Mona Morstein, ND
With the epidemic of diabetes at full swing in America right now, it’s a good time for naturopathic physicians to update themselves on the different types of diabetes. In particular, it’s pertinent for NDs to learn about a common type of diabetes that has not been heard of by most physicians, including most MDs.
Latent Auto-Immune Diabetes of the Adult (LADA) is not well known. LADA is an auto-immune process against the beta cells of the pancreas, but the destruction of the organ occurs very slowly, not quickly as in classic Type I. As a result, patients with LADA can be treated without insulin for years, and when it begins to be needed, doses are very low compared to injecting either Type I or Type II patients.
Diagnosing LADA
LADA patients are often misdiagnosed as Type II patients, as onset typically occurs during the mid-30s to -40s age range and insulin is rarely needed initially. In fact, recent studies show that 15%-20% of Type II patients are actually LADA patients. Thus, because many doctors are unaware of LADA, Type II is the only other option for diagnosis, though LADA patients are invariably lean, which makes a Type II diagnosis suspicious at best. They do not have insulin resistance. The LADA patients I’ve seen were women and diagnosed originally with Type II, even though none of them had any truncal obesity or signs of insulin resistance. Their ages at diagnosis ranged from 37 to 45 years.
There is no family history of diabetes Type I or II in LADA patients. LADA patients will be diagnosed through elevated blood sugar levels, both fasting and post-prandially. They do not present with ketoacidosis as a Type I patient does; their blood sugar numbers are not that high. Unlike Type I patients, they do not have to be hospitalized right away to stabilize their condition.
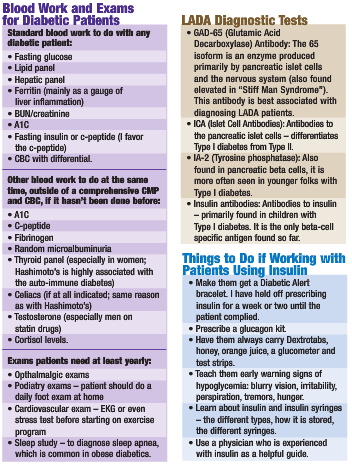
However, like typical Type I patients, the rest of their blood work is usually unremarkable; lipid panels and hepatic panels are normal. The diagnostic test for LADA is a positive GAD-65 antibody, although if one wishes, one can test the ICA (islet cell antibodies), IA-2 (Tyrosine phosphatase) or insulin antibodies, as well (see the accompanying story, “LADA Diagnotic Tests,” for more information). However, GAD-65 alone is standard for diagnosis.
Diagnostic clarity: If the GAD-65 antibody is elevated in a lean diabetic patient, with no signs of metabolic syndrome and whose hyperglycemia is uncontrolled with oral hyperglycemia agents, who has no family history of Type II and who has evidence of other auto-immune conditions in the family history, then LADA is the correct diagnosis. Out of the five LADA patients I saw, I was the only doctor who did the GAD-65 test. Also, some MDs use LADA and Type 1.5 interchangeably. The terms are not yet wholly defined; however, I don’t see any reason not to interchange them.
Since LADA is a formal type of diabetes, the same blood work needs to be performed on them as with any other type of diabetic (see the accompanying Blood Work and Exams for Diabetics sidebar).
It seems that full destruction of LADA patients’ pancreas will occur over time; however, I strongly believe that naturopathic medicine can slow that process. By keeping patients’ blood sugars as close to non-diabetic ranges as possible, and by supporting their bodies with exercise, stress relaxation, nutrients and herbs, the damaging effects of the disease can be greatly reduced. These same treatments will also slow or prevent the other devastating consequences of uncontrolled diabetes: cardiovascular disease, high blood pressure, blindness, kidney failure, neuropathy, amputations, NASH and dental problems.
Treatment for LADA
The treatment goals for a LADA patient are twofold: 1) keep medical indices in the standard medical treatment range; and 2) slow further destruction of the pancreas.
Medical indices treatment goals:
- BP: <130/80 mm/Hg
- TGs: <150 mg/dl
- LDL: <100
- A1C: <6.0
- Total chol: <200/180/175 (depending on whose guide you use).
