Fecal Microbiota Transplantation for Ulcerative Colitis
Mark Davis, ND
Fecal microbiota transplantation (FMT) is also known as human probiotic infusion, fecal transplant, fecal bacteriotherapy, fecal slurry, and gut flora rehabilitation and has been humorously referred to as “transpoosion.” The procedure consists of collecting stool from a healthy donor; suspending it in water, normal saline, or 4% milk; and administering it to the patient (most frequently via enema but also via colonoscope, nasogastric or nasoduodenal tube, rectal tube, or even [anecdotally] orally as a milkshake1). This massive infusion of healthy colonic bacteria has been used as far back as the 17th century in veterinary medicine to treat digestive disturbances2 and as early as 1958 in humans to treat pseudomembranous colitis.3
Fecal microbiota transplantation has a 90% success rate in curing Clostridium difficile–associated chronic diarrhea, colitis, and pseudomembranous colitis,4 which affect half a million and kill 15 000 to 20 000 Americans per year.5 Fecal microbiota transplantation has been used to treat patients with ulcerative colitis (UC), Crohn disease, and irritable bowel syndrome6; metabolic syndrome7; and chronic constipation (T. J. Borody, MD, PhD, personal communication, October 2011) and may have benefited patients with Parkinson disease8 and with multiple sclerosis.9 Adverse effects of administration via enema have been reported as none10 or as negligible,11 although abdominal discomfort may occur, as reported in the case study herein.
A randomized controlled trial of FMT to treat relapsing C difficile infection (CDI) has been conducted by a group of Dutch scientists and is awaiting publication (T. J. Borody, MD, PhD, personal communication, October 2011), and a trial examining FMT to treat inflammatory bowel disease is under way in Seattle, Washington (P. Schleinitz, MD, personal communication, October 2011). Gastroenterologists in the United States are only performing the procedure for the 20% of CDI that does not resolve with antibiotics. Dr Paul Schleinitz of the Rogue Valley Medical Center in Medford, Oregon, performs FMT to treat CDI for the cost of the colonoscopy he delivers them with (about $200) using donor stool from household members. He is waiting for conclusive research to demonstrate the efficacy of the technique in other areas but says that “we’re just touching the tip of the iceberg. In 10-20 years, we’ll understand a lot more about the benefits of the healthy human microbiome” (P. Schleinitz, MD, personal communication, October 2011).
FMT for UC
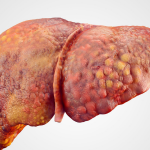
The cause of UC is unknown. However, it is associated with an altered intestinal microbiome and is hypothesized to result from an unbalanced relationship between the gut flora and the host’s immune system.5
Fecal microbiota transplantation is the only nonsurgical therapy for UC that has demonstrably induced persistent medication-free remission. Symptom-free remission, with no histological signs of inflammation, has been documented during follow-up as long as 13 years.10 Fecal microbiota transplantation pioneer Dr Thomas Borody of the Center for Digestive Diseases (CDD) near Sydney, Australia, defends the use of FMT even in the absence of published randomized controlled trials: “You only need one Martian to prove there is life on Mars” (T. J. Borody, MD, PhD, personal communication, October 2011). In 2004, Borody and colleagues6 authored the first literature review on bacteriotherapy. The CDD performs 100 to 200 FMT procedures annually, totaling more than 1650 procedures to date; about 5% of their FMTs are performed on patients with UC (T. J. Borody, MD, PhD, personal communication, October 2011).
Methods
The definitive article on the use of FMT to treat UC recommends the following protocol10: (1) antibiotics for the suppression of clostridia (vancomycin [500 mg twice daily], metronidazole [400 mg twice daily], and rifampicin [150 mg twice daily], all by mouth for 7-10 days), (2) followed by whole-bowel irrigation with 3 L of polyethylene glycol–based oral solution, and (3) using 200 to 300 g of donor stool (about 1 normal adult bowel movement [BM]) mixed with 200 to 300 mL (about 1 cup) of normal saline, administration as a daily retention enema for 5 consecutive days. The definitive article on the use of FMT to treat CDI11 further refines the methods as applicable to the treatment of UC, instructing that the donor stool should be strained for particulate matter and blended to a slurry within 24 hours (ideally within 6 hours) of the donor BM and administered within 10 minutes of preparation. The article also suggests the optional addition of a gentle osmotic laxative for the donor and loperamide hydrochloride for the recipient.
