Shaida Sina, ND
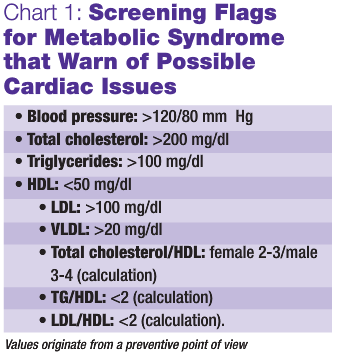 Cardiovascular risk is a real issue for patients with metabolic syndrome. Chart 1 shows screening flags for metabolic syndrome that should draw your attention to possible future cardiac issues.
Cardiovascular risk is a real issue for patients with metabolic syndrome. Chart 1 shows screening flags for metabolic syndrome that should draw your attention to possible future cardiac issues.
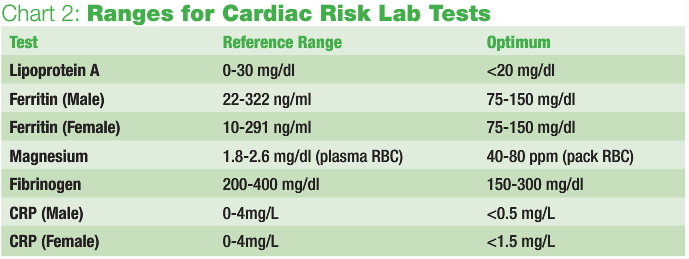
Metabolic syndrome’s pathology begins with inflammation; therefore, some inflammatory marker should be assessed. When evaluating for cardiac risk, an expanded test panel may include the following: lipoprotein A, ferritin, magnesium, fibrinogen, CRP, homocysteine, coenzyme Q10, vitamin E, lipid peroxidase and testosterone.
Lipoprotein A
Expanded lipid testing would include Lipoprotein A, a lipid protein marker associated with oxidative stress, and a genetics marker for atherosclerotic vascular disease. When vessels become vulnerable to aging and oxidative stress, lipoprotein A will form aggregates, leading to plaque buildup. Reference range for lipoprotein A is 0-30 mg/dl; optimum levels would be <20 mg/dl. However, anything greater than 14 mg/dl could suggest a problem.
Iron
Ferritin is a serum marker for the storage form of iron. Men have a much higher optimum range than women. When women reach menopause and stop menstruating, their iron stores build up. As part of the normal senescence of an RBC, the liver helps break down and remove old, dying red cells (lifespan of an RBC being about 120 days). If there is liver impairment or excess iron, the iron is stored in the body’s tissues. The buildup of iron is most problematic because it can lead to hepatobiliary hypertension. Ferritin’s reference range for women is 10-291 ng/ml and for men the range is 22-322 ng/ml.
Magnesium
Magnesium is an important nutrient; it is required for nearly all extra- and intra-cellular reactions. It promotes nerve and muscle function, helps convert glucose to energy, aids in utilization of calcium, helps vessels dilate and increases blood flow. So why do so few doctors use this marker for cardiovascular issues? Serum magnesium is not a good indicator of true magnesium, but RBC magnesium is. Most magnesium is concentrated in bones, muscles and cells. Muscle testing for magnesium is probably most accurate. The same holds true for assessing foliate levels. Normal plasma RBC magnesium levels range from 1.8-2.6 mg/dl. A better methodology is to analyze the magnesium in pack RBC, which spins the cells down and removes the plasma, and only analyzes the red cells. Optimum RBC magnesium for ppm packed cells is 40-80.
Fibrinogen
Fibrinogen is a great marker for hypercoagulability. I use this as a screen for risk of stroke or clot formers. Fibrinogen is complex protein manufactured in the liver, which is converted into fibrin in the blood stream. It is considered an acute phase protein reactant, so inflammation and injury to the vascular network can set off the cascade of clotting. Too much fibrinogen can be detrimental. Traditional reference range runs 200-400 mg/dl; my recommended optimum range is 150-300 mg/dl.
C-Reactive Protein
CRP is another inflammatory marker. It is manufactured by the liver in response to acute phase reactants. Similar to ESR, CRP does not indicate the source of the inflammation. Acute phase reactants can be due to trauma or bacterial infections. Remember to order a highly sensitive CRP lab test; there is a difference in methodology. Typical reference range values are 0-4 mg/L. My cutoffs are different for men and women, partly because women’s menstruation causes more variation inflammation. Men should be <0.5 mg/L and women should be <1.5 mg/L. If a patient’s CRP comes back higher than optimum, search through his or her history to find the site of acute phase reactant. Be sure to assess teeth; this can offer an important sign when discerning infection/inflammation.
Next issue’s column will assess homocysteine, coenzyme Q10, vitamin E, lipid peroxidase and testosterone.
 Shaida Sina, ND has been working in the field of medicine for more than 20 years. She received her BS from the University of Maryland, in the School of Medicine’s Department of Medical and Research Technology. During her first 10 years in health care, she worked in the field of laboratory medicine, where she ultimately became lead technologist of a reference infectious disease laboratory. Sina began her studies in natural medicine in 1995 at SCNM and was the first naturopathic physician to do a clinical rotation at Mayo Clinic, where she trained in reproductive endocrinology. Her areas of clinical focus include women’s health care, pediatrics and general family practice.
Shaida Sina, ND has been working in the field of medicine for more than 20 years. She received her BS from the University of Maryland, in the School of Medicine’s Department of Medical and Research Technology. During her first 10 years in health care, she worked in the field of laboratory medicine, where she ultimately became lead technologist of a reference infectious disease laboratory. Sina began her studies in natural medicine in 1995 at SCNM and was the first naturopathic physician to do a clinical rotation at Mayo Clinic, where she trained in reproductive endocrinology. Her areas of clinical focus include women’s health care, pediatrics and general family practice.