Hal Brown, ND, DC, RAc
This article is based on a presentation I made at the 2015 BMO Vancouver Marathon Expo, in British Columbia, on the use of regenerative injection therapies for running injuries. For the purposes of this discussion I will include prolotherapy, neural prolotherapy, prolozone and platelet rich plasma (PRP) – all within the category of Regenerative Injection Therapies (RIT).
The February 2011 issue of Runner’s World magazine published the results of a reader’s survey of the most common injuries experienced by runners; 40% of running injuries were knee injuries, and 13% of runners suffered knee pain within the past year.1 This survey was consistent with other surveys2 in highlighting knees as the most common area of injury in runners.
 The Big 7 Body Breakdowns
The Big 7 Body Breakdowns
The Runner’s World article1 listed the following 7 injuries as the most common among runners:
- Patellofemoral Syndrome
- Achilles Tendinitis
- Hamstring Issues
- Plantar Fasciitis
- Shin Splints
- Iliotibial Band Syndrome (ITBS)
- Stress Fracture
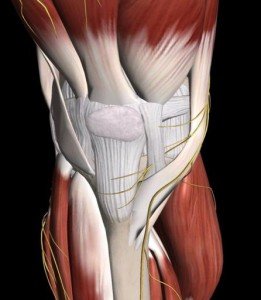
Patellofemoral syndrome (PFS) is a common diagnosis (frequently referred to as “runner’s knee”); however, it is often a catch-all term for what should be properly referred to as anterior knee pain. This can be due to many causes, so all anatomic structures and injuries must be considered: patella tendinosis; chondromalacia patella; meniscal damage; saphenous and femoral cutaneous nerve inflammation or entrapment; medial or lateral patella-femoral ligament injury; MCL; ITBS; gracilis, sartorius or popliteus tendons; and the ubiquitous patella femoral tracking. As well, no knee workup is complete without considering ankle/foot, hip, and pelvis assessment.
When pain first occurs, runners may continue on, often discovering that many symptoms are transient. Perhaps the body is adapting and compensating by loading stress onto other areas, only to show up later. Perhaps “running through” the pain is a strategy when high goals are at stake. A chronic dysfunction may appear as a gradually increased pain that eventually causes a runner to take note and stop. A sudden and acute trauma may also be the instigating factor. The usual scenario is that a competent runner is suddenly faced with an acute pain that limits or disables him or her from performing at an optimal level. The most common initial response to an injury is to take a rest from the running that is aggravating it, to let the body heal itself. The use of ice and/or anti-inflammatory medication is very common and might permit someone to get back to running quickly; however, it might also, as we will see, be counterproductive.
Making a Correct Diagnosis
The most important task in using RIT is to first make a correct diagnosis of the problem. A pain doctor using prolotherapy is a physician looking for the cause of the problem, not a treatment in search of a patient. Prolotherapy/RIT might sometimes be a bit like horseshoes and grenades, in that while close may count, being specific counts more.
James Cyriax3 described the basic principles of orthopedic medicine as follows:
- Every pain has a source
- Treatment must reach the source
- Treatment must benefit the source in order to relieve the pain
- Most sources of pain in the musculoskeletal system can be localized to a specific tissue
Effective RIT therapy depends upon a diagnostic method that isolates the cause of pain, whether in ligaments, tendons, muscles, capsules, intra-articular structures, or bursa. Because nerve density in ligaments and tendons is very high, most tenderness is noted over ligaments and tendons. Nerve structures must also be considered as a source of pain, whether subcutaneous4 or entrapped.5
As naturopathic doctors, it is also critical to view the pain patient as requiring the same health assessments as any other patient, and to ensure that the healing of mechanical structures is supported by the optimal well-being of the patient.
Inflammation & Injury Pathophysiology
Systemic and cellular inflammation is understood to lead to chronic degenerative conditions such as heart disease, cancer, rheumatoid arthritis, and asthma; clearly, pathological inflammation is undesirable. There is generally confusion and controversy regarding the understanding of the cause of orthopedic pain, when so many conditions are attributed to “inflammation.” It seems facile to tell a patient that their pain is tendonitis of whatever structure is hurting, as this seems to be a treatment looking for a diagnosis. It’s like telling a patient he has elbowitis or lumbaritis. Before injectable steroids became available in the 1950s, orthopedic diagnosis was based on the assessment of the tissues where the pain manifested, whether tendons, ligaments, muscles, etc.3 Steroid injections, when they appeared, were so miraculous, that their anti-inflammatory effect became the evidence of the diagnosis – inflammation. Then followed a flurry of the naming of the “itis”: epicondylitis, tendonitis, bursitis, fasciitis, and so forth.6 Inflammation is clearly present in acute injuries, but it is not necessarily the cause of the pain; rather, it is the attempt of the body to heal the injury.
