Deborah Ardolf, ND
Infertility patients usually present to us in a very desperate and near-hopeless position. According to the Centers for Disease Control & Prevention (CDC) 2015 statistics, 7.4 million women have sought out help from various infertility services.
Case Study
My 37-year-old female patient was no different. She and her husband had been trying for 5 years to conceive and maintain a pregnancy. Despite consulting several fertility specialists, an endocrinologist, a primary care physician with a certificate in functional medicine, and conducting her own online “research,” she was beginning to wonder if it would ever happen. She had become pregnant twice within the past year, only to spontaneously abort in as little as 4 weeks.
During this time, she “improved” her diet, set up a simple exercise routine, and initiated a few cleansing protocols. According to the primary care doctor’s recommendations, she underwent imaging and frequent lab work-ups. Structurally, everything was in working order. Her labs revealed low progesterone on multiple blood draws, taken on Days 2 and 21 of her cycle. Estrogen levels were relatively high in comparison. She was advised to avoid the use of plastics for cooking and food and drink storage. She was prescribed leuprolide (which she never took), clomiphene, and a prescription for progesterone, which she followed as prescribed, only to begin experiencing breakthrough bleeding.
In late April 2015, she requested an appointment for a naturopathic medical consultation, based on the recommendation from her friend who was also receiving treatment for infertility through this office. The many beauties of natural medicine include taking into consideration the whole person. We have learned through our experiences and training the importance of mental health. We understand how a person’s life experiences to-date can potentially obstruct the healing process and, therefore, the patient’s overall well-being. Our patients have the opportunity to experience the plethora of natural treatment options at our disposal, to share with our patients in need. Once they begin to partake, they begin to experience the gentle powerful effectiveness of what we prescribe to them. It all starts with taking the case.
Patient History
Of significance, her cycles were brief with scant flow, lasting only 4 days, but regular and accompanied by only mild discomfort. Her PMS, however, was riddled with anxiety, hypersensitivity to loved ones’ impressions, a tendency to tears, and was followed by severe episodic depression. She admitted to hysterical outbreaks during and after experiencing intercourse with her husband. She does not recall any sexual violations, but does recall her father’s desire to sleep together. She had experienced vivid sexual dreams, which would wake her in a fit of panic. She had tremendous fear of never being able to have a child of her own. In her mind, this was all her fault, as her husband had a child from a previous relationship. On the positive side, she reported experiencing ample energy, appetite, digestion, and no insomnia, other than the occasional disruptive nightmare. Past medical history was significant for alcohol and drug abuse 10 years prior, and frequent upper respiratory and urinary tract infections.
Visually, her face, neck, and throat were of a ruddy complexion. She gave the impression of being uncomfortable in her own skin and in the presence of others. Her speech was hesitant and somewhat calculated. It was rare to see a smile, and I never saw a robust laugh.
Goals of Treatment
Our goals included immune and mental health support, and hormone balancing. Due to the urgency of the matter, we utilized a wide variety of modalities. We explained to our patient the importance of not only delivering a baby, but having as a goal a healthy baby and mom. We requested 3 months of treatment time to meet our goals. She was in agreement, already feeling a mild sense of relief, but also some skepticism around this refreshing, inexpensive, nurturing, albeit a bit unusual approach. But first, she opted to follow through on her last infertility appointment before committing to inpatient naturopathic care. At this appointment, in-vitro fertilization (IVF) was highly recommended. She was temporarily enticed.
Treatment
Food as Medicine
Treatment commenced on July 2, 2015. The patient was asked to focus on the consumption of hormone-free foods, cruciferous vegetables to help clear excess estrogens and toxins from her body, foods for healthy blood, and immune-building foods.
Homeopathy
Her mental health was of great concern, and a huge obstacle for us to overcome. Homeopathy seemed like a wise choice to address the totality of her case. Sepia seemed to fit her case quite well. Sepia is known as a premier remedy for sexual or menstrual issues, and pregnancy disorders, including the tendency to spontaneous abort. Sepia also covered her mental health issues; her tendencies to tears or anxiety after intercourse, and her great irritability with the slightest cause, are just a few of the similars. She was prescribed Sepia 30C, 3 pellets QD.
Upon follow-up 1 month later, she appeared healthier; the blotchy red hue was gone from her skin. She appeared calmer, readily smiled, and was clearly much more at ease, with the ability to converse freely. She also noticed improvements at home. She was less sensitive, less likely to become emotional, and instead could hold a discussion regarding whatever was troubling her. Her periods, though, were still scant, slightly improved but still only 3 days in length. Sepia 200C was prescribed.
Acupuncture
She had already been receiving acupuncture, but requested receiving the treatment in our office. Her tongue was scalloped, pale in color, with a purple-hued undercarriage. Pulses were thready, and kidney pulses were weak. A protocol was developed and administered once a week. Tongue and wrist pulses improved after 4 treatments. Twice she called in and requested an appointment when an emotional outburst occurred at home. She felt calmer and back in control by the time she left the office.
Labs
Although a spot hormone blood test showed evidence of a hormone imbalance as a possible obstacle to cure, I was curious to know what her estrogen and progesterone levels were throughout her cycle. After she had received the above treatments, I recommended a salivary hormone profile, with specimens collected at specific times during her cycle; measurements included estradiol, progesterone, testosterone, and DHEA. As Figure 1 illustrates, her luteal phase revealed a sluggish spike in progesterone levels, with no secondary rise in estrogen. DHEA was low-normal, and testosterone was normal. A discussion was held regarding the need to increase her luteal-phase hormones and the treatment options available to her. Because she was leaving Hawaii to visit her family on the mainland, she opted to not change her treatment protocol at this time.
