Robin DiPasquale, ND, RH (AHG)
Constipation can be a major problem. It affects daily life. It can make or break someone’s day. Yet, statistics show that 1 in 6 Americans live with chronic constipation.1 It is estimated that $725 million dollars is spent yearly on laxatives.2 These can get things moving… but do not correct the underlying problem.
Some key rule-out diagnoses for acute constipation are colonic obstruction, appendicitis, diverticulitis, peritonitis, and possible stone obstruction from the gall bladder or kidneys. For chronic constipation, some key rule-outs include celiac disease, hypothyroidism, and irritable bowel syndrome (IBS), as well as inflammatory bowel disease and colon cancer.
Gastroenterologists have classified chronic constipation into 4 subtypes3:
- Slow-transit constipation
- Pelvic floor dyssynergia
- IBS with constipation
- Functional constipation
Functional constipation is defined as chronic idiopathic constipation that does not have a physiological cause. Research suggests that those using this subtype as the diagnosis have not looked deeply enough into possible etiologies.
Causes of Constipation
Dr J. H. Bundy, one of the Eclectic physicians and discoverer of the medicinal properties of Cascara sagrada, wrote the following back in 1878 about the causes of and contributors to constipation4:
- the nature of the diet
- deficiency or a faulty composition of the intestinal secretions
- disordered glands that pour their secretions into the intestines
- impairment of muscular power, which leads to a deficiency in the propelling power, which may result from nervous or mechanical influences
- congestion of the portal circulation
- normal secretions of intestinal juices interfered with
- deficiency in biliary secretions of a healthy character
- congestion of mucus membranes of intestines
- and [most frequently], resisting the calls of nature from carelessness or circumstances that prevent obedience at the proper time
Perhaps once all of the above have been thoroughly evaluated and addressed, there would be a place for the subtype of functional constipation. I would also include the sedentary nature of many people as a contributing factor.
The following statement, written by Dr W. G. Gibbons in 1903, understood the insidious impact of constipation on daily life, as well as the far-reaching toxicity issue this health problem presents:
Without question, the most frequent departure from the normal standard of health has relationship to the alimentary tract, with the great danger of auto-infection always in evidence. We should remember that what may be designed pathological constipation is not a disease of itself but only a functional disarrangement.5
Recommendations for Constipation
So, as Dr Bundy advises, first and foremost check on bowel habits and whether the patient is responding obediently to the call of nature at the proper time. This issue can begin very young. Many children in my office have told me that they are not allowed to be excused to the bathroom as need be while in school. This, along with the sedentary nature of children’s school days, can create a lifelong pattern of constipation. For some, the call of nature stops calling after an extended time of no response, which would then necessitate bowel retraining to reestablish peristalsis and normal function.
Secondly, evaluate the diet for potential food intolerances and sensitivities, and for low-quality foods or poor choices of food or food combining that may be contributing to the constipation. I have observed adverse reactions to foods lead to leaky gut and congestion in the whole alimentary tract. The elimination of dairy – a mucus-promoting and potentially binding food – is a dietary change that I’ve seen help correct constipation in some patients. Eliminating gluten has also produced noticeable improvement. Individual testing is optimal for best outcomes.
Thirdly, evaluation of the gut-brain axis may reveal reasons for altered secretions of the organs and glands of the whole digestive system, including secretions from stomach and intestines, biliary secretions from the liver and gall bladder, and pancreatic enzyme secretions. The major player in this arena is cranial nerve X, ie, the vagus nerve, also named the “wandering nerve” because of its far-reaching impact in the body.