Inflammation, however, is not seen in chronic injuries to a significant degree. Patellar tendinopathy is a degeneration of the inferior patella tendon, due to repetitive and/or chronic overloading that exceeds the tendon’s capacity. Histological evidence indicates that degenerative damage begins long before the onset of symptoms. Rather than tendonitis, a more correct term would be tendinopathy, or tendinosis, which refers to tendon degeneration and tearing without inflammation,7 usually associated with overuse.8
As another example, Achilles tendonitis is frequently associated with calcaneal inflammation. However, inflammatory lesions are rarely seen in clinical, imaging, and histological examinations.9,10 Fatty or mucinoid degeneration within the peripheral section of the Achilles tendon has been shown to constitute the lesion.11
Cortisone injections do have a place, and they often provide dramatic instant relief and, occasionally, long-lasting benefit. But overall, the use of cortisone has been shown to have a temporary benefit. As an example, the Cochrane Collaboration indicates that cortisone injections for knee osteoarthritis are effective, but of short-term benefit,12 not effective for rotator cuff injuries,13 and provide only temporary benefit for Achilles tendonitis.14 Importantly, as well, because of the catabolic effect of corticosteroids, tissue destruction and wasting can occur when used repetitively.
What about ice? In 1978, in The Sports Medicine Book, Dr Gabe Mirkin coined the acronym RICE, for Rest, Ice, Compression, and Elevation.15 Since then, the application of ice on acute injuries has become almost ritualistic, as it is assumed that inflammation is the cause of the pain. Today, Dr Mirkin has countered his initial assertion:
Coaches have used my “RICE” guideline for decades, but now it appears that both Ice and complete Rest may delay healing, instead of helping.
(Gabe Mirkin, MD)16
This is because ice causes blood vessels near the injury to constrict, which shuts off the blood flow that brings in the healing cells of inflammation.16 Importantly, early mobilization is also critical to successful healing.17
Wound healing utilizes the same biological mechanisms as the immune system – ie, inflammation – to kill germs. Inflammation is required in injury for healing to occur; neutrophils rapidly invade, followed by macrophages and other inflammatory cells. This inflammatory response coincides with tissue repair, regeneration, and growth.18 Macrophages remove necrotic debris and produce growth factors such as IGF-1, which is important for the healing of damaged tissues.19 In one study, 2 groups of mice were compared by inducing similar injury into muscles. One group was normal; the other was unable to form an immune response. The inhibited group did not display wound-healing; the normal group, in contrast, healed and recovered from the injuries, demonstrating high macrophage activity and IGF-1 in the recovered muscle.20
RIT Theory & Inflammation
The basic mechanism of prolotherapy is the same as the immune/inflammatory healing response of the body. A proliferating substance, commonly dextrose 10-25%, is injected into the affected ligaments or tendons, which leads to localized inflammation. This inflammation triggers the same wound-healing cascade of inflammatory cells as might an injury or infection. There are many factors at work here: the IFG-1 from macrophages, oxygen from red blood cells, and – significantly – the growth factors in platelets. Growth factors stimulate the formation and deposition of collagen. Ligaments, tendons, and cartilage are primarily composed of collagen,21 which is critical for the repair, growth, and regeneration of these tissues. The regeneration that occurs after injection is of actual new ligaments and tendons, not – as is mistakenly understood – of scar tissue. The new tissues are thicker, tighter, more flexible, and contain fibers of varying thickness, testifying to the new and ongoing regeneration.22
Platelet-Rich Plasma (PRP)
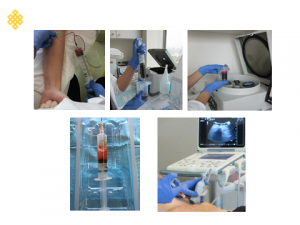
The use of platelet-rich plasma is an extension of this principle. Platelets are not just for clotting, immune response, or angiogenesis. Four percent of blood volume is platelets. They are the first cells to arrive at the injury site, they initiate the healing cascade, and – importantly – they contain the growth factors required for collagen regeneration.23 Put simply, instead of stimulating an inflammatory healing cascade to bring platelets and growth factors to the site of injury, with PRP the platelets are extracted from whole blood via a variety of centrifuge methods (Figure 1), and injected in high concentrations directly into the target sites (Figure 2). The result is an enhanced healing response, with less discomfort and fewer treatments.