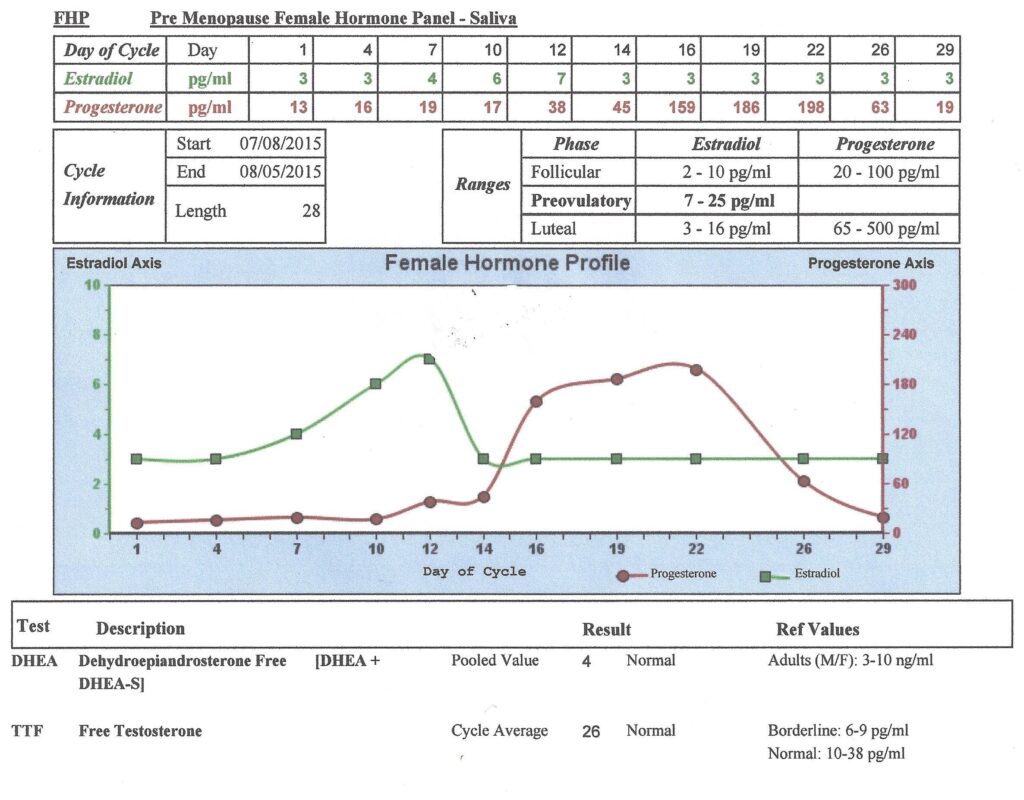
Figure 1. Salivary Female Hormone Profile
Follow-ups
Upon her return to Hawaii on September 7, 2015, she called with an announcement of a positive pregnancy test; however, just like the 2 previous pregnancies, she was already experiencing spotting and cramping. I encouraged her to re-dose Sepia 200C and to continue dosing daily. She was also prescribed an herbal tincture that targeted the luteal phase, which included anti-spasmodics such as Dioscorea, Smilax, Cimicifuga, Angelica sinensis, and Foeniculum vulgare.
Her bleeding and cramping stopped within 48 hours. Follow-up blood work revealed a doubling of human chorionic gonadotropin (hCG). Ultrasound detected a healthy heartbeat. Her second ultrasound, completed in the first week of November, at 14 weeks gestation, helped her to visualize the formation of fingers and toes.
Mom and baby appear healthy and happy while continuing only the homeopathic and herbal medicine, which was reformulated as she began her second trimester. Her second tincture focused more on nourishing herbs while continuing to gently balance her hormones. Our goal is to change the tincture one more time at the beginning of her third trimester. Ahh… the power of natural medicine!
 Deborah Ardolf, ND, is a uniquely trained naturopathic physician. Besides her doctorate degree (SCNM, 2009), she holds a master’s degree in speech pathology. Through this degree, Dr Ardolf obtained medical experience in trauma, neurology, substance abuse, infectious disease, autoimmunity, and oncology at the VA and The Queens Medical Center. While pursuing her naturopathic degree, she studied with a researcher whose natural, self-treating approach focused on immunology; many of his techniques were buried deep in the literature. Dr Ardolf is now practicing in Hawaii. Her emphasis continues to be in immunology, as this is where she can make the greatest impact on the health of mankind.
Deborah Ardolf, ND, is a uniquely trained naturopathic physician. Besides her doctorate degree (SCNM, 2009), she holds a master’s degree in speech pathology. Through this degree, Dr Ardolf obtained medical experience in trauma, neurology, substance abuse, infectious disease, autoimmunity, and oncology at the VA and The Queens Medical Center. While pursuing her naturopathic degree, she studied with a researcher whose natural, self-treating approach focused on immunology; many of his techniques were buried deep in the literature. Dr Ardolf is now practicing in Hawaii. Her emphasis continues to be in immunology, as this is where she can make the greatest impact on the health of mankind.



