The gut-brain axis is a bidirectional neurohumoral communication system. If the GI tract is not working properly, brain issues can result. The intestinal microbiome impacts brain development.6 Imbalanced gut flora, as well as leaky gut as a result of inflammation, can also affect brain neurochemistry.6
Conversely, if the brain is not working properly, you can have GI issues. The brain controls the movement of food through the intestines – motility, the release of gastric and pancreatic enzymes, and liver/gallbladder bile release. The vagus nerve carries information to and from the brain. The brain activates the brain stem, and the brain stem activates the vagus nerve. The vagus nerve activates the enteric nervous system. The enteric nervous system then stimulates secretions, motility, and function of the gut. Loss of digestive function can thus be linked back to loss of brain function and/or loss of vagus nerve function. An underactive vagus nerve may express with gastroparesis, decreased heart rate, stomach pain, nausea, heartburn, stomach spasm, weight loss, and/or maldigestion.
Three observations in the office can help evaluate whether vagus nerve function is diminished: 1) bowel sounds are diminished; 2) the uvula does not rise when the patient says, “ahhh”; and 3) the gag reflex is not very responsive.
Stimulating the Vagus Nerve
The vagus nerve’s plasticity and function can be improved with neurological exercises that stimulate the muscles in the back of the throat (which in turn stimulates the vagus nerve). These should be repeated daily for 2-4 weeks.6
Gargling: Gargle long enough and deep enough to make it an exercise. Drink several 8-oz glasses of water daily by gargling each mouthful.
Singing loudly: Sing in your car, sing while gardening, or cooking, or cleaning; sing while driving, or while working out; chant following meditation; and go to a kirtan or a sing-along whenever you can.
Gagging: Stimulate the gag reflex several times a day; use a tongue depressor, a spoon, or your finger, though only to the point of gagging, not vomiting.
In addition, coffee enemas’ ability to reestablish motility works in 2 ways, both through the vagus nerve. The distention activates the stretch receptors, which activates the vagus nerve. The caffeine acts on cholinergic receptors, thereby restoring plasticity to the vagus nerve.6
Herbs for Constipation
Following is an overview of a few herbs to consider when working with patients troubled by constipation.
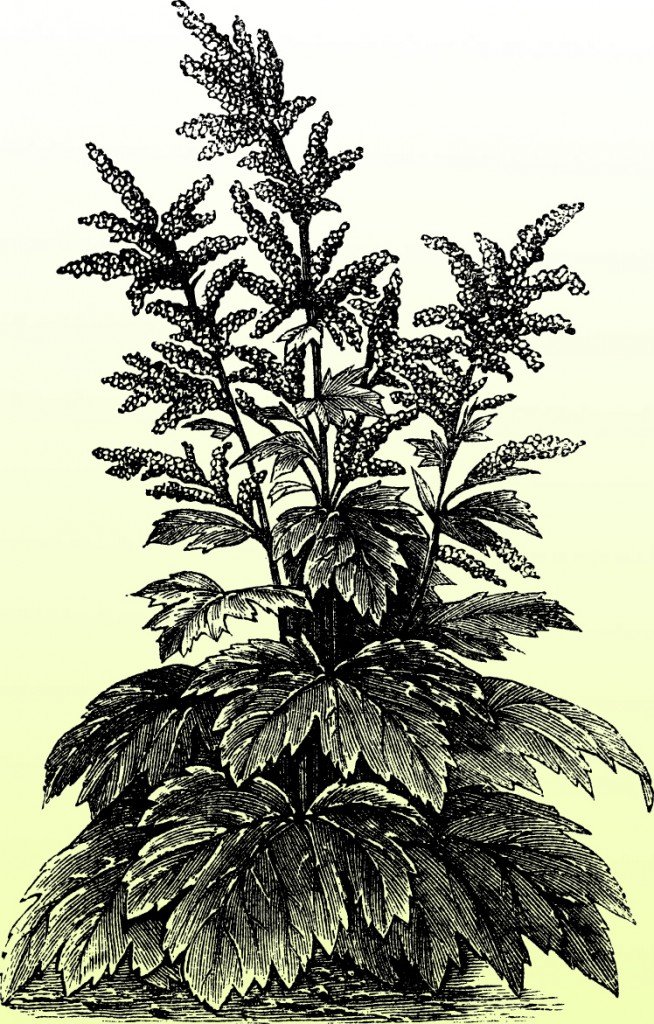
Frangula Purshiana, formerly Rhamnus Purshiana, common name Cascara Sagrada
Cascara is often termed “sacred bark.” Of all the herbs used for constipation, this one stands out because of its ability to restore tone and function to the intestine. Cascara bark must be aged for 1 year before it is used to make medicine. The action of Cascara is dose-dependent. A dose of 3-10 minims restores function; 5-20 minims QID is a laxative; 20-60 minims AM and PM is cathartic. One minim is equal to 1/480 fluid ounce, which equals about 1.875 drops.
