Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols (FODMAPs)
Christine Doherty, ND
Fructose was discovered in 1847 by French chemist Augustin-Pierre Dubrunfaut.1 It is the sweetest and most water-soluble of all the sugars. A naturally occurring plant monosaccharide, it has been implicated as a cause of the American obesity epidemic, elevated triglycerides, gout, nonalcoholic fatty liver disease, hypertension, cancer, and more. The focus of this article, however, is on fructose and its related carbohydrates effect on the digestive tract, specifically as an underdiagnosed cause of irritable bowel syndrome (IBS). The prevalence of IBS in Europe and North America according to the World Gastroenterology Organisation is estimated to be 10% to 15%.2 There is a serious genetic condition called hereditary fructose intolerance (HFI), which can cause severe hypoglycemia, vomiting, liver damage, and seizures. For both fructose intolerance and HFI, the treatment is a diet low in fructose and related molecules, specifically fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs). Technically, lactose intolerance falls under the FODMAP umbrella; therefore, patients with lactose intolerance may also have a further intolerance to other foods in this category. Like lactose intolerance, the laboratory test is a fructose challenge breath test.
Fructose Intolerance or Malabsorption
Fructose is absorbed directly from the intestines into the bloodstream. Individual tolerance for fructose varies widely; the standard American diet can be high enough in fructose to exceed the threshold for absorption even in those who do not have any compromise in their ability to absorb fructose. Free fructose has limited absorption in the small intestine, with up to one-half of the population unable to completely absorb a load of 25 g.3 The average daily intake of fructose varies from 11 to 54 g around the world.3 The term fructose intolerance is used interchangeably with fructose malabsorption. Fructose intolerance can cause damage to the villi of the small intestine, leading to nutrient malabsorption. If patients have been diagnosed as having another malabsorption condition such as celiac disease or small intestinal bacterial overgrowth, they often have a reduced threshold for FODMAPs, leading to refractory gastrointestinal symptoms. It is interesting to note that, unlike small intestinal bacterial overgrowth, fructose intolerance will not falsely raise tissue transglutaminase IgA in patients with celiac disease. Fructans are not hydrolyzed or absorbed in the small intestine. The physiological consequences of their malabsorption include increasing osmotic load, providing substrate for rapid bacterial fermentation, changing gastrointestinal motility, promoting mucosal biofilm, and altering the profile of bacteria.3
Hereditary Fructose Intolerance
Hereditary fructose intolerance becomes symptomatic when FODMAP foods are introduced to babies with this genetic predisposition. According to researchers at Boston University, Boston, Massachusetts, it is an autosomal recessive metabolic disease that is due to a deficiency of fructose-1-phosphate aldolase activity, which results in an accumulation of fructose-1-phosphate in the liver, kidney, and small intestine.4 The accumulated fructose-1-phosphate inhibits glycogen breakdown and glucose synthesis, thereby causing severe hypoglycemia following ingestion of fructose. Adults with milder cases can reach adulthood without being diagnosed.
Laboratory test results that can be abnormal in patients with HFI include the following:
- Elevated liver function tests
- Elevated uric acid
- Reactive hypoglycemia after fructose and sucrose dose
- Low magnesium
- Low phosphate
Symptoms of HFI include the following:
- Excessive sleepiness
- Hypoglycemia
- Convulsions
- Vomiting
- Irritability
- Jaundice
- Poor feeding as a baby
- Problems after eating fruits and fructose-containing or sucrose-containing foods
- Failure to thrive
- Renal damage
Hereditary fructose intolerance may remain undiagnosed until adult life and may lead to death following fructose or sorbitol infusion.5 Boston University offers the HFI gene test, although it is not considered diagnostic; the only truly diagnostic test is a liver biopsy and assay for aldolase B. Consider referring patients to a geneticist for diagnosis.