Current practice at the CDD includes an initial bolus of fecal slurry to be delivered via colonoscope and as many as 10 consecutive days of FMT by retention enema, retained for 2 to 8 hours, followed by weekly readministrations (by a gastroenterologist or as a home procedure) until a colonoscopic biopsy sample reveals normal histologic findings of unprepared biopsy. Using this protocol, Dr Borody reports a greater than 90% extended remission rate for patients with UC (T. J. Borody, MD, PhD, personal communication, October 2011).
Donor stool is tested for C difficile, Giardia, Cryptosporidium, Cyclospora, Isospora, and pathogenic enteric bacteria, ova, and parasites. Donor serologic testing includes human immunodeficiency virus, syphilis, and hepatitis A, B, and C.11 These donor screening tests cost between US $500 and $600 to run.
A thorough donor interview is necessary to identify transmissible risks that laboratory tests may not detect (owing to unavailability, lack of sensitivity or early stage, or window period timing). The ideal donor is a healthy individual with the following characteristics: (1) no communicable disease or risk factors, (2) no history of inflammatory bowel disease, irritable bowel syndrome, or gastrointestinal malignancy, (3) no antibiotic, major immunosuppressive, or systemic antineoplastic use in the past 3 months, (4) no autoimmune, atopic, or chronic pain disease or metabolic syndrome, and (5) no recent ingestion of any potential allergens.11
Patient Perspectives
Scouring the Internet for anecdotal data reveals a treasure trove of conversation on the HealingWell.com forum. In one particular thread spanning 2 years,12 28 individuals describe their experience undergoing FMT at the CDD as an outpatient under the supervision of a local gastroenterologist or at home without the use of donor screening, initial antibiotics, intestinal lavage, or medical supervision of any kind. Of 28 posters to the forum who tried FMT, 11 stated that they have UC and reported their results. Of those individuals, 5 had immediate, dramatic, and long-lasting improvement; 3 had some improvement; 1 had no improvement; and 2 reported that the FMT caused a flare. One of the success stories involved a single FMT self-administration using only a few tablespoons of a related infant donor’s stool, which resulted in almost immediate cessation of symptoms lasting 2 years until a course of antibiotics precipitated UC symptoms again. This highlights the fact that practitioners can suggest home treatment to individuals with UC and have patients use stool—an abundant natural substance—to potentially effect a previously unattainable cure at no financial cost. This may be the only option available to patients with limited financial resources and has been documented as successful treatment for refractory CDI.13 At the CDD, patients estimate paying more than US $20,000 to treat UC with FMT, including prescreened donor stool, antibiotic therapy, the procedure itself, lodging, and travel costs.14
Patients on health forums (and every patient to whom I have ever proposed the procedure) are inevitably confronted with “the yuk factor” of putting someone else’s fecal matter in their own body cavity. Some patients, despite their suffering, are dissuaded from trying FMT for that reason, although other patients who continue to be interested or go on to try the therapy cite their more displeasing UC symptoms as the reason for overcoming their initial revulsion. There are groups working on a system to extract the therapeutic bacteria from donor fecal matter to overcome this limitation (T. J. Borody, MD, PhD, personal communication, October 2011).