Considered a bitter tonic, Cascara can increase gastric juices, bile secretions, and pancreatic juices, but will not increase salivary secretion. It has been suggested that Cascara assumes nearly all the favorable or desirable indications of the gastric, hepatic, and intestinal laxative/cathartic herbs, with few undesirable side effects.7 It acts upon the sympathetic nervous system through the vasomotor system, stimulating the muscular and secreting apparatus of the entire alimentary tract, influencing the glandular system, and increasing peristaltic function. Rather than mechanically liquifying and emptying the intestinal canal, Cascara restores normal elasticity and tone, initiates peristalsis, and gets things moving. Cascara is especially indicated in torpidity (loss of motion or power of exertion) or atonicity. The Eclectic physicians report that Cascara can single-handedly relieve bowel torpidity, whereas other laxative herbs can only work effectively when given in combination.8
Cascara has been found in nervous maladies to assist the action of nerve tonics. And there are some nervine herbs that will increase the action of Cascara, including Berberine aquifolium and Avena sativa.8 A list of nervine herbs to consider can be found later in this article.
As a cure for chronic constipation, take 2-10 gtt of Cascara tincture 3 to 5 times a day. After a few days, a normal bowel movement in the AM should take place. Once regular evacuation is achieved, the dose can be gradually decreased, down to 1 gtt in the AM, and 1 gtt in the PM, then eventually discontinued.
According to Ellingwood, if constipation [presumably impaction in this case] pre-exists, flush the bowels first with a laxative, then begin Cascara in small doses. Large doses can produce colic.4
Cassia Acutifolia, Alexandrian Senna
This laxative herb is one of the most commonly used in our current time. Senna has a narrow but important sphere of medicinal application, best used specifically for temporary relief of constipation. Senna is prepared from the dried leaves of this Middle Eastern Fabaceae family plant. Its action is exerted primarily on the small intestine, augmenting the mucous secretions and inducing peristaltic motion. Higher doses can cause gripping pains, as well as catharsis. A simple and palatable preparation results from making a strong infusion of the senna leaves, then adding prunes or figs and allowing these fruits to soak in the infusion. Eat 1 prune or fig several times per day to get things moving.
If using senna in patients with atonic or torpid bowels, adding ginger, cayenne, or black pepper is recommended. Little or no effect on hepatic function is seen when taking senna – the opposite of Cascara. If more liver movement is desired, combine senna with Veronicastrum virginica (old name is Leptandra virginica, Culver’s root, or black root). For tonic, laxative, and carminative actions, combine senna with rhubarb (Rheum officinalis) and peppermint (Mentha piperita). Ginger (Zingiber officinale) and jalap (Ipomoea purga) can be combined with senna for biliousness. One of the famous formulas in the late 1800s was Compounded Licorice Powder – a combination of senna, licorice, fennel, sublimed sulphur, and sugar – given for issues of constipation.4,5
Rheum Officinale, Turkey Rhubarb
Rheum has bitter-like effects that stimulate digestion, improve appetite, promote chyle* formation, and augment bile flow. It has an astringent action, acting specifically on the duodenum; being astringent, it does not augment mucosal secretions throughout the GI tube. If the GI tract is debilitated, it will tone, to a degree, and if it’s overactive, it will have some restraining action. Rheum does increase intestinal muscular action, enhancing peristaltic movement.4