Additional Regenerative Injections

Other substances than dextrose are used as irritant or shock agents to stimulate inflammation. These may include various combinations of phenol, glycerine, sodium morrhuate (from cod liver oil), or pumice.
Neural prolotherapy, or subcutaneous nerve injection, utilizes a 5% dextrose solution injected into inflamed or entrapped subcutaneous nerves. It has been demonstrated that chronic inflammation or damage of these C-fiber nerves can produce arthritic changes in joints, and that the healing of these nerves via injection can reduce pain and lead to joint regeneration.24 For example, saphenous nerve injury can contribute to medial and anterior knee pain (Figure 3).
Prolozone involves the injection of ozone gas into damaged tissues including joints. Dr Shallenberger states, “Prolozone works by improving oxygen utilization in a localized area of damaged connective tissue, allowing it to heal, and to restore full function.”25
Testosterone and human growth hormone function as releasing/signaling molecules, altering cell wall flexibility, modifying pain perception, and adjusting blood flow at the wound site.26
Most recently and dramatically, stem cell therapies (in which adipose-derived stromal cells are injected in combination with PRP) are becoming practical in a clinical setting. This multipotent cell replenishment source is effective for enhanced musculoskeletal healing.27 Other methods that isolate stem cells from fat or marrow have been demonstrated to exponentially increase the regenerative capability of tissue.28
Evidence for Regenerative Injection Therapies
There is a vast body of literature today that supports the clinical efficacy of RIT.
One literature review of 44 case series – including 2 non-randomized controlled trials, 9 randomized controlled trials, 2443 patients, and 1478 musculoskeletal structures – demonstrated level 1 and 2 evidence to support the use of dextrose prolotherapy for osteoarthritic pain and function, tendinopathies, myofascial pain syndrome, sacroiliac pain, and myofascial pain syndrome.29
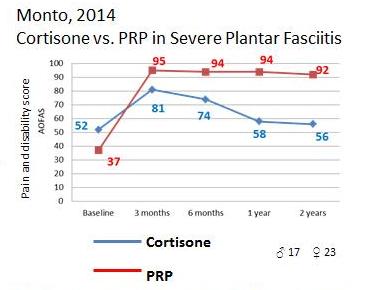
In 2 studies of PRP vs cortisone treatment for lateral epicondylitis and severe plantar fasciitis, it was shown that although both cortisone and PRP provided close to equal relief after 3 months, continued and significant benefit in the PRP groups remained for 2 years, whereas the cortisone groups reverted to baseline (Figure 4).30,31
Among many examples, the effectiveness of RIT has been demonstrated for patella tendinopathy,32 jumper’s knee,33 chondromalacia patella,34 Achilles tendinosis,35 knee instability,36,37 chronic low back pain,38,39 hip pain and labral tears.40
Candidates for Regenerative Injection Therapy
The RIT candidate has:
- an unresolved pain and/or dysfunction for greater than 3 months
- instability due to laxity
- connective tissue damage, as evident by pain and/or tenderness over ligaments, tendons or nerve sheaths
Summary
Going back to our original running injury, most runners would take a break from painful activity and commonly ice the injury and/or use anti-inflammatory medications. If they can resume activity in a reasonable time, they would return without further treatment. Many people apply the “if you ignore it, it will go away” principle, which often does work. But what happens when they don’t get better? The next step is to see a practitioner of some kind (eg, PT, DC, RMT, RAc, ND), for treatments such as IMS*, TRP† injection, ART‡, massage, manipulation, mobilization, exercise, electric therapies (laser, ultrasound), taping, bracing, arnica, glucosamine sulphate, and other supplements. Perhaps a visit to a sports physician or physiatrist. Much of the time, these treatments are successful. When resolution is not satisfactory, then imaging using X-ray, ultrasound, or MRI might be performed. Although pathologies may be noted, unless they can be correlated with the clinical picture, the imaging report is often treated instead of the patient.
