Integrative Lifestyle Change: Reducing Obesogenic Stress
Erica Oberg, ND, MPH
Recommendations to adopt a “healthy diet” are ubiquitous, yet adopting and sustaining healthy behaviors remains a hurdle for both individuals and society at large. One challenge to sustained behavior change relates to common emotional responses to an increasingly stressful environment, including excess energy intake and unhealthy food choices. Although acute and chronic stress are recognized barriers to healthy dietary choices and increased physical activity, programs typically lack an intervention component that first addresses the psychoneuroendocrine contributions to obesity. The psychoneuroendocrine dysfunctions associated with stress are directly (physiologically) and indirectly (via cognitive and emotional pathways that affect health behaviors) obesogenic. These relationships are modeled in Figure 1. Further, improving lifestyle behaviors requires an intensive, personalized approach that addresses underlying causes in all domains that disrupt the neuroendocrine balance: physical, mental-emotional, spiritual, and social.
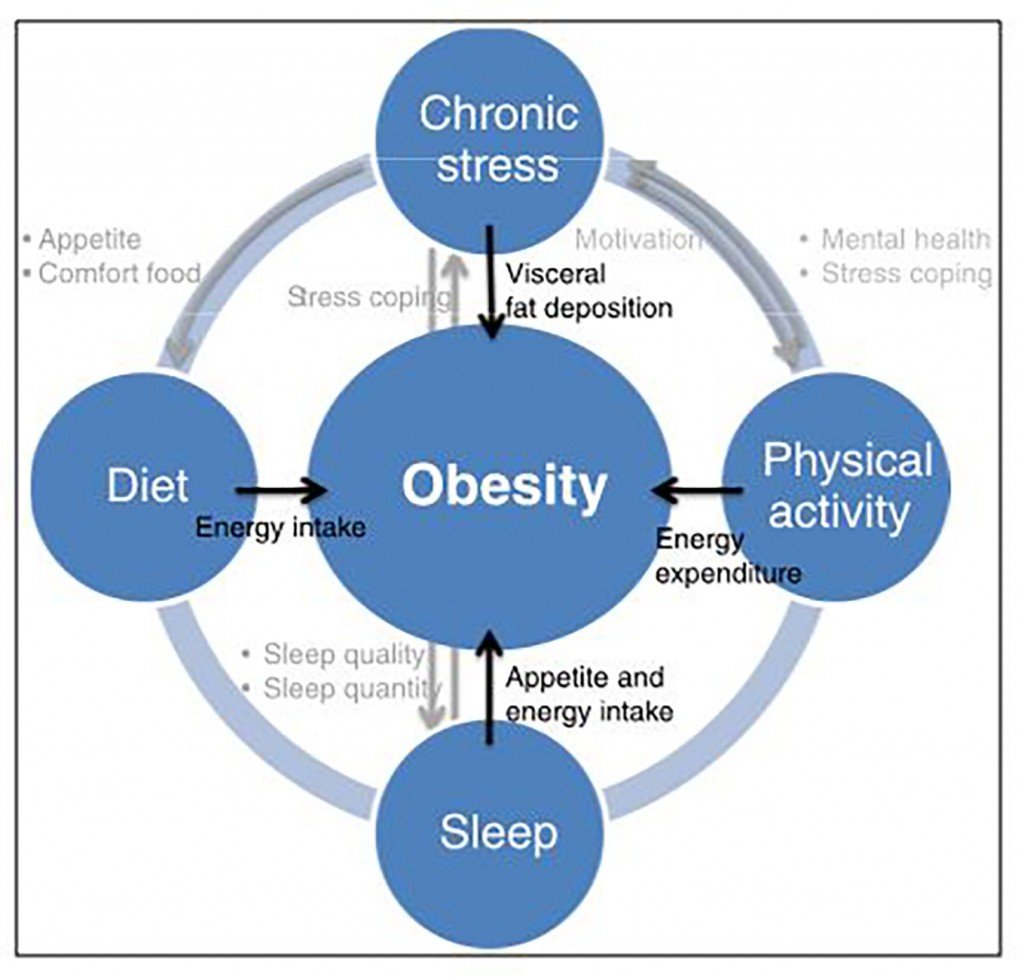
Figure 1. Neuroendocrine Contributions to Weight
Over the past dozen years, I have conducted clinical research, some of it NIH-funded, in health promotion and health behavior change. I have also worked with thousands of patients struggling with obesity and stress. My colleagues at our integrative medicinal practice, Pacific Pearl La Jolla, have also been involved in lifestyle change research (eg, the Ornish Program). As we designed the lifestyle change program for our new center, we drew upon both our scientific knowledge and patient experience to design an evidence-based program that also acknowledges the unique needs of each individual. Here, we share our program and what makes it so successful for people struggling to make significant, lasting lifestyle changes.
