Risk Stratification of CVD: Making Use of an ECG Interpretation Guide
Docere
Nathaniel Bingham, ND
Electrocardiography (ECG), today, is an essential part of the initial evaluation for patients presenting with cardiac complaints. An ECG plays an important role as a non-invasive, cost-effective tool to evaluate arrhythmias and ischemic heart disease.1 As an important diagnostic tool, healthcare providers of all levels of training and expertise consistently recognize the need to have the ability to interpret ECGs; however, an increased rate of misinterpretation has occurred among non-specialized physicians and especially among medical students.2
Evolution of the ECG
Dr Willem Einthoven, a Dutch physiologist, developed the first ECG machine in 1901 and demonstrated the 5 deflections known today as the waveforms PQRST.3 The original device weighed 600 lb, and 3 electrodes were used to construct Einthoven’s triangle.4,5 In 1924, Einthoven was awarded the Nobel Prize in physiology and medicine for the invention of the ECG.5 Over the next 30 years, a central terminal was developed to establish the precordial leads and the augmented unipolar leads. In 1954, the American Heart Association’s 12-lead ECG, as we know it, was standardized.5,6
There is a multitude of clinical uses of the 12-lead ECG. For example, the ECG may reflect changes associated with coronary artery disease, hypertension, cardiomyopathy, infiltrative disorders, metabolic and electrolyte abnormalities, and therapeutic or toxic effects of drugs or medical devices.7 Each waveform of an ECG has its own sensitivity and specificity and is influenced uniquely by pathophysiologic factors. There are more structural/pathophysiologic changes than recognizable ECG patterns, which results in significant overlap and reduces the specificity of ECGs. For example, although ST-segment and T-wave changes are the most common and most sensitive ECG abnormalities, these changes are also the least specific.8
ECGs are interpreted by practitioners of cardiology, emergency medicine, internal medicine, and family medicine.9 If the interpretation of an ECG contributes to clinical decision-making, the physician should have a sufficient knowledge base to make an accurate diagnosis. A categorical list comprised of 88 abnormalities has been established by the American College of Cardiology /American Heart Association (ACC/AHA), to represent competency.10 An adequate knowledge base should include the ability to define, recognize, and understand the basic pathophysiology of certain electrocardiographic abnormalities. A competent ECG reader should understand the importance of comparing a current ECG tracing to previous tracings in order to make the correct diagnosis, and recognize that not all clinical disorders always produce a diagnostic ECG pattern.10
ECG Interpretation Guide for Primary Care
Dr Martin Milner, Professor of Cardiology at the National University of Natural Medicine, developed a 1-page ECG interpretation guide 25 years ago as a reference for reducing interpretation time and aiding in the education of medical students. The backbone of Dr Milner’s original interpretation guide consisted of topics including: rate, rhythm, axis, hypertrophy, ischemia, and infarct. This framework guides students through a standard 12-lead ECG and highlights basic-to-complex concepts in a method that results in an acceleration of content/pattern recognition and recall.
In 2013, Cory Szybala (an eager naturopathic medical student at the time) , and I (a 1st-year medical resident) attempted to update Dr Milner’s classic document. Dr Szybala was the lead graphic designer and essential to the development of the new ECG Interpretation Guide. Our goals were to 1) enhance the guide with an overview section; 2) create a graphic-enhanced, stepwise approach for students to learn specific aspects of ECG tracings; 3) include keynotes of specific ECG findings; 4) provide a review of the cardiac conduction pathway; and 5) create a means of locating ECG findings and associating them with specific coronary artery abnormalities. The new edition has been updated 11 times in the last 2 years and has been used by more than 400 medical students. During this process, the feedback from students was surveyed, cataloged, and reviewed before changes to the Interpretation Guide were completed (Figure 1).
