Student Scholarship Honorable Mention
Terri Bugg, ND
Patricia J. Rennie, ND
Morphea, also known as localized scleroderma, is a rare disease with an incidence rate of 3 in 100 000 and a prevalence rate of 50 per 100 000.1 The disease affects women 2.6 times more than men, and can appear in all races, though appears to be more common, up to 73-82%, among Caucasians.2 The average age of onset for morphea is typically between 20 and 40 years of age and depends on the type of morphea involved. Approximately 50-65% of those affected are adults.3 The etiology of morphea is unknown4; however, the condition has been associated with trauma, vascular abnormalities, autoimmune processes, viruses, and infections.5 Morphea is a chronic inflammatory skin disease, which manifests as a disorder of cellular immunity, microcirculation, and an abnormal increase in collagen synthesis.6 Excessive collagen deposition causes sclerosis and fibrosis of the skin, which contributes to stiffness, movement disorders, and limited mobility.
Current first-line treatments with the most evidence for efficacy in morphea include phototherapy, methotrexate, systemic corticosteroids, calcipotriene, and topical tacrolimus.7 However, there is no consensus on the treatment of morphea, and most of the studies are case series, with very few comparative or placebo-controlled clinical trials.8 Management of morphea remains unsatisfactory or inconsistent, as some patients receive systemic immunosuppressives, while others receive little to no therapy. Methotrexate, either alone or with corticosteroids, has the greatest level of evidence.7 However, recurrence rates following discontinuation of treatment are high, ranging from 30-40%.5 Long-term use of corticosteroids is associated with increased risks of cardiovascular disease, osteoporosis, increased infections, and suppressed adrenal gland function. Chronic use of methotrexate can result in liver damage and side effects including nausea and vomiting, mouth ulcers, and anemia. Treating scleroderma in earlier stages is generally more successful at reducing inflammatory activity compared to treating sclerosis featuring chronic, well-established lesions.9
Case Presentation
This case report is of a 68-year-old female, Chilean senior citizen who initially presented with chief complaints of morphea. Based on skin biopsy, the patient was conventionally diagnosed with morphea. Her medical doctor prescribed methotrexate and corticosteroids, which she refused in favor of alternative therapies. The onset of the skin condition was 4 months prior to seeking natural treatment. Two years before the onset of the condition, the patient cited several major stressful life events that continued to affect her, including a sudden loss of employment and the death of her pet cat. The patient was single and lived alone, and she described her pet as an important and primary emotional support for her. She experienced intense shock, grief, and sadness at the death. She had been unable to express the grief fully and was still in the grieving process. She admitted that the loss of her pet triggered a deep fear of being alone, fear of the aging process, and fear of the transition process into retirement.
The patient does not have a genetic predisposition to morphea or other skin disorders per family history or previous medical history. She also has no prior history or family history of physical trauma, radiation exposure, major infection, or autoimmune conditions. She has a good social support system with friends and is conscientious about her health, incorporating a healthy diet and regular light exercise. She lives an active lifestyle, spending her time visiting friends in social gatherings, doing errands, or traveling.
The patient’s main presenting symptoms were indurated, dry, and discolored skin, distributed over the ankles and dorsal feet bilaterally. At the time of initial presentation she rated her condition as 8/10, (10=worst). The affected skin was not pruritic or painful, but was associated with intense discomfort, stiffness, and sensation of tightness, as if the skin were about to break. On examination, the epidermis of the feet and ankles bilaterally was dry, hyperkeratotic, indurated, flaking, cracking, and stiff, with approximately 40% discoloration in the affected areas, which ranged from white, light yellow, pink, and light purple (Figure 1). Skin discoloration was most prominent when the feet were in flexed position or when the patient was supine. Epidermis at the dorsal and lateral ankle areas was sclerotic, smooth, and shiny, with decreased mobility. The right foot was slightly less affected than the left foot, and the toes were spared bilaterally. She had dry skin on her face and upper and lower extremities, and spider veins were observed on the lateral sides of the right and left-upper thighs. All other physical findings were within normal limits. In the mental and emotional sphere, the patient suffered from chronic grief, anxiety related to her health, insomnia, and intense restlessness. She had persistent restlessness in the feet, with desire for constant movement and a sense of internal unease. Movement greatly improved her symptoms, as it ameliorated both her physical discomfort and emotional restlessness. The patient found both the morphea and insomnia distressing and having a negative impact on her quality of life.