Why Stress Makes Us Fat
Numerous studies demonstrate a relationship between stress and choices or preferences for snack-type foods and foods high in fat and sugar.1,2 Women and unrestrained eaters consume more calories and fat under stress3 and alter their food choice from meal-type foods toward snack foods.4 “Emotional eaters” have elevated cortisol responses to stress, as well as increased intake of sweet and fatty snacks during stress.5 The mechanisms underlying these choices, linking cortisol to food choice, have not been fully elucidated, although neuroscience research implicates brain reward circuitry: adrenal glucocorticoids can enhance dopamine release, which reinforces the rewarding or motivational qualities of a rewarding food.6 Thus, decreasing stress emotionality and teaching people to separate emotionality/reward from food consumption are key strategies to restore balanced neuroendocrine feedback.
Mindfulness, Mood, and Biomarkers of Stress
Contemporary definitions of mindfulness emphasize bringing conscious, non-judgmental attention to one’s inner and outer experience in the present moment. Cultivating mindfulness is thought to promote clear thinking and open-heartedness. In the Buddhist tradition, mindfulness, or satipatthana, is one of the tenets of the Noble Eightfold Path leading to enlightenment.
A number of studies have documented the efficacy of different types of meditation training, including mindfulness and Mindfulness-Based Stress Reduction (MBSR)7 and transcendental and compassion-based practices, to decrease physiologic stress. In a 2011 study of overweight and obese individuals, mindfulness training improved cortisol secretion and reduced abdominal fat, more so among the obese.8 Thus, mindfulness may be acting in part by normalizing HPA-axis function, which can be observed though improvements in ACTH and cortisol.
In addition to the physiologic benefits of mindfulness on obesogenic stress, disordered cortisol/HPA axis functioning is also strongly associated with depression. A number of studies have found that short-term mindfulness training decreases depression, anxiety, and negative affect, and increases life satisfaction, vitality, optimism, sense of competence, and overall quality of life.9 Enhancement of emotional and mental attributes by mindfulness training improves weight loss success because improved mood is directly associated with increased chances of making good health choices, such as being physically active and eating healthfully.10 In fact, study participants report that feeling better because of [non-weight-targeted] treatments from CAM practitioners improved mood and well-being, thereby enabling them to tackle lifestyle behaviors changes.11 In this way, mindfulness training may help accelerate and maintain more consistent and self-motivated health behavior change.