Fructose Challenge Breath Test
Fructose challenge breath tests are available in home kits. The patient has to follow a low-fiber diet the day before the test, and then after a 12-hour fast he or she consumes a fructose load and provides 3 hourly breath samples in test tubes. A positive test result shows an elevation of hydrogen over baseline.6 This test is not currently available from many laboratories commonly used by NDs. The turnaround time for the laboratory I use is approximately 2 to 4 days. The laboratory does not provide free kits to clinicians, so I recommend drop shipping them directly to patients. Some gastroenterologists now perform an in-office fructose challenge breath test, generating instant results. I generally recommend a FODMAP elimination or challenge diet as my diagnostic tool because this will not exacerbate patients’ symptoms, but taking a challenge dose of fructose may. For patients with undiagnosed HFI, a fructose challenge breath test can be dangerous, triggering life-threatening symptoms.7
FODMAP Diet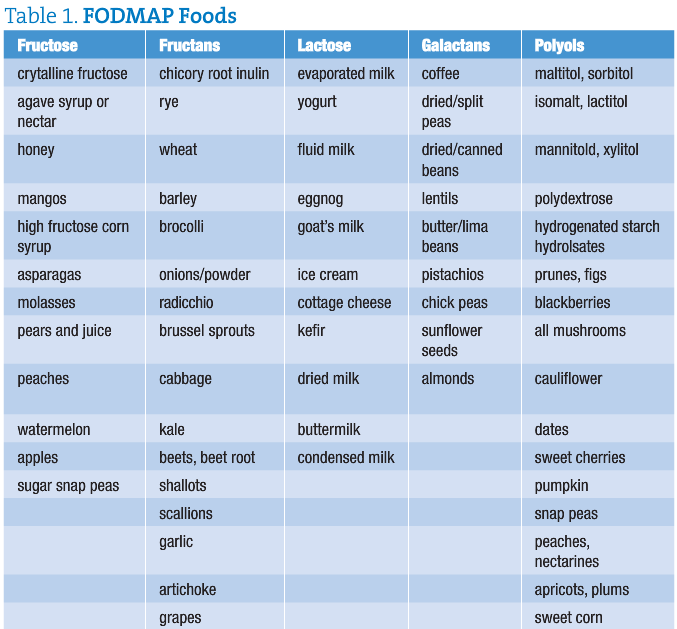
In 1999, Australian researcher Dr Sue Shepherd developed the low-FODMAP diet.8 She has celiac disease and recognized that many patients with celiac disease continued to experience IBS symptoms even when they were compliant with their gluten-free diet. She developed the diet as her PhD research. In 2006, she was awarded the Gastroenterological Society of Australia’s Young Investigator of the Year Award for discovering the connection between FODMAPs and IBS (the same award was given for the discovery of Helicobacter pylori). The FODMAP diet has been shown to improve IBS in 74% of patients.9
FODMAP Diet Implementation and Challenge
I have been working with patients having fructose intolerance for the past 3 years.
I was introduced to it by Melinda Dennis, RD, LDN, from the Celiac Center at Beth Israel Deaconess Medical Center in Boston. Clinically, I usually recommend a 2-phase FODMAP elimination diet. Most of my patients are already on a gluten-free diet
and may have other dietary restrictions when we begin to work with the FODMAP diet.
I explain that fructose tolerance is individual and cumulative; we eliminate the high-fructose and high-lactose foods first, which drops their overall FODMAP load, and this usually leads to significant improvement in their IBS symptoms within a week. If they have no improvement in their symptoms, then they are not likely fructose intolerant. If they have improved but still have residual symptoms, we work to identify their individual sensitivities to specific foods or to a specific FODMAP category. The most common category my patients react to beyond lactose and fructose is the fructans, especially garlic and onions and any of the polyol sugar alcohols. I advocate for the lowest amount of restriction of fruits and vegetables high in nutrient density that patients’ bowel tolerance will allow. Some choose to eliminate all high-FODMAP foods for 2 to 3 weeks and then reintroduce each category one at a time. There is not a digestive enzyme equivalent to lactase that increases FODMAP tolerance, but apparently taking glucose pills when ingesting fructose can increase absorption, leading to fewer IBS symptoms. It is not yet understood by what mechanism glucose improves fructose absorption. I have not worked with this clinically, but for further information please refer patients to the book IBS—Free at Last! by Patsy Catsos, MS, RD, LD, for dosing instructions.10
A 62-year-old female patient was referred to me by a local chiropractor for evaluation of her IBS. She had a prior diagnosis of Sjögren syndrome. She presented with daily gas and bloating and alternating episodes of constipation and diarrhea. She had previously eliminated gluten and had experienced minor improvement of her gastrointestinal symptoms as a result. I noticed she was chewing gum during our interview for the dry mouth that resulted from her Sjögren syndrome. Her diet contained several daily high-fructose foods, including apples, pears, juices, dried fruit, and some high-fructose corn syrup. I gave her a copy of the FODMAP diet and discussed the implementation of the diet, and we decided to use the FODMAP elimination as the test as opposed to possibly exacerbating her symptoms with a fructose challenge breath test. She was shocked when I explained that the sugar-free gum she was chewing contained the polyol xylitol and that her 2 packs a day of gum could be one of the major triggers of her IBS symptoms, which turned out to indeed be the case. I followed up with her 3 weeks later, and her symptoms were 70% improved. We had to add a lipase supplement to her diet for fat digestion, as people with Sjögren syndrome often have pancreatic insufficiency because the exocrine pancreatic secretions can be affected. She then experienced 95% resolution of her IBS symptoms. She had to switch to sugar-sweetened gum and limit the amount she chewed to the minimum quantity needed to assist with her severe dry mouth; this did not trigger her IBS.