Figure 1. Before Treatment
 Treatment
Treatment
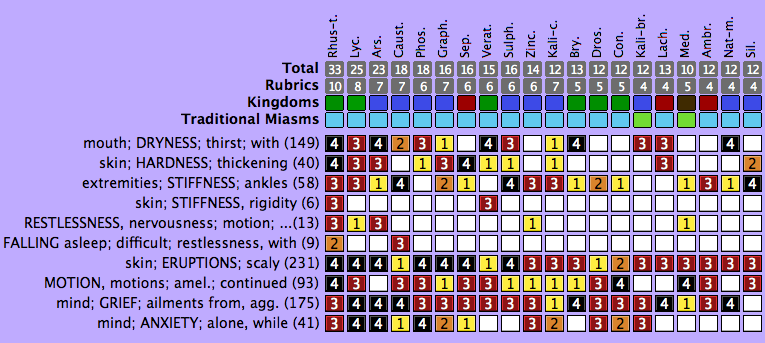
The primary intervention was an individualized constitutional homeopathic medicine. The single homeopathic remedy, Rhus radicans, was prescribed as a 200C potency. The patient received a total of 3 dry doses of 2 pellets per dose over a period of 6 months, with approximately 6-7 weeks between doses (Table 1). Selection of the appropriate homeopathic medicine was based on the guiding totality of symptoms that characteristically represented the entirety of the case, including mental, physical, and general symptoms. As you know, homeopathic materia medica was developed through clinical signs and symptoms both in patient provings and patients treated with homeopathy. Materia medica and repertorization were used to select appropriate rubrics for skin qualities (stiffness, induration, discoloration) as well as key mental and emotional features (grief, restlessness, sleeplessness) (Figure 2). The repertory software program MacRepertory (Edition 8.5.2.9) was used to match rubrics to an extensive collection of historical repertory databases. Rubrics were analyzed under the Expert Analysis setting.
Table 1. Frequency & Dosing of Remedy
| Date | Treatment | Dose |
| September 19, 2016 | Rhus radicans 200C | 2 dry pellets once |
| November 14, 2016 | Rhus radicans 200C | 2 dry pellets once |
| February 6, 2017 | Rhus radicans 200C | 2 dry pellets once |
Figure 2. Repertorization
Rhus tox vs Rhus radicans
Analysis of the rubrics scored Rhus toxicodendron, also known as the Atlantic poison oak (Toxicodendron pubescens), as the top remedy. A review of homeopathic materia medica and provings indicated clinical use of both Rhus tox and Rhus radicans in dermatological conditions characterized by rash, stiffness, induration, yellow or white discoloration, and anxiety with restlessness.10 Rhus radicans, also known as the Eastern poison ivy (Toxicodendron radicans), is symptomatically a close relative of the well-known homeopathic remedy Rhus toxicodendron. Rhus radicans is a poisonous Asian and North American flowering plant that causes intense pruritus, erythema, and dermatitis on contact.
The clinical use of homeopathic Rhus radicans is quite similar to Rhus tox, the main distinction being that Rhus radicans is often used in more severe presentations of a condition and when Rhus tox fails to act.10 Rhus radicans was chosen as a first remedy due to the severe presentation of this patient’s condition. Keynotes for the remedy are joint or skin stiffness accompanied by anxiety and restlessness that are ameliorated by motion – symptoms which the patient in this case study strongly exhibited.
Outcome & Data
As mentioned, the patient was treated with a single, individualized constitutional homeopathic remedy, with multiple, repeat single doses over a period of 6 months. During this time, both the morphea and insomnia continuously improved. Skin on the feet and ankles bilaterally displayed decreased sclerosis, cracking, dryness, and discoloration. In comparison to before treatment, skin in the area exhibited increased suppleness and mobility at the end of treatment (Figure 3).