Applying this science to our 12-week lifestyle transformation program, we include experiential training in several types of mindfulness, as well as group support to process deeper facets of mood and emotionality. We measure both biomarkers of stress (hair cortisol, diurnal cortisol rhythm, and endothelial dysfunction) and patient-reported metrics of mood, self acceptance, and mindfulness (the validated 10-item Perceived Stress Scale,12 PHQ-8 depression survey,13 Five Facets of Mindfulness,14 and Self-Compassion scale).15
How We Eat Matters Most
My previous research has shown that the conditions under which one eats may be more important than what one eats. There is a high prevalence of disordered eating among overweight/obese people.16 Poorest scores were found in the domains of Emotional Eating and Food Fretting. In our 2011 study, we evaluated a nutrition program containing both nutrition education and behavioral awareness education, to explore correlations between patterns of eating behavior, dietary composition, and biomarkers of cardiometabolic disease. We found that high scores in “Emotional Eating” correlated most strongly with higher baseline HbA1c values (p=0.04). At the end of the trial, HbA1c improvement was not significantly correlated with specific dietary factors such as percent of dietary carbohydrate or caloric intake. Rather, improvements in emotional eating patterns predicted improvements in HbA1c (p=0.046).17 Those that made the biggest changes in their eating behaviors had the largest changes in biomarkers of cardiometabolic disease, independent of calories or carbohydrate intake!
What to Eat
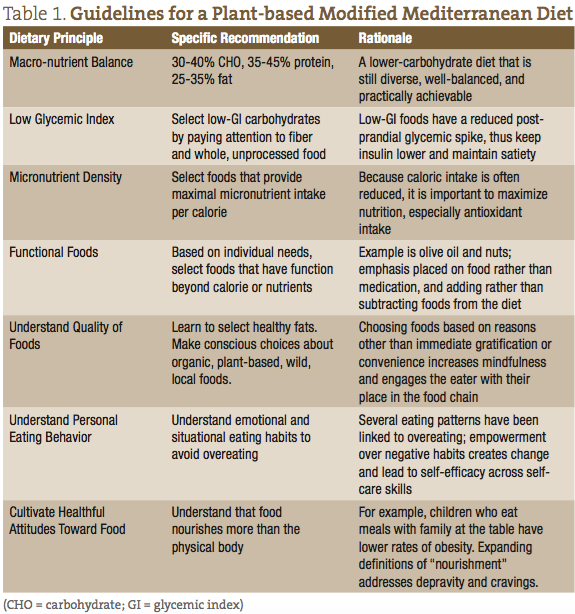
While importance of how we eat and the psychoneuroendocrine disruptions in dietary intake and preferences-related stress should be clear by now, people still need to know what to eat. We follow a plant-based modified Mediterranean pattern diet as a “best-practice” intervention, based on the accumulation of favorable epidemiology, clinical trials, and evidence of its palatability as a long-term option for healthful eating. The protective effects of this dietary pattern have been ascribed to specific components, such as increased fiber, poly- and mono-unsaturated fatty acids (MUFAs), dietary antioxidants, and polyphenols. Epidemiologically, following a Mediterranean diet is associated with lower rates of cardiometabolic disease and is inversely associated with body weight.18 Clinical trials support use of a Mediterranean diet for weight loss and reduced adiposity, as well as for primary and secondary prevention of cardiometabolic disease.19,20 More recently (2013), the Spanish PrediMed trial randomly assigned more than 7000 individuals to 2 versions of a Mediterranean diet (with additional unsaturated fats and polyphenols in the form of olive oil or mixed nuts) or to a low-fat diet.21 After 4.8 years, the trial was terminated because the Mediterranean diet groups had significantly fewer cardiovascular events. Compared to the low-fat diet, the multivariable-adjusted hazard ratios were 0.70 (95% confidence interval [CI], 0.54 to 0.92) and 0.72 (95% CI, 0.54 to 0.96) for the 2 versions of the Mediterranean diet, respectively.21
Compared to other dietary patterns, the Mediterranean diet is considered superior for the long term because it is more palatable. In the PrediMed trial, adherence to a Mediterranean diet was superior to a low-fat diet, and dropout rates were lower (4.9%) compared to the control group (11.3%). Similarly, 7-year outcomes from Toobert et al’s Mediterranean Lifestyle Program demonstrated durable adherence to a Mediterranean diet, both in terms of macronutrient intake and dietary behaviors.22
Using the principles outlined in Table 1, we teach and personalize a plant-based Mediterranean diet to meet individual goals such as additional caloric restriction, further reduction in glycemic load, or avoidance of food sensitivities. Our program includes cooking demonstrations, nutrition education, personalized meal plans, and modeling of healthy eating with bimonthly vegetarian dinners hosted at our center. We measure and track dietary adherence and eating behavior using the 14-question MEDAS Mediterranean Diet score, which was used to assess adherence in the PrediMed trial and the Seven Eating Styles eating behavior questionnaire.16,23
Using Physical Activity to Address Obesogenic Stress
