HA, Hamdy O, et al. Testosterone, sex hormone-binding globulin, and the development of type 2 diabetes in middle-aged men: prospective results from the Massachusetts male aging study. Diabetes Care. 2000;23(4):490-494.
Haffner SM, Shaten J, Stern MP, et al. Low levels of sex hormone-binding globulin and testosterone predict the development of non-insulin-dependent diabetes mellitus in men. MRFIT Research Group. Multiple Risk Factor Intervention Trial. Am J Epidemiol. 1996;143(9):889-897.
Liva SM, Voskuhl RR. Testosterone acts directly on CD4+ T lymphocytes to increase IL-10 production. J Immunol. 2001;167(4):2060-2067.
Boonekamp JJ, Ros AH, Verhulst S. Immune activation suppresses plasma testosterone level: a meta-analysis. Biol Lett. 2008;4(6):741-744.
Alonso-Alvarez C, Perez-Rodriguez L, Garcia JT, Vinuela J. Testosterone-mediated trade-offs in the old age: a new approach to the immunocompetence handicap and carotenoid-based sexual signalling. Proc Biol Sci. 2009;276(1664):2093-2101.
Cuculi F, Suter A, Erne P. Spironolactone-induced gynecomastia. CMAJ. 2007;176(5):620.
Rose LI, Underwood RH, Newmark SR, et al. Pathophysiology of spironolactone-induced gynecomastia. Ann Intern Med. 1977;87(4):398-403.
Millsop JW, Heller MM, Eliason MJ, Murase JE. Dermatological medication effects on male fertility. Dermatol Ther. 2013;26(4):337-346.
Pont A, Williams PL, Azhar S, et al. Ketoconazole blocks testosterone synthesis. Arch Intern Med. 1982;142(12):2137-2140.
Shegem NS, Nasir AM, Jbour AK, et al. Effects of short term metformin administration on androgens in normal men. Saudi Med J. 2002;23(8):934-937.
Shegem NS, Alsheek Nasir AM, Batieha AM, et al. Effects of short term metformin administration on androgens in diabetic men. Saudi Med J. 2004;25(1):75-78.
Sarkola T, Eriksson CJ. Testosterone increases in men after a low dose of alcohol. Alcohol Clin Exp Res. 2003;27(4):682-685.
Ida Y, Tsujimaru S, Nakamaura K, et al. Effects of acute and repeated alcohol ingestion on hypothalamic-pituitary-gonadal and hypothalamic-pituitary-adrenal functioning in normal males. Drug Alcohol Depend. 1992;31(1):57-64.
Gordon GG, Altman K, Southren AL, et al. Effect of alcohol (ethanol) administration on sex-hormone metabolism in normal men. N Engl J Med. 1976;295(15):793-797.
Vatsalya V, Issa JE, Hommer DW, Ramchandani VA. Pharmacodynamic effects of intravenous alcohol on hepatic and gonadal hormones: influence of age and sex. Alcohol Clin Exp Res. 2012;36(2):207-213.
Ruusa J, Bergman B, Sundell ML. Sex hormones during alcohol withdrawal: a longitudinal study of 29 male alcoholics during detoxification. Alcohol Alcohol. 1997;32(5):591-597.
Block RI, Farinpour R, Schlechte JA. Effects of chronic marijuana use on testosterone, luteinizing hormone, follicle stimulating hormone, prolactin and cortisol in men and women. Drug Alcohol Depend. 1991;28(2):121-128.
Gorzalka BB, Hill MN, Chang SC. Male-female differences in the effects of cannabinoids on sexual behavior and gonadal hormone function. Horm Behav. 2009;58(1):91-99.
Prasad AS, Mantzoros CS, Beck FW, et al. Zinc status and serum testosterone levels of healthy adults. Nutrition. 1996;12(5):344-348.
Nimptsch K, Platz EA, Willett WC, Giovannucci E. Association between plasma 25-OH vitamin D and testosterone levels in men. Clin Endocrinol (Oxf). 2012;77(1):106-112.
Pilz S, Frisch S, Koertke H, et al. Effect of vitamin D supplementation on testosterone levels in men. Horm Metab Res. 2011;43(3):223-225..
Armanini D, Lewicka S, Pratesi C, et al. Further studies on the mechanism of the mineralocorticoid action of licorice in humans. J Endocrinol Invest. 1996;19(9):624-629.
Armanini D, Bonanni G, Palermo M. Reduction of serum testosterone in men by licorice. N Engl J Med. 1999;341(15):1158.
Ahmad MK, Mahdi AA, Shukla KK, et al. Withania somnifera improves semen quality by regulating reproductive hormone levels and oxidative stress in seminal plasma of infertile males. Fertil Steril. 2010;94(3):989-996.
Testosterone replacement therapy for male aging: ASA position statement. J Androl. 2006;27(2):133-134.
Gooren LJ. Advances in testosterone replacement therapy. Front Horm Res. 2009;37:32-51.
Miller J, Britto M, Fitzpatrick S, et al. Pharmacokinetics and relative bioavailability of absorbed testosterone after administration of a 1.62% testosterone gel to different application sites in men with hypogonadism. Endocr Pract. 2011;17(4):574-583.