Figure 3. After Treatment
 Patient outcome was evaluated both subjectively (through a 0-10 numerical analogue scale based on self-identified symptoms of concern) and objectively (through validated clinical assessment outcomes based on localized scleroderma skin activity and skin damage). After the first homeopathic dose and reassessment after 3 weeks, energy and insomnia had improved, with no difficulty falling asleep on any days. The morphea had also improved, with a decrease in dryness. However, a sensation of tightness and restriction on movement remained. After the second homeopathic dose, the patient had a return of old symptoms, including whole-body itching for approximately 2 months and a temporary worsening of existing symptoms for 1 week.
Patient outcome was evaluated both subjectively (through a 0-10 numerical analogue scale based on self-identified symptoms of concern) and objectively (through validated clinical assessment outcomes based on localized scleroderma skin activity and skin damage). After the first homeopathic dose and reassessment after 3 weeks, energy and insomnia had improved, with no difficulty falling asleep on any days. The morphea had also improved, with a decrease in dryness. However, a sensation of tightness and restriction on movement remained. After the second homeopathic dose, the patient had a return of old symptoms, including whole-body itching for approximately 2 months and a temporary worsening of existing symptoms for 1 week.
At the end of treatment the patient subjectively rated the morphea as 3/10 (10=worst), compared to 8/10 at the onset of treatment. The patient rated the insomnia as 2/10 at end of treatment, compared to 8/10 at initial presentation. Subjective assessment demonstrates a 63% improvement in morphea and 75% improvement in insomnia. At the end of treatment the patient reported decreased anxiety about her health, a greater sense of overall well-being, decreased grief and internal restlessness, and a discontinuation of restless sensation in the lower extremities. Energy levels had increased and were consistent, with only an occasional drop in energy in the afternoons.
To objectively evaluate localized scleroderma, computerized skin scores (CSS), MRI, skin biopsy and ultrasound can be used. However, these methods often require specialized equipment or training, are not available at the teaching clinic, and are invasive or often expensive, so were not utilized. Several clinical assessment methods have been published, such as the Modified Rodnan Skin Score (MRSS), the Localized Scleroderma Skin Severity Index (LoSSI), and the Localized Scleroderma Assessment Tool (LoSCAT).11,12 These methods assess activity and damage based on limited clinical parameters.
The LoSCAT has recently been validated to assess scleroderma,12,13 is the most widely reported outcome measure for morphea, and has been recommended for future treatment studies.13,14 The LoSCAT consists of the modified LoSSI (mLoSSI), the Localized Scleroderma Damage Index (LoSDI), and the Physician Global Assessment of Disease Damage (PGA-D). The LoSCAT was selected in this case to objectively evaluate the patient’s condition before and after treatment (Table 2 and Figure 4). The LoSSI score decreased from 12 to 4, and the LoSDI decreased from 8 to 4. Objective assessment demonstrates a 67% improvement in skin activity and 50% improvement in scleroderma skin damage after 6 months of treatment.