There is a case to be made for the treatment of acute injuries, such as those patients who have re-injured previously-treated areas, or in cases where performance is critical. Many RIT doctors, myself included, will often receive treatment soon after our own injuries, as will experienced and educated patients. Generally however, the case for RIT is better made in chronic cases, after “everything has been tried.” If the injury is indicated for RIT, that is ligament and/or tendon laxity and damage, probably not much else will help this problem; however, most patients would prefer to resolve their pain with less invasive methods and may only turn to RIT when nothing else has helped.
As a treatment of “last resort” in many cases, patients are willing to endure discomfort, in the hopes and likelihood of achieving excellent outcomes.
*IMS=intramuscular stimulation; †TRP=trigger point; ‡ART=active release technique
Case Study 1
Knee Prolotherapy
Danita, age 45, is a former National Canadian Olympic Team rower, and an active runner and cyclist. In 2011 she came for a consultation, complaining of anterior knee pain of 14 months’ duration. Because of debilitating pain, she could not carry her child upstairs, walk a block, or cross a street. She had received a diagnosis of patellofemoral pain syndrome (PFPS) and was on a surgery wait-list. She was receiving physio treatment, which gave some relief, but she was still disabled.
Assessment & Treatment
She was assessed with A & P cruciate instability and medial collateral ligament instability and tenderness. In the first month she received prolotherapy injections 3 times. Within 5 weeks she was cycling again and could do a frog-kick swimming. She received 2 more treatments over the next 3 months.
Follow-up
Within 5 months of initiating treatment, she was back to 80% normal activities and exercise. Four years later, she reports she is at 95% recovery, running 10 km with no pain, and doing all desired activities, including boot-camp training. She has been enthusiastic about her recovery.
Case Study 2
Hip Pain
Debbie, age 50, was a competitive Master’s Track racer. Her chief complaint was right hip pain and being unable to run for 5 years. In 2005 her right leg suddenly “collapsed,” and she had hamstring and hip pain. She had had numerous treatment modalities, including: muscle balance exercises, physical therapy, massage therapy, chiropractic, and intramuscular stimulation, all of which were helpful for a time. She experienced frequent aggravations, requiring weeks of recovery, and felt worse when her stride was more powerful. Imaging included: MRI (“inconclusive”), arthrogram (unremarkable), X-ray (early hip osteoarthritis), and CT scan (disc bulges). She also had other running injuries of the knees and ankle.
Treatment
Between April 2010 and June 2010, she received 5 prolotherapy treatments. In June 2010 she received PRP 3 times. By September 2010, she reported feeling more “solid,” her performance was improving, and she was beginning to race again, running 6-8 km intensely and without re-injury. From September 2010 to May 2011, she received 3 more PRP treatments.
The injection treatments were aimed at multiple injury sites, which included the hip joint, labrum, pectineus muscle, and obturator externus tendons in the groin. The posterior hip was also treated, as were the insertions of the gemelli and obturator muscles. The lumbar facets, iliolumbar ligaments, and SI joints were also treated. She also received a comprehensive naturopathic treatment regime, spinal adjustments, and supplementation; several health issues were also addressed with naturopathic methods. The healing of any tissues requires the health of the entire body.
Follow-up
In July 2011, she went back to competition and ran the World Masters Athletics Championship. She finished 9th out of 27 in the 1500, running her best time since 2005.
Since then, her performance has continued to improve. In 2013 she placed 4th in the 800 at the World Masters Athletics in Brazil, and in 2013 she placed 3rd in the 1500, and 2nd in the 800, at the World Masters Games in Italy.
 Hal Brown, ND, DC, RAc, is a graduate of CMCC (1977), OCNM (1989), and ICTCM (1993). He is a cofounder and partner in Integrative Healing Arts (1983), where he practices in Vancouver BC. He is a former chair of Physical Medicine and instructor at BINM and served as Chair of the Manipulation Advisory Committee, CNPBC (2005). Dr. Brown is a contributor to the Textbook of Naturopathic Physical Medicine (2007) and NDNR (2007). Past presentations include: NW Naturopathic Convention (2008), BCNA (2004), and the Third International Fascia Research Congress (2012).