Naturopathic Medicine and FMT
This article is not the first on the topic of FMT by an ND. Jacob Schor15 has written on the subject in the Natural Medicine Journal, pointing out that polymerase chain reaction analysis of recipient colon flora before and after FMT reveals a persistent change to the donor enterotype after FMT. For NDs in regions where FMT is in the scope of practice, like Oregon,16 the procedure seems a natural fit. It is using the very life within us to restore balance to an unbalanced system, doing no harm by the use of a therapy with no known deleterious adverse effects. That being said, we would be remiss to neglect the tenet of tolle causum by treating a patient who has not undergone a comprehensive evaluation. For example, treating persistent rectal bleeding and pain with FMT without previous colonoscopic evaluation could overlook a colon cancer. As Dr Borody has said, “you have to treat the whole of the patient, not just the hole of the patient” (T. J. Borody, MD, PhD, personal communication, October 2011).
Case Study (Treated in Collaboration with Steven Sandberg-Lewis, ND)
LC is a 37-year-old woman who presented with a diagnosis of left-sided UC from the rectum to 35 cm. She was making 10 to 15 trips to the bathroom per day for unproductive rectal spasms, all her BMs were bloody, and she could eat few foods without aggravating her tenesmus and abdominal pain. Abdominal ultrasonography findings were normal, and small intestinal bacterial overgrowth test results were negative.
She was unable to control her symptoms with mesalamine, a specific carbohydrate diet, butyrate enemas, oral probiotics, low-dose naltrexone, medical food powders, or an intestinal health nutraceutical product containing mucilaginous herbs, plant enzymes, glutamine, butyric acid, and deglycyrrhizinated licorice. Hydrocortisone (100-mg rectal suppositories twice daily for 2 weeks) controlled her symptoms well, but her symptoms returned after the 2-week course.
We suggested a home FMT, and she tried a modified version. With no home preparation (antibiotics or lavage), she collected the fecal contents of her toddler’s diaper, blended with a cup of salt water, and took them as a retention enema for 4 of 5 consecutive days. She was only able to retain the sample for 2 to 3 hours (instead of the recommended 6-8 hours) owing to increased abdominal tenderness and the need to care for her children. She experienced no improvement during or following the 4 days of FMT, and if anything her condition was worse afterward.
LC came to see us again several months later, interested in trying FMT again. Her abdominal pain was limiting her activities of daily living, she was experiencing tenesmus as often as every 5 to 10 minutes, and she was only able to make our appointment by skipping breakfast. She reported spending half of each day in the bathroom or being immobilized by her abdominal pain. She had found an adult donor and arranged for child care during the series. Her vital signs were significant for a pulse rate of 108 beats/min, temperature of 99.5°F by mouth, and blood pressure of 90/70 mm Hg left arm, sitting.
We were concerned about her apparent hypovolemia and did not think she was likely to receive therapeutic benefit from the FMT with such uncontrolled spasms and frequency. So, we referred her to a local gastroenterologist for pharmaceutical management, calling to secure her a next-day appointment.
Her symptom picture and energy improved dramatically over the next week on a regimen of prednisone (20-30 mg daily), oral mesalamine, and a liquid multivitamin, at which point she initiated FMT for a second time. This time, she used a polyethylene glycol lavage and an adult donor and was able to remain horizontal and retain the enemas for 6 to 8 hours per day as we suggested. At her request, we had prescribed antibiotics per the protocol given in the “Methods” section, with the caveat that she must sign an informed consent form detailing the common minor and uncommon rare adverse effects of those antibiotics. She initially planned to fill the prescriptions, but after her pharmacist cautioned her about potential adverse effects as well, she decided to decline.
She experienced intense abdominal tenderness and chills while retaining the enemas, and she almost immediately had to have a BM if she had to stand or walk. She also menstruated at mid-cycle, a first for her. At her 1-month follow-up visit after the 5-day series, she reported “feeling much better,” with more-formed stools, minimal blood, and decreased tenesmus.
 Mark Davis, ND graduated with honors in research from National College of Natural Medicine, Portland, Oregon. He works at the Bright Medicine Clinic in Portland, focusing on naturopathic primary care, colon health, and environmental allergens. Bright Medicine Clinic will be offering inpatient fecal microbiota transplantation starting in January 2012, along with nutritional, botanical, physical, and pharmaceutical services and Traditional Chinese Medicine. He can be reached at [email protected].