Table 2. LoSCAT Results: Data
| Date | LoSSI
(Total Score, out of 100) |
LoSDI
(Total Score, out of 100) |
| September 19, 2016 | 12 | 8 |
| February 13, 2017 | 6 | 6 |
| March 6, 2017 | 4 | 4 |
(LoSCAT = Localized Scleroderma Cutaneous Assessment Tool; LoSSI = Localized Scleroderma Skin Activity Index; LoSDI = Localized Scleroderma Skin Damage Index)
Figure 4. LoSCAT Results: Graph
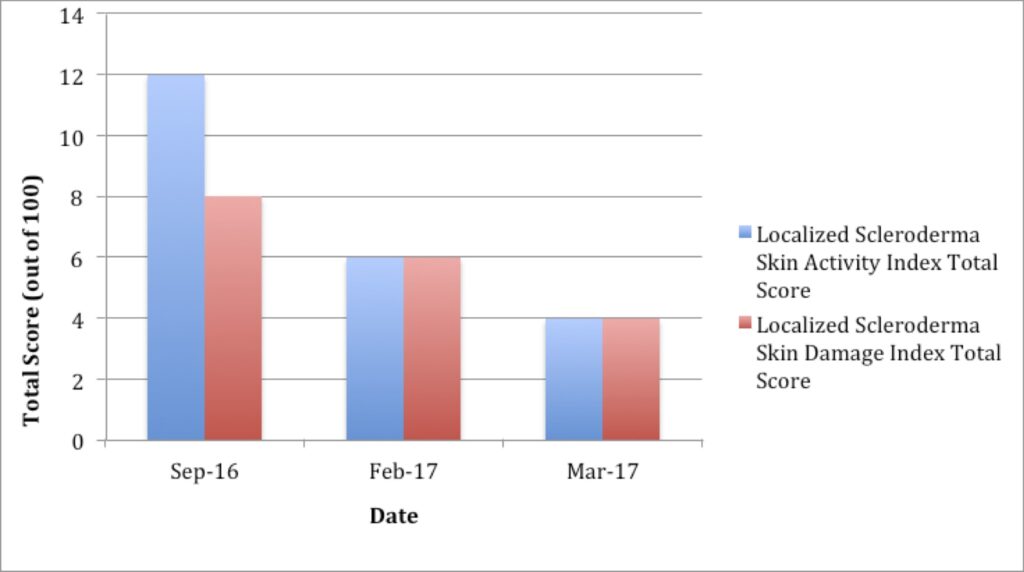
(LoSCAT = Localized Scleroderma Cutaneous Assessment Tool)
Discussion
Conventional treatment and management of morphea is challenging and unsatisfactory, and backed by very few comparative or placebo-controlled trials.5 A variety of therapeutic strategies have been proposed and used clinically; however, no consensus currently exists regarding treatment strategies for morphea. Lack of agreement on how to accurately capture disease outcomes in localized scleroderma has also hindered the development of efficacious treatment protocols.5 Similarly, there is a lack of controlled therapeutic studies examining treatment of morphea with homeopathy. However, homeopathy offers an alternative approach with a higher safety profile and fewer adverse effects,15-17 as demonstrated in this case.
A cross-sectional descriptive survey study assessed the use of complementary and alternative medicine (CAM), including homeopathy, in pediatric rheumatological cases, including several with scleroderma.18 A high prevalence of CAM use in pediatric rheumatology patients attending a tertiary-care ambulatory clinic was found, although actual results from its use were not evaluated. To date, no peer-reviewed medical literature or clinical trials exist on the treatment of scleroderma-related conditions with homeopathy. The lack of literature is possibly due to the rare incidence of scleroderma and, in particular, morphea. Although no peer-reviewed literature exists for this condition, homeopathic materia medica is extensive and derived from clinical cases collected over the past 200 years and systematic provings indicating the symptoms best treated by a particular remedy.
After several months of constitutional homeopathic treatment, the patient’s physical symptoms – and, most importantly, the mental and emotional symptoms such as energy and mood – all markedly improved. Homeopathic medicines work on the totality of the patient, including the mental, emotional, and physical aspects. Consistent administration of the homeopathic medicine via scheduled repetition of doses was the main variable held constant throughout treatment. Improvements were noted after each successive dose of homeopathic medicine, supporting the notion that Rhus radicans is an effective primary intervention.
An indication of the correct remedy selection was the long action of single doses as well as the slight aggravation at beginning of treatment that was followed by overall improvement. According to Hahnemann, the closer a remedy is to the simillimum, the more reaction may be expected15; the exact simillimum may cause a slight aggravation before relief comes.15 Deep therapeutic action was demonstrated by the return of old symptoms (ROS), which occurred after the second dose. Earlier in the year, prior to the manifestation of morphea, the patient experienced intense whole-body itching for several months on the back, shoulders, and extremities. The itching spontaneously resolved, followed by the appearance of morphea. The resolution of 1 symptom that is immediately followed by another, more severe symptom, represented a shift in disease state from a milder condition to a deeper pathological state.