The physical and metabolic effects of physical activity on weight and health are obvious and well documented, but the impact of physical activity on obesity goes beyond increasing caloric expenditure. Less obvious, but predicted to contribute to the success of multi-dimensional interventions, are the effects of physical activity on mood and motivation. Both basic and clinical studies document the efficacy of regular exercise to improve mood and cognition in studies with animals and a wide range of human subjects, including youth, adults, the obese, and a geriatric population with pharmacotherapy-resistant depression.24 There are multiple likely CNS mechanisms that mediate the mood effects of physical activity (endogenous opioids, serotonin, and dopaminergic systems).25 The hippocampus is a brain region that plays a critical role not only in cognition, but also in mood and depression.26 Elevated stress causes detrimental adrenal glucocorticoid effects on hippocampal function and anatomy; suppression of the generation of new synapses in the hippocampus is associated with both depression and obesity, conditions in which hippocampal atrophy has been documented.27 Physical activity independently increases hippocampal neurogenesis and volume in circumstances of both stress and non-stress, and can counteract the influence of a high-fat diet.28
When dietary interventions include caloric restriction, as they invariably do when addressing obesity, basal metabolic rate is suppressed, creating a disadvantage in long-term metabolism and weight loss. Researchers have compared caloric restriction of 25% compared to caloric restriction of 12.5% plus increased caloric expenditure of 12.5% (for an equal energy deficit). When physical activity is included, basal metabolic rate is maintained, thereby conferring a metabolic advantage that extends beyond the activity session.29
While any physical activity has beneficial effects on psychoneuroendocrine parameters, we emphasize feasible, stepped, individualized goal-setting and motivational interviewing to identify strategies to incorporate types of activity that are enjoyable.30 Our program includes a “sampler” of physical activities in which we emphasize finding activities that are enjoyable. We take our participants to the beach to walk and hike, offer yoga, and invite in-community instructors who lead activities ranging from dance to hula hooping. We encourage participants to track their own activity using personal accelerometers (build into most smart phones or FitBit-type devices). They upload their weekly reports via our electronic health records (EHR) patient portal, enabling us to measure pre/post changes.
Pulling It All Together
The effects on mood and motivation will be rooted to some extent in changes in CNS synaptic plasticity. For synaptic changes to be maintained, the cause (stimulus) of these changes must be embedded with frequent reinforcement of the new behaviors, as well as new understanding of old behaviors. Our lifestyle change program includes an hour-long weekly group support session facilitated by one of our doctors. In these groups, patients share their successes and struggles with health-related behaviors and support one another in transition. An independent relationship has been demonstrated between social support group attendance and improved health behaviors that is measurable beyond the effects of specific lifestyle habits.31 Neuroplasticity posits that the brain continually adjusts and reorganizes. As neural pathways become inactive or disused, they can atrophy or be repurposed to carry out functions lost to degeneration. Contrary to popular belief, adult brains can form new neural pathways.32
Integrative lifestyle change, which must often target obesity for maximal risk reduction and salugenesis, is best approached with multi-factorial, intensive, individualized treatment programs. When such programs are rooted in addressing the psychoneuroendocrine dysfunctions associated with stress, they are poised for success. Our best-practices program continues to undergo outcomes evaluation through formal IRB-approved research. Because of this research orientation, we are able to recruit patients who might not otherwise afford such a program; interim data-analysis also guides protocol refinement to ensure optimal patient outcomes. Additionally, it enables dissemination through publication. I suspect there are other integrative lifestyle change programs operated through integrative medicine clinics that are helping patients achieve positive outcomes. If you are involved with one and interested in participating in a practice-based research network, I invite your inquiry. New research studies are actively being planned.