Mark Davis, ND graduated with honors in research from National College of Natural Medicine, Portland, Oregon. He works at the Bright Medicine Clinic in Portland, focusing on naturopathic primary care, colon health, and environmental allergens. Bright Medicine Clinic will be offering inpatient fecal microbiota transplantation starting in January 2012, along with nutritional, botanical, physical, and pharmaceutical services and Traditional Chinese Medicine. He can be reached at [email protected].
References
1. Health Matters to Me. Fecal transplants: the turd twister & a historical account. August 8, 2011. http://www.ryan-koch.blogspot.com. Accessed October 2011.
2. Klein W, Müller R. Das einweibminimum, die zymogene symbiose und die erzeugung von mikrobeneiweib im pansen aus stickstoffverbindungen nicht eiweibartiger nature (ein beitrag zur biologie des widerkäuers). Z Tierz Züchtungsbiol. 1941;48:255-276.
3. Eiseman B, Silen W, Bascom GS, et al. Fecal enema as an adjunct in the treatment of pseudomembranous enterocolitis. Surgery. 1958;44:854-859.
4. Bakken JS. Fecal bacteriotherapy for recurrent Clostridium difficile infection. Anaerobe. 2009;15:285-289.
5. Khoruts A, Sadowsky MJ. Therapeutic transplantation of the distal gut microbiota. Mucosal Immunol. 2011;4(1):4-7.
6. Borody TJ, Warren EF, Leis SM, Surace R, Ashman O, Siarakas S. Bacteriotherapy using fecal flora: toying with human motions. J Clin Gastroenterol. 2004;38:475-483.
7. Vrieze A, Holleman F, Serlie MJ, et al. Metabolic effects of transplanting gut microbiota from lean donors to subjects with metabolic syndrome. Abstract presented at: European Association for the Study of Diabetes Annual Meeting 2010; September 22, 2010; Berlin, Germany. Abstract 90.
8. Ananthaswamy A. Faecal transplant eases symptoms of Parkinson’s. New Scientist. January 19, 2011.
9. Freakonomics.com. Freakonomics radio: the power of poop. March 4, 2011. http://freakonomicsradio.com/the-power-of-poop.html. Accessed October 2011.
10. Borody TJ, Warren EF, Leis S, Surace R, Ashman O. Treatment of ulcerative colitis using fecal bacteriotherapy. J Clin Gastroenterol. 2003;37(1):42-47.
11. Bakken JS, Borody T, Brandt LJ, et al; Fecal Microbiota Transplantation Workgroup. Treating Clostridium difficile infection with fecal microbiota transplantation [published online ahead of print August 24, 2011]. Clin Gastroenterol Hepatol. doi:10.1016/j.cgh.2011.08.014. Medline:21871249
12. HealingWell.com. Fecal transplant: I took the plunge! part I. http://www.healingwell.com/community/default.aspx?f=38&m=1612467. Accessed October 2011.
13. Silverman MS, Davis I, Pillai DR. Success of self-administered home fecal transplantation for chronic Clostridium difficile infection. Clin Gastroenterol Hepatol. 2010;8(5):471-473.
14. HealingWell.com. Fecal transplant via colonoscopy tmrw. http://www.healingwell.com/community/default.aspx?f=38&p=6&m=2135358. Accessed October 2011 (page 6, post by “jasherlynch” on 7/21/11).
15. Schor J. Fecal flora transplantation in the treatment of colonic and metabolic disease. Nat Med J. April 5, 2011. http://naturalmedicinejournal.com/article_content.asp?article=144. Accessed November 16, 2011.
16. Oregon Board of Naturopathic Medicine. Public board meeting. February 7, 2011. http://www.oregon.gov/OBNM/Minutes/2011/2.7.11.pdf. Accessed October 2011.