An ROS occurs during homeopathic treatment when unresolved disease states and previous suppressions reappear before being removed, and is a sign of a correct remedy selection.19 According to both Hering’s Direction of Cure and Hahnemann, an ROS is a clinically observed symptom or symptoms that can indicate a deep-seated healing and healing crisis in a patient.19,20 The reversing of the order of symptoms is the basis of the direction of cure, because it inherently includes the return of old, unresolved states as well as the movement from within to without, from the most important to the less important, and from above to below when the disease clearly developed this way.19 This process also includes a beneficial change in the mental state, an increased sense of well-being, and increased vitality – all of which this patient experienced. After the second dose, in spite of a temporary slight worsening of symptoms, the patient had an internal sense of well-being. The temporary worsening of symptoms may be classified as a homeopathic aggravation15 and can be interpreted as an indication of a positive healing process.
Limitations in the case include a lack of reassessment by biopsy as well as the possibility of spontaneous resolution. To confirm improvement in morphea, morphological skin changes should be evaluated through follow-up biopsy testing and correlated to clinical outcomes in scleroderma skin damage and activity, as described earlier. The potential exists that observed changes in the patient’s condition might be superficial in nature and not representative of a true regression of the disease. The natural history of morphea shows that spontaneous regression can occur within 3 to 5 years, with the average time of spontaneous remission, or skin softening, occurring at 2.7 years.1 However, the available evidence does not show resolution before 3 years. The patient in this case experienced improvement within 6 months of treatment, which most likely indicates that results were due to the therapy undertaken and not a result of spontaneous remission.
Conclusion
This case report demonstrates the effectiveness of a well-selected homeopathic remedy, as a primary intervention in morphea, to support healing of dermatological conditions. The homeopathic medicine Rhus radicans was clinically shown to improve morphea, a rare skin condition that is historically difficult to treat.
Homeopathy was founded in the 18th century by the German physician, Samuel Hahnemann. Homeopathy is based on the principle of “like cures like,” or the Law of Similars, where highly diluted small doses of a substance can heal a health condition that would produce similar symptoms to that same condition when given in larger doses. As a complementary and alternative medicine, homeopathy is a whole-systems approach to healthcare that is prescribed based on the patient’s entire pattern of symptoms, including the physical, emotional, mental, and spiritual factors of disease, to treat root causes and provide highly individualized treatment. Since homeopathic medicines have a high safety profile, low risk of side effects, and are cost-effective, they constitute a viable alternative to conventional treatment in morphea.
References:
- Peterson LS, Nelson AM, Su WP, et al. The epidemiology of morphea (localized scleroderma) in Olmsted County 1960-1993. J Rheumatol. 1997;24(1):73-80.
- Fett N, Werth VP. Update on morphea: part 1. Epidemiology, clinical presentation, and pathogenesis. J Am Acad Dermatol. 2011;64(2):217-228.
- Leiteneberger JJ, Cayce RL, Haley RW, et al. Distinct autoimmune syndromes in morphea: a review of 245 adult and pediatric cases. Arch Dermatol. 2009;145(5):545-550.
- Fitzpatrick TB. Dermatology in General Medicine: Textbook and Atlas, Volume 2. New York, NY: McGraw-Hill Companies; 1987: 1841-1852.
- Careta MF, Romiti R. Localized scleroderma: clinical spectrum and therapeutic update. An Bras Dermatol. 2015;90(1):62-73.
- Valančiene G, Jasaitiené D, Valiukevičiene S. Pathogenesis and treatment modalities of localized scleroderma. Medicina (Kaunas). 2010;46(10):649-656.
- Zwischenberger BA, Jacobe HT. A systematic review of morphea treatments and therapeutic algorithm. J Am Acad Dermatol. 2011;65(5):925-941.
- Vilela FA, Carneiro S, Ramos-e-Silva M. Treatment of morphea or localized scleroderma: review of the literature. J Drugs Dermatol. 2010;9(10):123-129.