Hal Brown, ND, DC, RAc, is a graduate of CMCC (1977), OCNM (1989), and ICTCM (1993). He is a cofounder and partner in Integrative Healing Arts (1983), where he practices in Vancouver BC. He is a former chair of Physical Medicine and instructor at BINM and served as Chair of the Manipulation Advisory Committee, CNPBC (2005). Dr. Brown is a contributor to the Textbook of Naturopathic Physical Medicine (2007) and NDNR (2007). Past presentations include: NW Naturopathic Convention (2008), BCNA (2004), and the Third International Fascia Research Congress (2012).
References:
- Aschwanden C. The Big 7 Body Breakdowns. February 3, 2011. Runner’s World Web site. http://www.runnersworld.com/health/the-seven-most-common-running-injuries. Accessed September 1, 2015.
- Fredericson M, Misra AK. Epidemiology and aetiology of marathon running injuries. Sports Med. 2007;37(4-5):437-439.
- Cyriax JH. Cyriax’s Illustrated Manual of Orthopaedic Medicine. 2nd Oxford, England: Butterworth-Heinemann; 1993.
- Lyftogt J. Neural Prolotherapy: Extinguishing Neuropathic Pain [seminar notes]. From: Neural Prolotherapy workshop; April 12-14, 2013; Seattle, WA.
- Lam KH. Ultrasound Guided Hydrodissection of Peripheral Nerves as a Treatment Option For Chronic Musculoskeletal Pain Failed Manual Therapy, Using Different Solutions Including Platelet Rick Plasma. Ultrasound in Medicine & Biology. 2015;41(4):S91.
- Johnson ML. Prolotherapy & Connective Tissue Damage Syndrome: Why am I hurting, and no one seems to know what is wrong? Journal of Prolotherapy. 2009;1(1). Available at: http://tinyurl.com/q9psq9e. Accessed September 1, 2015.
- Ferrero G, Fabbro E, Orlandi D, et al. Ultrasound-guided injection of platelet-rich plasma in chronic Achilles and patellar tendinopathy. J Ultrasound. 2012;15(4):260-266.
- Khan KM, Maffulli N, Coleman BD, et al. Patellar tendinopathy: some aspects of basic science and clinical management.Br J Sports Med. 1998;32(4):346-355.
- Alfredson H, Lorentzon R. Chronic tendon pain: no signs of chemical inflammation but high concentrations of the neurotransmitter glutamate. Implications for treatment? Curr Drug Targets. 2002;3(1):43-54.
- Leach RE, James S, Wasilewski S. Achilles tendinitis. Am J Sports Med. 1981;9(2):93-98.
- Schepsis AA, Jones H, Haas AL. Achilles tendon disorders in athletes. Am J Sports Med. 2002;30(2):287-305.
- Bellamy N, Campbell J, Welch V, et al. Intraarticular corticosteroid for osteoarthritis. April 19, 2006. Cochrane Web site. http://tinyurl.com/oy3nynu. Accessed September 1, 2015.
- Buchbinder R, Green S, Youd JM. Corticosteroid injections for shoulder pain. January 20, 2003. Cochrane Web site. http://tinyurl.com/o7lpfev. Accessed September 1, 2015.
- Kearney RS, Parsons N, Metcalfe D, Costa ML. Injection treatment for painful Achilles tendons in adults. May 26, 2015. Cochrane Web site. http://tinyurl.com/ngyp9qq. Accessed September 1, 2015.
- Mirkin G, Hoffman M. The Sports Medicine Book.Boston, MA: Little Brown & Co; 1978.
- Mirkin G. Why Ice Delays Recovery. March 16, 2014. Available at: http://drmirkin.com/fitness/why-ice-delays-recovery.html. Accessed September 1, 2015.
- Van den Bekerom MP, Struijs PA, Blankevoort L, et al. What Is the evidence for rest, ice, compression, and elevation therapy in the treatment of ankle sprains in adults? J Athl Train. 2012;47(4):435-443.
- Tidball JG. Inflammatory processes in muscle injury and repair. Am J Physiol Regul Integr Comp Physiol. 2005;288(2):R345-R353.
- Baoge L, Van Den Steen E, Rimbaut S, et al. Treatment of skeletal muscle injury: a review. ISRN Orthop. 2012;2012:689012.