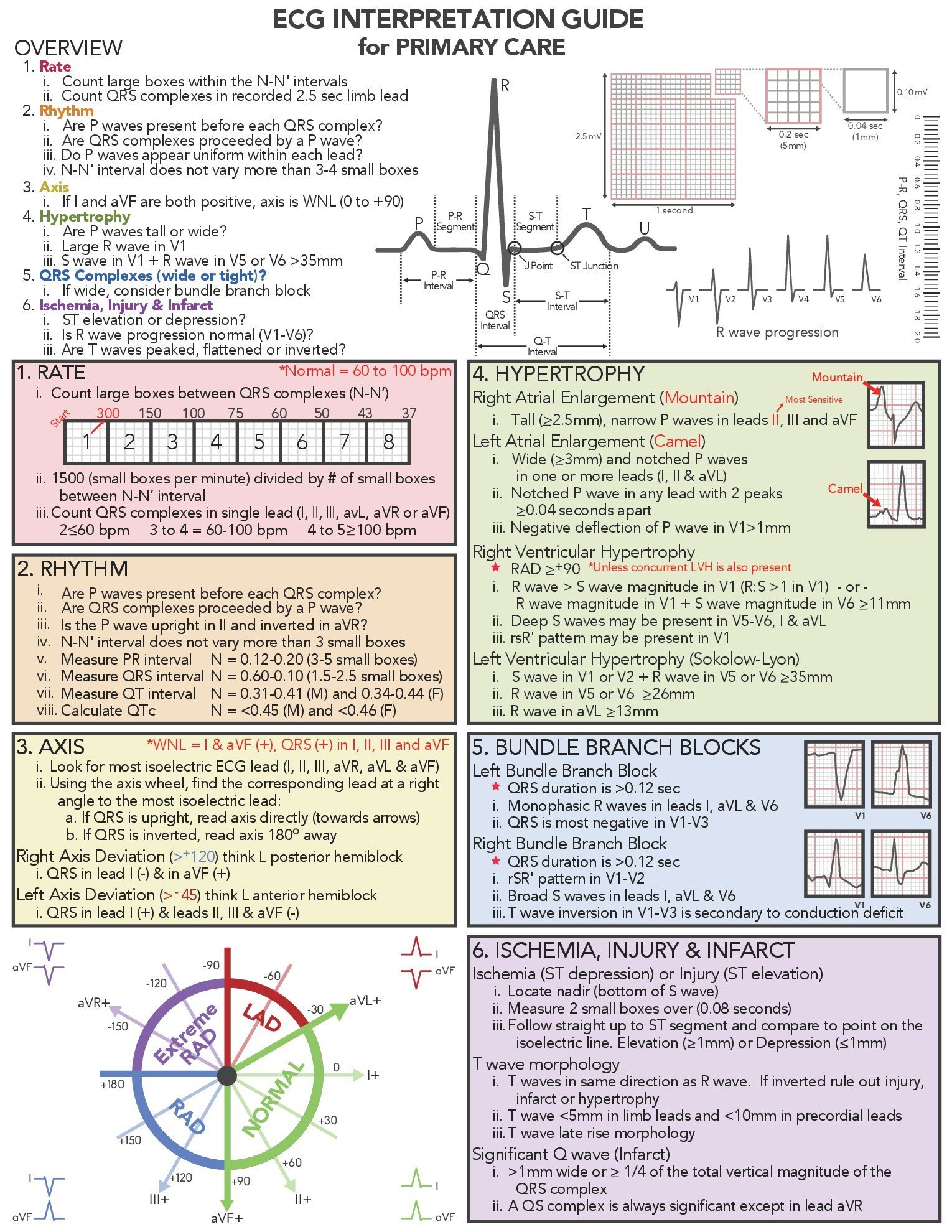
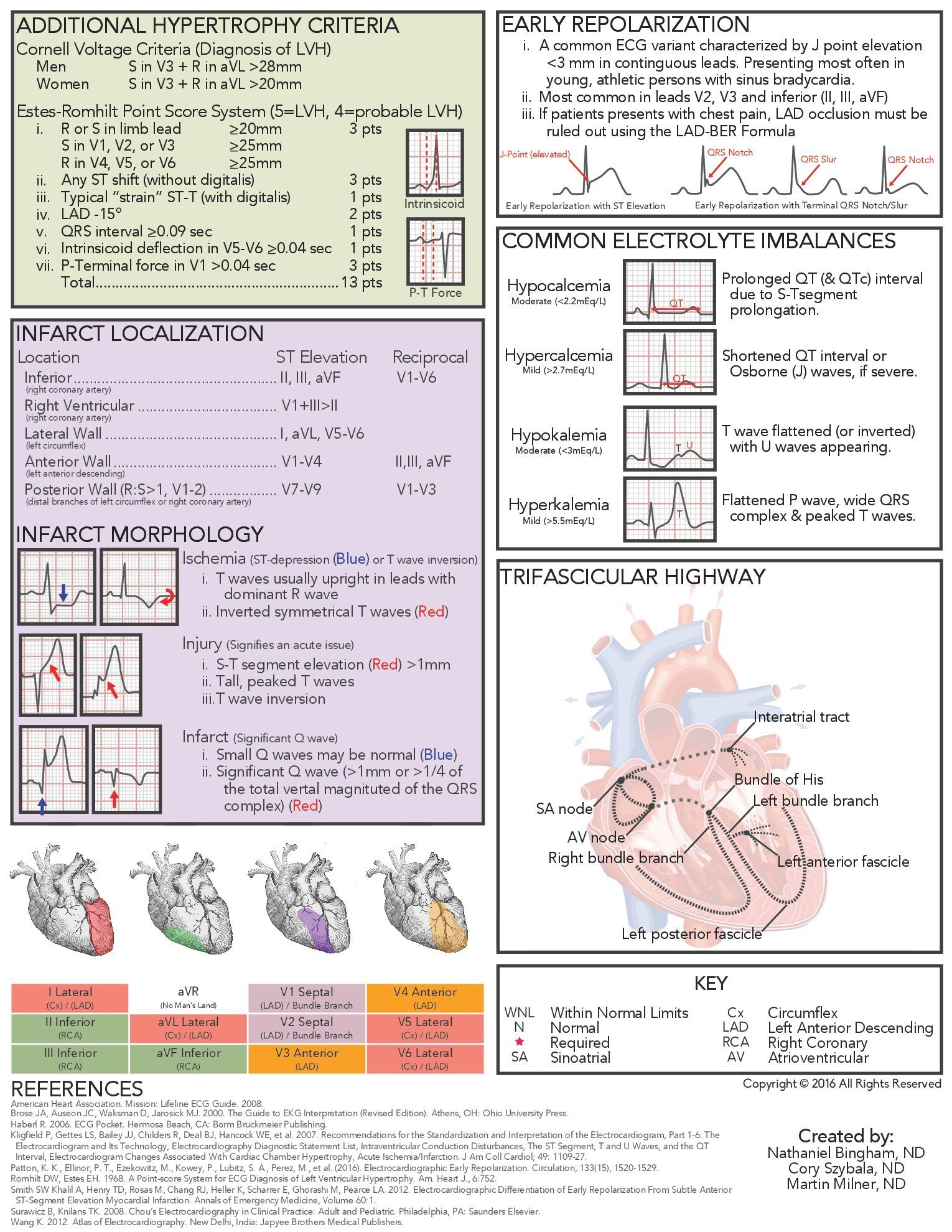
Figure 1. ECG Interpretation Guide
The indispensable reference source for ECGs – Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric, 6th edition – has 752 pages, which is obviously very difficult to summarize into a 2-page document. The ECG Interpretation Guide for Primary Care explains rhythm concepts; however, it never discusses premature atrial, junctional, or ventricular contractions, types of atrioventricular blocks, sinoatrial blocks, paroxysmal supraventricular tachycardias, Torsades de Pointes, or wide QRS complex tachycardias. Unique ECG findings, such as coved ST-segment elevation in Brugada syndrome; the SI QIII TIII pattern associated with a pulmonary embolism; or PR interval depression and the “Fireman’s hat sign” in pericarditis, are also not discussed due to a lack of space and a need for greater competency of the ECG reader.