Treatment of a LADA patient is very similar to treatment for other diabetic patients. They need a low-carb diet, as the very existence of diabetes means they have lost the metabolic capacity to regulate their usage of carbohydrates. I use a modified Bernstein diet with patients, which is very effective. In this type of diet, carbohydrates are greatly restricted; although unlike Bernstein, I do not have patients count every leaf of lettuce. Fats are not counted at all, but healthy ones are taught. Protein is a variable, with the grams/ounces of intake per day depending on activity level, need for weight loss or gain, and the experience of feeling gorged or hungry between meals. I advocate three meals a day and no snacking for my diabetic patients, especially for those on insulin.
Upon diagnosis, LADA patients may or may not do well on OHA. Testing the c-peptide is helpful. If it is low, then insulin is necessary; if not, OHA can be tried. The only OHA to use with LADA patients is Biguanide Glucophage, which works by decreasing glucose hepatic output. Thiazolidinendines (TZDs) are not indicated, as they work by decreasing insulin resistance. Studies have shown that the insulin secretagogues, the Sulphonylureas and Metiglinides are contra-indicated, as they quicken pancreatic burnout in LADA patients. The Alpha-glucosidase inhibitors, which prevent intestinal carbohydrate breakdown, are generally not prescribed, because most patients would rather have diabetes than relentless bloating and flatulence.
LADA and Insulin
At some point, LADA patients will need to be put on insulin. Prescribing this helpful drug means committing to close follow-up with patients and knowing how to deal with hypoglycemic reactions.
The type of insulin to start with for a LADA patient is Lantus or Detemir, one of the very long-acting insulins. However, be careful with dosing. The standard starting dose of Lantus for a Type II patient is 10 units at night; considering that LADA patients are usually diagnosed as Type II, this is a real problem. That much Lantus could cause a severe hypoglycemica reaction in a LADA patient.
My LADA patients are typically getting 1-2 units of Lantus p.m. or p.m./a.m. Although Lantus is considered a no-peak, 24-hour insulin, recent studies suggest that for many people it doesn’t last 24 hours and may even last only 11 hours. So, one must be able to analyze blood sugars and see if two doses of Lantus are needed; generally, seeing blood sugars rise in the afternoon and evening, even without dietary indiscretions, means that the bedtime Lantus is wearing off and a morning dose would be helpful for this patient. Raise insulin with LADA patients by only 0.5-1 units each time.
Upon diagnosis, LADA patients do not tend to need mealtime insulin dosing. Eventually, they may; but the progression to that need will definitely be slowed by following naturopathic protocols. Monitoring their c-peptide and glucograf will enable you to probably know when mealtime insulin is needed. The indication is continual pronounced elevated post-prandial glucose readings when they are on long-acting insulin and eating properly.
Having a patient fill out a weekly diet diary and chart of his or her blood sugars is necessary. I see patients weekly until I feel confident the protocol is working well in all ways – the diet is correct, supplements are well handled, blood sugars are under control, exercise is progressing, usage of insulin is good, and the patient feels he or she has things well understood. This generally takes three weekly visits, if enough time is given for Docere to occur.
The blood sugar journal differs based on the type of diabetic you are working with. For LADA patients not on insulin, taking their readings fasting and 1-1/2 hours after meals will suffice. When long-acting insulin is added, I suggest adding in a bedtime glucose reading. When mealtime dosing is also needed, check blood sugars fasting, after breakfast, before/after lunch, before/after supper and at bedtime until the patient is stable, and then the patient can test sugars fasting, after meals and at bedtime.
Of course, any time you change the bedtime insulin dose, I strongly suggest you have the patient wake up around 2 a.m. and test his or her middle-of-the-night glucose, to ensure there’s no overdose. Conservative use of insulin should mitigate this type of event.
Appropriate Herbals and Nutrients
Nutrients and herbs shown to protect the pancreas from diabetic damage include:
- NAC: 1200mg/day
- Taurine: 1500mg/day
- Green tea (extract): 100-300mg/day
- Gymnema sylvestre: 400mg/day
- Eucalyptus: I think only Jarrow’s Glucose Optimizer contains Eucalyptus
- General antioxidants: because much diabetic damage is oxidative damage
- Anti-glycosation nutrients: L-carnosine, vitamin E, ALA, Taurine.
I put all of my patients on a good multiple vitamin, fish oils and R-Alpha Lipoic Acid, as well as mixtures of the above. Other general diabetic supplements to know and use include: high-dose chromium, vanadium, bilberry/blueberry extract, Benfotiamine, Korean pine nut extract, cinnamon, chlorogenic acid from coffeeberry, ginseng, holy basil and bitter melon. Of course, exercise and stress reduction needs to be included in the protocol.