- Lu H, Huang D, Saederup N, et al. Macrophages recruited via CCR2 produce insulin-like growth factor-1 to repair acute skeletal muscle injury. FASEB J. 2011;25(1):358-369.
- Johnson DH, Pedowitz RA, eds. Practical Orthopaedic Sports Medicine and Arthroscopy. Hagerstown, MD: LWW Publishing; 2006.
- What is Prolotherapy? 2014. Journal of Prolotherapy Web site. http://tinyurl.com/nwgja7u. Accessed September 1, 2015.
- Lubkowska A, Dolegowska B, Banfi G. Growth factor content in PRP and their applicability in medicine. J Biol Regul Homeost Agents. 2012;26(2 Suppl 1):3S-22S.
- Weglein AD. Neural Prolotherapy. Journal of Prolotherapy. 2011;3(2):639-643. Available at: http://www.journalofprolotherapy.com/index.php/neural-prolotherapy/. Accessed September 1, 2015.
- Shallenberger F. Prolozone™ – Regenerating Joints and Eliminating Pain. Journal of Prolotherapy. 2011;3(2):630-638. Available at: http://tinyurl.com/pkqzx79. Accessed September 1, 2015.
- Ravin T. The Use of Testosterone and Growth Hormone for Prolotherapy. Journal of Prolotherapy. 2010;2(4):495-503. Available at: http://tinyurl.com/odhmv9l. Accessed September 1, 2015.
- Alderman DD, Alexander RW, Harris GR, Astourian PC. Stem Cell Prolotherapy in Regenerative Medicine. Journal of Prolotherapy. 2011;3(2):689-708. Available at: http://www.prolotherapy.com/Alderman_JOP%20article_2011.pdf. Accessed September 1, 2015.
- Regenexx is a Research Based Stem Cell Procedure. Regenexx Web site. http://www.regenexx.com/about-regenexx/research-based-stem-cell-procedure/. Accessed September 1, 2015.
- Hauser RA, Hauser MA, Baird NM. Evidence-Based Use of Dextrose Prolotherapy for Musculoskeletal Pain: A Scientific Literature Review. Journal of Prolotherapy. 2011;3(4):765-789. Available at: http://tinyurl.com/pzd4hdf. Accessed September 1, 2015.
- Monto RR. Platelet-rich plasma efficacy versus corticosteroid injection treatment for chronic severe plantar fasciitis. Foot Ankle Int. 2014;35(4):313-318.
- Gosens T, Peerbooms JC, van Laar W, et al. Ongoing positive effect of platelet-rich plasma versus corticosteroid injection in lateral epicondylitis: a double-blind randomized controlled trial with 2-year follow-up. Am J Sports Med.2011;39(6):1200-1208.
- Charousset C, Zaoui A, Bellaiche L, Bouyer B. Are multiple platelet-rich plasma injections useful for treatment of chronic patellar tendinopathy in athletes? a prospective study. Am J Sports Med. 2014;42(4):906-911.
- Kon E, Filardo G, Delcogliano M, et al. Platelet-rich plasma: new clinical application: a pilot study for treatment of jumper’s knee. Injury. 2009;40(6):598-603.
- Hauser RA, Sprague IS. Outcomes of prolotherapy in chondromalacia patella patients: improvements in pain level and function. Clin Med Insights Arthritis Musculoskelet Disord.2014;7:13-20.
- Monto RR. Platelet rich plasma treatment for chronic Achilles tendinosis. Foot Ankle Int. 2011;33(5):379-385.
- Ongley MJ, Dorman TA, Eek BC, et al. Prolotherapy – Ligament Instability of Knees: A New Approach to Treatment. Manual Medicine. 1988;3:152-154.
- Reeves KD, Hassanein KM. Long-term effects of dextrose prolotherapy for anterior cruciate ligament laxity. Altern Ther Health Med. 2003;9(3):58-62.
- Ongley MJ, Klein RG, Dorman TA, et al. A new approach to the treatment of chronic low back pain. Lancet. 1987;2(8551):143-146.
- Klein R, Eek B. Prolotherapy: an alternative approach to managing low back pain. J Musculoskeletal Medicine. 1997;May:45-49.
- Hauser R. Prolotherapy Research Hip Pain. GetProlo Web site. http://www.getprolo.com/prolotherapy-research-hip-pain/. Accessed September 1, 2015.