- Kreuter A, Krieg T, Worm M, et al. German guidelines for the diagnosis and therapy of localized scleroderma. J Dtsch Dermatol Ges. 2016;14(2):199-216.
- Vermuelen F. Concordant Materia Medica. Haarlem, Netherlands: Emryss Publishers; 2000.
- Arkachaisri T, Pino S. Localized scleroderma severity index and global assessments: a pilot study of outcome instruments. J Rheumatol. 2008;35(4):650-657.
- Kelsey CE, Torok KS. The Localized Scleroderma Cutaneous Assessment Tool: responsiveness to change in a pediatric clinical population. J Am Acad Dermatol. 2013;69(2):214-220.
- Arkachaisri T, Vilaiyuk S, Torok K, Medsger T. Development and initial validation of the localised scleroderma skin damage index and physician global assessment of disease damage: a proof-of-concept study. Rheumatology. 2010;49(2):373-381.
- Mertens JS, Seyger MMB, Thurlings RM, et al. Morphea and eosinophilic fasciitis: an update. Am J Clin Dermatol. 2017;18(4):491-512.
- Hahnemann S. Organon of the Medical Art. Palo Alto, CA: Birdcage Press; 1996: 171-172, 196-205, 252-253.
- Brönhoft G, Wolf U, von Ammon K, et al. Effectiveness, safety and cost-effectiveness of homeopathy in general practice – summarized health technology assessment. Forsch Komplementmed. 2006;13 Suppl 2:19-29.
- Dantes F, Rampes H. Do homeopathic medicines provoke adverse effects? A systematic review. Br Homeopath J. 2000;89 Suppl 1:S35-S39.
- Hagen LE, Schneider R, Stephens D, et al. Use of complementary and alternative medicine by pediatric rheumatology patients. Arthritis Rheum. 2003;49(1):3-6.
- Hering C. Preface. In: Hahnemann SC. The Chronic Diseases. Translated by Hempel CJ. New York, NY: William Radde; 1845. Available at: http://www.simillimum.com/education/little-library/homoeopathic-philosophy/hpcd/article.php. Accessed June 20, 2018.
- Hahnemann SC. The Chronic Diseases. New Delhi, India: B Jain Publishers Pvt; 2005.
 Terri Bugg, ND, has a general family practice in Vancouver, British Columbia, with special clinical interests in mental health in adults and youth, autoimmune disease, and environmental medicine. Dr Bugg graduated from the Canadian College of Naturopathic Medicine (CCNM) in 2017; her other academic credentials were earned from the Ontario College of Homeopathic Medicine (DHMHS) and the University of Toronto (HBSc). She is originally from Yellowknife, Northwest Territories, and prior to naturopathic medicine she cultivated her love for nature working in biological research and the environmental field.
Terri Bugg, ND, has a general family practice in Vancouver, British Columbia, with special clinical interests in mental health in adults and youth, autoimmune disease, and environmental medicine. Dr Bugg graduated from the Canadian College of Naturopathic Medicine (CCNM) in 2017; her other academic credentials were earned from the Ontario College of Homeopathic Medicine (DHMHS) and the University of Toronto (HBSc). She is originally from Yellowknife, Northwest Territories, and prior to naturopathic medicine she cultivated her love for nature working in biological research and the environmental field.
 Patricia J. Rennie, ND, has been active in the field of naturopathic medicine in Ontario for over 25 years. Dr Rennie has a busy private practice in Thornhill, Ontario, and supervises interns at CCNM on a pediatric shift. She has served as academic faculty at CCNM, teaching anatomy labs and pediatrics, has served on the OAND Board, and was a founding member of Health Canada’s Pediatric Expert Advisory Council.
Patricia J. Rennie, ND, has been active in the field of naturopathic medicine in Ontario for over 25 years. Dr Rennie has a busy private practice in Thornhill, Ontario, and supervises interns at CCNM on a pediatric shift. She has served as academic faculty at CCNM, teaching anatomy labs and pediatrics, has served on the OAND Board, and was a founding member of Health Canada’s Pediatric Expert Advisory Council.