 Erica Oberg, ND, MPH, a 2003 Bastyr graduate, practices with Guarneri Integrative Health at Pacific Pearl La Jolla, CA. Her clinical expertise is in nutrition and metabolism, and her patient population is preponderantly geriatric, with cardiometabolic disease, and struggling with lifestyle behaviors. Dr Oberg has published over 35 peer-reviewed papers summarizing her research. At Pacific Pearl, she directs the cooking and nutrition curriculum of the lifestyle change program and is lead investigator of the clinical outcomes research described here. When not in clinic, you will find her promoting her own health as a beginning surfer, playing with her dog, Siddha, on the beach, and cooking vegetables in delicious ways. Learn more at: www.drericaoberg.com and www.pacificpearllajolla.com.
Erica Oberg, ND, MPH, a 2003 Bastyr graduate, practices with Guarneri Integrative Health at Pacific Pearl La Jolla, CA. Her clinical expertise is in nutrition and metabolism, and her patient population is preponderantly geriatric, with cardiometabolic disease, and struggling with lifestyle behaviors. Dr Oberg has published over 35 peer-reviewed papers summarizing her research. At Pacific Pearl, she directs the cooking and nutrition curriculum of the lifestyle change program and is lead investigator of the clinical outcomes research described here. When not in clinic, you will find her promoting her own health as a beginning surfer, playing with her dog, Siddha, on the beach, and cooking vegetables in delicious ways. Learn more at: www.drericaoberg.com and www.pacificpearllajolla.com.
References
Adam TC, Epel ES. Stress, eating and the reward system. Physiol Behav. 2007;91(4):449-458.
Epel E, Lapidus R, McEwen B, Brownell K. Stress may add bite to appetite in women: a laboratory study of stress-induced cortisol and eating behavior. Psychoneuroendocrinology. 2001;26(1):37-49
Wardle J, Steptoe A, Oliver G, Lipsey Z. Stress, dietary restraint and food intake. J Psychosom Res. 2000;48(2):195-202.
Oliver G, Wardle J. Perceived effects of stress on food choice. Physiol Behav. 1999;66(3):511-515.
Newman E, O’Connor DB, Conner M. Daily hassles and eating behavior: the role of cortisol reactivity status. Psychoneuroendocrinology. 2007;32(2):125-132.
Lattemann DF. Motivation to Eat: Neural Control and Modulation. In: Harris RB, Mattes R, eds. Appetite and Food Intake: Behavioral and Physiological Considerations. . Boca Raton, FL: CRC Press; 2008: 81-94.
Matousek RH, Pruessner JC, Dobkin PL. Changes in the cortisol awakening response (CAR) following participation in mindfulness-based stress reduction in women who completed treatment for breast cancer. Complement Ther Clin Pract. 2011;17(2):65-70.
Daubenmier J, Kristeller J, Hecht FM, et al. Mindfulness intervention for stress eating to reduce cortisol and abdominal fat among overweight and obese women: an exploratory randomized controlled study. J Obes. 2011;2011:651936.
Daubenmier JJ, Weidner G, Sumner MD, et al. The contribution of changes in diet, exercise, and stress management to changes in coronary risk in women and men in the multisite cardiac lifestyle intervention program. Ann Behav Med. 2007;33(1):57-68.
Palomo T, Beninger RJ, Kostrzewa RM, Archer T. Affective status in relation to impulsive, motor and motivational symptoms: personality, development, and physical exercise. Neurotox Res. 2008;14(2-3):151-168.