Dr Milner has stated, “An electrocardiogram is not cardiology; it is primary care.” I believe this as well and have seen first-hand how ECGs can guide clinical decision-making, risk-stratify patients for or with cardiovascular disease, and facilitate the best patient care for our patients. As there is an increased interest in an integrative approach to medicine, which naturopathic physicians provide, we as a profession must strive to educate medical students, new doctors, and established doctors to strengthen our abilities to be primary care physicians. The ECG Interpretation Guide for Primary Care is an attempt to create a building block for our profession and will hopefully one day be a keystone to naturopathic cardiovascular medicine.
References:
- Fye WB. A history of the origin, evolution, and impact of electrocardiography. Am J Cardiol. 1994;73(13):937-949.
- Salerno SM, Alguire PC, Waxman HS, et al. Training and competency evaluation for interpretation of 12-lead electrocardiograms: Recommendations from the American College of Physicians. Ann Intern Med. 2003;138(9):747-750.
- Einthoven W. Ueber die Form des menschlichen electrocardiogramms. Pflügers Arch Eur J Physiol. 1895;60(3):101-123.
- Einthoven W, Fahr G, De Waart A. On the direction and manifest size of the variations of potential in the human heart and on the influence of the position of the heart on the form of the electrocardiogram. Am Heart J. 1950;40(2):163-211.
- AlGhatrif M, Lindsay J. A brief review: history to understand fundamentals of electrocardiography. J Community Hosp Intern Med Perspect. 2012 Apr 30;2(1).
- Wilson FN, Kossmann CE, Burch GE, et al. Recommendations for standardization of electrocardiographic and vectorcardiographic leads. Circulation. 1954;10(4):564-573.
- Fisch C. Evolution of the clinical electrocardiogram. J Am Coll Cardiol. 1989;14(5):1127-1138.
- Friedberg CK, Zager A. “Nonspecific” ST and T-wave changes. Circulation. 1961;23:655-661.
- Mason JW, Hancock EW, Saunders DE Jr, et al. American College of Cardiology report on ECGEXAM. J Am Coll Cardiol. 1997;29(2):466-468.
- Kadish, A, Buxton, A, Kennedy H, et al. ACC/AHA clinical competence statement on electrocardiography and ambulatory electrocardiography: A report of the ACC/AHA/ACP-ASIM task force on clinical competence (ACC/AHA Committee to develop a clinical competence statement on electrocardiography and ambulatory electrocardiography) endorsed by the International Society for Holter and noninvasive electrocardiology. Circulation. 2001;104(25):3169-3178.
 Nathaniel Bingham, ND, completed a joint 3-year residency as the Heart & Lung resident at the National University of Natural Medicine (NUNM) and at the Center for Natural Medicine (CNM). During his residency, he completed a 3-year external rotation in Cardiology, which included ECG and echocardiogram interpretation, direct current (DC) cardioversion, and the observation of pacemaker/loop monitor implantation and 37 coronary angiograms. Dr Bingham has been in private practice since 2015 and is currently an adjunct clinical faculty member at NUNM.
Nathaniel Bingham, ND, completed a joint 3-year residency as the Heart & Lung resident at the National University of Natural Medicine (NUNM) and at the Center for Natural Medicine (CNM). During his residency, he completed a 3-year external rotation in Cardiology, which included ECG and echocardiogram interpretation, direct current (DC) cardioversion, and the observation of pacemaker/loop monitor implantation and 37 coronary angiograms. Dr Bingham has been in private practice since 2015 and is currently an adjunct clinical faculty member at NUNM.