Take-home Message
It is normal to experience gastrointestinal symptoms as a result of ingesting too many FODMAPs and exceeding the body’s ability to absorb them.11 Some of you who work in pediatrics may encounter patients with HFI, and the disease may be present in undiagnosed adults. If you have not already been diagnosing fructose intolerance and working with the FODMAP diet, I hope this valuable clinical tool will help you address the cause in some of your patients with IBS. Preliminary research has found that the FODMAP diet appears to improve bowel symptoms in patients with inflammatory bowel disease, but more research is needed.12 I think it is interesting to note that wheat, rye, and barley are the only FODMAP-containing grains. Fructose intolerance may be driving some of the popularity of the gluten-free diet and explains why some patients have a dramatic improvement in their IBS symptoms that cannot be justified by antibody testing. There are many conflicting lists of what foods contain FODMAPs. This is an evolving area of understanding, and no doubt the FODMAP lists will reflect that as they get fine-tuned. In my clinical practice I am finding patients with refractory GERD, without IBS symptoms, who respond very well to the FODMAP diet.
 Christine Doherty, ND graduated from Bastyr University, Seattle, Washington, in 1998. She has been in private practice, specializing in gluten-based disorders at Balance Point Natural Medicine in Milford, New Hampshire. She has been lecturing and writing about gluten since discovering her own gluten sensitivity in 2003. She was 1 of the top 50 international celiac experts invited to contribute to the American Gastroenterological Association’s award-winning 2010 book Real Life With Celiac Disease. She formulates C-liac Vitality supplements, available at www.glutenfreevitamins.com.
Christine Doherty, ND graduated from Bastyr University, Seattle, Washington, in 1998. She has been in private practice, specializing in gluten-based disorders at Balance Point Natural Medicine in Milford, New Hampshire. She has been lecturing and writing about gluten since discovering her own gluten sensitivity in 2003. She was 1 of the top 50 international celiac experts invited to contribute to the American Gastroenterological Association’s award-winning 2010 book Real Life With Celiac Disease. She formulates C-liac Vitality supplements, available at www.glutenfreevitamins.com.
References
Wikipedia. Augustin-Pierre Dubrunfaut. http://en.wikipedia.org/wiki/Augustin-Pierre_Dubrunfaut. Accessed November 7, 2012.
World Gastroenterology Organisation. World Gastroenterology Organisation practice guidelines: celiac disease. http://www.worldgastroenterology.org/assets/downloads/en/pdf/guidelines/04_celiac_disease.pdf. Accessed November 7, 2012.
Gibson PR, Newnham E, Barrett JS, Shepherd SJ, Muir JG. Review article: fructose malabsorption and the bigger picture. Aliment Pharmacol Ther. 2007;25(4):349-363.
HFI Laboratory at Boston University. Specifics of HFI and its diagnosis. www.bu.edu/aldolase/HFI/hfiinfo.html. Accessed December 12, 2012.
Yasawy MI, Folsch UR, Schmidt WE, Schwend M. Adult hereditary fructose intolerance. World J Gastroenterol. 2009;15(19):2412-2413.
Mann NS, Cheung EC. Fructose-induced breath hydrogen in patients with fruit intolerance. J Clin Gastroenterol. 2008;42(2):157-159.
Müller P, Meier C, Böhme HJ, Richter T. Fructose breath hydrogen test: is it really a harmless diagnostic procedure? Dig Dis. 2003;21(3):276-278.
Shepherd Works. Low FODMAP diet. http://shepherdworks.com.au/disease-information/low-fodmap-diet. Accessed November 7, 2012.
Barrett JS, Gibson PR. Disaccharides, monosaccharides and polyols (FODMAPs) and nonallergic food intolerance: FODMAPs or food chemicals? Therap Adv Gastroenterol. 2012;5(4):261-268.
Catsos P. IBS: Free at Last! Pond Cove Press; 2009.
Beyer PL, Caviar EM, McCallum RW. Fructose intake at current levels in the United States may cause gastrointestinal distress in normal adults. J Am Diet Assoc. 2005;105(10):1559-1566.
Gearry RB, Irving PM, Barrett JS, Nathan DM, Shepherd SJ, Gibson PR. Reduction of dietary poorly absorbed short-chain carbohydrates (FODMAPs) improves abdominal symptoms in patients with inflammatory bowel disease: a pilot study. J Crohns Colitis. 2009;3(1):8-14.