Professor John King, MD, originated the Syrupus Rhei Et Potassae Compositus – the syrup of rhubarb and potassa [potassium carbonate]. It contains Indian rhubarb, goldenseal, and cinnamon, 1 oz of each, and would be macerated for 6 hours in 1/2 gallon of brandy over gentle heat. This was then percolated with the other 1/2 gallon of brandy, then combined with 1 oz carbonate of potassa, 4 lb of sugar, and 20 minims of oil of peppermint. John Uri Lloyd replaced the sugar with glycerine to eliminate the possibility of fermentation; this preparation was named Glyconda, and it continues to be used today. This neutralizing cordial is most indicated for a sour stomach, to neutralize excessive acidity. The tongue is broad, coated uniformly white; mucous membranes are pale, and there are sour eructations. It is especially useful for children with gastric disorders. When given to nursing mothers, it relaxes the infant’s bowels. In the case of diarrhea, astringent herbs can be added, and with constipation, a mild laxative herb can be added.4,8
The frequency of acid reflux and heartburn is of an epic scale in our culture today, with constipation often being an underlying condition… If one end of the tube is blocked, it makes sense that things will bubble up on the other end. It continues to amaze me in clinical practice, the number of infants that are being diagnosed with reflux and put on proton-pump inhibitors. This is surely the beginning of a lifetime of digestive difficulties. We have other options available:
Aloes Socotrina, Cape Aloes
Aloes (aka aloe) acts through irritation of the mucous membranes, in particular in the large intestine. There is some increase in bile production with aloes, but less than with Cascara. Taking aloes yields a watery diarrhea from weakness, followed by an irritative action upon the bowels. According to Ellingwood, people with hemorrhoids should avoid aloes [referring most likely to its latex component].4
An eclectic formula from Dr O. G. Carroll, containing 2 parts wormwood (Artemisia absinthium) and 1 part cape aloes, was indicated in acute conditions featuring pain and irritation. The wormwood acts on the upper GI tract, whereas the cape aloes is a slowly-acting large intestine purgative which empties the bowl within 10-15 hours.9
Additional Remedies
Epsom salts, containing magnesium sulfate, can be taken as a laxative to clear the colon. It is often used for colon prep before a colonoscopy, and can be used in constipation on an acute basis. The magnesium increases the efficiency of oxygen utilization, which serves to increase blood circulation to the intestinal smooth muscles and help with peristalsis. The sulfates help eliminate and flush out internal toxins from the colon lining. Use only food-grade Epsom salts. Dosing varies by body weight and constitution of each individual. A dose of 1-2 tsp in 8 oz of water, taken every 1/2 hour for a total of 2-4 doses, should produce a purging effect 4-6 hours later. I have found it to be more effective to ingest the salts within a shorter time period, dosing closer together rather than spreading them out over a longer period of time. This will give a concise cleansing of the colon that will not be prolonged over many hours. Sodium chloride can also be used in this way, as can castor oil.
The nervous system plays a major role in digestive disorders. In such cases, including nervine herbs with any laxative will support deeper resolution of the constipation. Nervine tonics that can be useful in rejuvenating the nervous system include Avena sativa, Scutellaria officinalis, and Hypericum perforatum. There are many nervine relaxants, including Tilia tomentosa, Leonurus cardiaca, Passiflora incarnata, Piper methysticum, and Melissa officinalis. The antispasmodics have a significant role in constipation because so much tension is held in the smooth muscles of the entire GI tract. We know well this action with Viburnum opulus, Viburnum prunifolium, and Actea racemosa because of their effectiveness in female reproductive health. Two other antispasmodic herbs are well to be considered in the case of constipation – Atropa belladonna and Lobelia inflata.