In my experience, working with LADA patients has been very rewarding. With help, the complications of diabetes can be much less likely to occur and the patient’s quality of life can be good.
Mona Morstein graduated from NCNM in 1988, and completed a one-year family residency there. Moving to Great Falls, Montana, Morstein practiced medicine in her own clinic for 13 years, during which time she had a cable access TV show and was a regular writer in the Great Falls Tribune on natural medicine. She joined SCNM as associate professor in 2002 and is now chair of nutrition and clinical supervisor, as well. Morstein sees patients of all ages, both sexes and all conditions, but particularly enjoys working with pre-diabetic and diabetic patients, GI conditions and women’s health. She is an avid hiker, a serious bibliophile, has written a book on Sherlock Holmes, and is a huge fan of the old TV show, “The Avengers.”
Case Study
A 47-year-old WF PTC with diagnosis of DM2 and fibromyalgia. She was diagnosed with Type II 12 years ago, which was controlled with diet and exercise. About three years ago, she began Actos and Metformin. A1C was around 6.3, but had risen to 7.9 recently. Her primary care physician had added Glyburide when the patient came to see me.
She was a very petite lady and always had been. She had daily diarrhea for years, no doubt due to the Metformin, as one-third of patients on that drug has that type of GI complaint. She also had chronic yeast infections; yeast overgrowth is common in diabetics. Her fibromyalgia was “body-wide.”
I put her on my modified Bernstein diet; multivitamin without iron; quality fish oils; a proprietary formula consisting of GYMNEMA SYLVESTRE 750 MG, ascorbic acid 250 MG, ALANINE 250 MG, GLUTAMINE 100 MG, ZINC (l-monomethionine) 30 MG; chromium polynicotinate 200 MCG; vanadyl sulfate 1.5mg; ALA alpha lipoic acid 300mg bid; and a magnesium bis-glycinate, taurine and malic acid combination. I had her begin exercising and stopped the Glyburide.
Within 10 days, her blood sugar journal was improving, so I stopped her Metformin. I ran a diabetic antibody test, which came back positive. Also, her c-peptide was <0.5ng/ml, indicating she needed to be put on insulin. Her diarrhea ceased with the cessation of Metformin, and I had her take a month of high-potency probiotics to ensure her gut was healthy again after such a long drug irritation.
I re-diagnosed her with LADA and began Lantus – 2 units p.m. and a.m. – and had her also stop the Actos. After another week, with her fasting glucose still being around 125, I raised the evening Lantus to 3 units. The patient suffered hypoglycemia the next morning, which was managed by taking 8 ounces of orange juice hourly until around noon, when her sugars stabilized. I decreased her evening Lantus dose to 2.5 units. This is a classic illustration of how one needs to go slowly with LADA insulin dosing!
Ten weeks after her first visit, she was off all OHA, was on the naturopathic protocol and supplements, had no more yeast infections, had significantly improved fibromyalgia; and all her blood sugars, fasting and post-prandial, were between 80 (fasting) and 110 (post-prandial); A1C 5.3.
I didn’t see her for one year and then called to follow up. She had gone to an endocrinologist three months before, who added humalog (mealtime insulin) and told her to eat more carbohydrates. She felt awful on this protocol and suffered terrible bouts of hypoglycemia, when she then had to eat a lot of food and went into really high hyperglycemia. Her fibromyalgia, which had not been a problem at all, came back badly.
She had gone back on my protocol one month before my follow-up, except she was only taking 2 units of Lantus in the a.m. Her blood sugars had stabilized at 90-100 all day long, fasting or post-prandial. She felt great! She has not needed an appointment, as her diabetes is stable and A1C in the low 5.0s on this protocol.
This case shows that not only did naturopathic medicine control her disease, it improved the functioning of her pancreas. She needed less Lantus one year after seeing me to control her sugars. And, as she was my first LADA patient, I had not yet incorporated the NAC, Taurine and/or a strong antioxidant formula.
Dr.Morstein received her B.S. summa cum laude in Foods and Nutrition from Arizona State University; she graduated from and did a residency at National College of Naturopathic Medicine. For 13 years, she had a successful private practice in Great Falls, MT. In 2002, Dr. Morstein joined SCNM and is Chair of Nutrition, Gastroenterology Professor and Clinical Supervisor. Known as an expert on diabetes, she teaches a two day “Insulin Intensive Seminar” which has been consistently highly praised, and lectures regularly throughout North America. Dr. Morstein is also a recipient of the AANP’s 2012 “The President’s Award” for service to the profession.