Karlik JB, Ladas EJ, Ndao DH, et al. Associations between healthy lifestyle behaviors and complementary and alternative medicine use: integrated wellness. J Natl Cancer Inst Monogr. 2014;2014(50):323-329.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385-396.
Kroenke K, Strine TW, Spitzer RL, et al. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009;114(1-3):163-173.
Veehof MM, Ten Klooster PM, Taal E, et al. Psychometric properties of the Dutch Five Facet Mindfulness Questionnaire (FFMQ) in patients with fibromyalgia. Clin Rheumatol. 2011;30(8):1045-1054.
Costa J, Marôco J, Pinto-Gouveia J, et al. Validation of the Psychometric Properties of the Self-Compassion Scale. Testing the Factorial Validity and Factorial Invariance of the Measure among Borderline Personality Disorder, Anxiety Disorder, Eating Disorder and General Populations. Clin Psychol Psychother. 2015 Aug 20. [Epub ahead of print]
Scherwitz L, Kesten D. Seven eating styles linked to overeating, overweight, and obesity. Explore (NY). 2005;1(5):342-359.
Oberg EB, Bradley RB, Allen J, McCrory MA. Evaluation of a naturopathic nutrition program for type 2 diabetes. Complement Ther Clin Pract. 2011;17(3):157-161.
Dilis V, Katsoulis M, Lagiou P, et al. Mediterranean diet and CHD: the Greek European Prospective Investigation into Cancer and Nutrition cohort. Br J Nutr. 2012;108(4):699-709.
de Lorgeril M, Salen P, Martin JL, et al. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: final report of the Lyon Diet Heart Study. Circulation. 1999;99(6):779-785.
Schroder H. Protective mechanisms of the Mediterranean diet in obesity and type 2 diabetes. J Nutr Biochem. 2007;18(3):149-160.
Estruch R, Ros E, Salas-Salvado J, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013;368(14):1279-1290.
Toobert DJ, Strycker LA, Barrera M, Glasgow RE. Seven-year follow-up of a multiple-health-behavior diabetes intervention. Am J Health Behav. 2010;34(6):680-694.
Martinez-Gonzalez MA, Garcia-Arellano A, Toledo E, et al. A 14-item Mediterranean diet assessment tool and obesity indexes among high-risk subjects: the PREDIMED trial. PLoS One. 2012;7(8):e43134.
Dinas PC, Koutedakis Y, Flouris AD. Effects of exercise and physical activity on depression. Irish J Med Sci. 2011;180: 319-325.
Olsen CM. Natural rewards, neuroplasticity, and non-drug addictions. Neuropharmacology. 2011;61(7):1109-1122.
Fabricatore AN, Wadden TA, Higginbotham AJ, et al. Intentional weight loss and changes in symptoms of depression: a systematic review and meta-analysis. Int J Obesity (Lond). 2011;35(11):1363-1376.
Fotuhi M, Do D, Jack C. Modifiable factors that alter the size of the hippocampus with ageing. Nat Rev Neurol. 2012;8(4):189-202.
Mechanick JI, Apovian CM. Stressing over obesity. Curr Opin Endocrinol Diabetes Obes. 2009;16(5):339
Larson-Meyer DE, Redman L, Heilbronn LK, et al. Caloric restriction with or without exercise: the fitness versus fatness debate. Med Sci Sports Exerc. 2010;42(1):152-159.
Oberg EB. Research Review: Physical Activity Prescription: Our Best Medicine. IMCJ. 2007;6(5):18-22.
Schulz U, Pischke CR, Weidner G, et al. Social support group attendance is related to blood pressure, health behaviours, and quality of life in the Multicenter Lifestyle Demonstration Project. Psychol Health Med. 2008;13(4):423-437.
Liou S. Neurobiology. June 26, 2010. Huntington’s Outreach Project for Education, at Stanford Web site. http://web.stanford.edu/group/hopes/cgi-bin/hopes_test/neuroplasticity/. Accessed October 1, 2015.