Atropa Belladonna
The Eclectic physicians used this herb often. The influence of belladonna as an antispasmodic against involuntary muscular action confers its value in obstinate constipation as well as the spasms of colic.4 Because of its alkaloids and the potential for toxicity, low dosing is recommended. Ellingwood suggests 10 gtt of the specific medicine in 4 oz of alcohol, and then dosing this as you would a strong tincture. Ten gtt of this dilution in a 4-oz mixture given in dram doses is recommended for children.4
Lobelia Inflata
The writings on Lobelia in the Eclectic books touch on the extreme virtue of this herb in relation to many, if not all, organ functions. Ellingwood writes about its ability to assist the nervous system and the essential vital force within the system to “reassert themselves and obtain complete control of the functional action of every organ.”17
For constipation, Lobelia is said to thoroughly relax muscular spasm and encourage peristalsis.4 The herb can relieve many cases of chronic constipation, including obstipation [severe constipation].18
Closing Comments
Herbal medicine has much to offer in the resolution of constipation; however, even with the effective actions of properly chosen herbs, lifestyle choices generally play the major role. Daily exercise or movement, proper selection of foods, deep and rejuvenating sleep, and management of anxiety or stress are essential in keeping things moving.
*Chyle is a term referring to a milky bodily fluid consisting of lymph and emulsified fats, formed in the small intestine during digestion of fatty foods.8
 Robin DiPasquale, ND, RH (AHG), who has been practicing in the healing arts for over 30 years, is growing into one of the elders in the naturopathic medicine community. Practicing first as an herbalist, homeopath, and massage therapist led her to her calling as a naturopathic doctor. Dr DiPasquale served as faculty at Bastyr University for 15 years and returns yearly as a guest teacher. She currently practices in Madison, WI, at Red Lotus Healing Arts. Her eclectic healing tools include homeopathy, biotherapeutic drainage, herbal medicine, and gemmotherapy. For the last 7 years she has brought naturopathic medicine to patients through the U of WI Integrative Medicine program. Robin is published and teaches internationally. Her current passion is the study and practice of Family Constellation Therapy.
Robin DiPasquale, ND, RH (AHG), who has been practicing in the healing arts for over 30 years, is growing into one of the elders in the naturopathic medicine community. Practicing first as an herbalist, homeopath, and massage therapist led her to her calling as a naturopathic doctor. Dr DiPasquale served as faculty at Bastyr University for 15 years and returns yearly as a guest teacher. She currently practices in Madison, WI, at Red Lotus Healing Arts. Her eclectic healing tools include homeopathy, biotherapeutic drainage, herbal medicine, and gemmotherapy. For the last 7 years she has brought naturopathic medicine to patients through the U of WI Integrative Medicine program. Robin is published and teaches internationally. Her current passion is the study and practice of Family Constellation Therapy.
References
Rao SS. Health-Care Burden and Costs of Constipation and Fecal Incontinence: The Silent Afflictions. May 6, 2015. American Gastroenterological Association Web site. http://tinyurl.com/zrzmv5c. Accessed November 23, 2015.
Constipation: NIDDK. From NIH Publication No. 95-2754; July 1995. Right Diagnosis for Health Grades Web site. http://www.rightdiagnosis.com/artic/constipation_niddk.htm. Accessed November 23, 2015.
Prather CM, Subtypes of constipation: sorting out the confusion. Rev Gastroenterol Disord. 2004;4 Suppl 2:S11-S16.
Ellingwood F, Lloyd JU. American Materia Medica, Therapeutics, and Pharmacognosy. Sandy, OR: Eclectic Medical Publications. Portland, OR; 1983. First published Cincinnati, OH; 1919.
Boston District Eclectic Medical Society Meeting. September 15, 1903. The Eclectic Review. 1903;5-6:287.
Kharrazian D. Why Isn’t My Brain Working? Carlsbad, CA: Elephant Press; 2013.
Boston District Eclectic Medical Society Meeting. September 15, 1903. The Eclectic Review. 1903;5-6:289.
Boston District Eclectic Medical Society Meeting. September 15, 1903. The Eclectic Review. 1903;5-6:288.
Moore L. Classical Formulas in the Western Herbal Tradition. Self-published by Les Moore; 2002.





