Orthobiologics and Epicondylosis: Tendon Healing Using Microfragmented Adipose Tissue and PRP
TERRANCE MANNING II, ND, RMSK
A 53-year-old male presented to the clinic with persistent right lateral elbow pain. The pain onset was insidious, yet this patient had had recurrent symptoms for several years; the most recent episode started 8 months before this visit. The patient had tried rest, ice, therapeutic ultrasound with iontophoresis, kinesiology taping, and 4 months of physical therapy. Unfortunately, symptoms persisted, and in fact were worsening. Pain was rated 7/10, aggravated by repetitive wrist extension. Patient had normal BMI and no contributory medical history or comorbidities.
Patient Evaluation
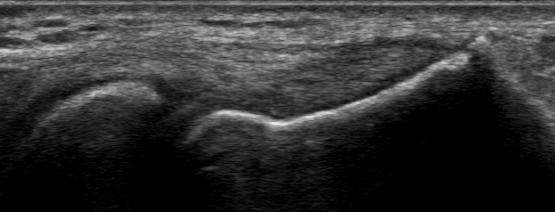
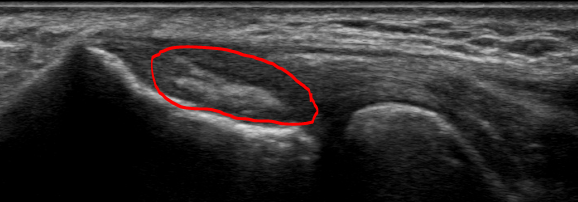
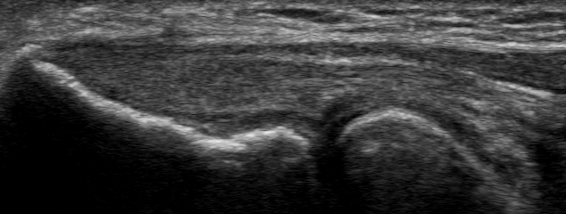
The cervical spine was evaluated for potential C5 radiculopathy. Cervical range of motion, Spurling’s test, and maximal foraminal compression test were negative and did not reproduce the chief complaint symptoms. Upper extremity muscle strength was 5/5, while reflexes were 2+ and symmetric. The elbow appeared normal on gross inspection and was stable against valgus and varus stressing. Resisted wrist extension reproduced lateral elbow pain – a positive Cozen’s test. Maudsley’s test was also positive, provoking a tender lateral epicondyle with resisted extension of the 3rd digit. Immediately following the clinical exam, a point-of-care diagnostic ultrasound was performed, significant for partial tearing of the originating fibers of the proximal common extensor tendon in the setting of moderate tendinosis (Figure 1). Routinely, when pathology is suspected or found, the same structure will be evaluated on the contralateral side for the sake of comparison. Figure 2 exhibits the left common extensor tendon, a more normal-appearing tendon without partial tearing. In this complete diagnostic ultrasound, the other evaluated structures were unremarkable.

Diagnosis
Lateral epicondylitis is the most common cause of elbow pain, associated with persistent lateral elbow pain of a mechanical nature.1,2 This is often a clinical diagnosis that does not require diagnostic imaging. In most patients, it resolves with rest, physical therapy, and a course of oral non-steroidal anti-inflammatory medication.1,2 Yet the diagnosis of lateral epicondylitis is not very specific and could be better delineated.
The underlying cause of lateral epicondylitis usually involves tendinopathic changes of the common extensor tendon.1,2 This tendon is the proximal origin at the lateral epicondyle for wrist extensor muscles. These include the extensor carpi radialis brevis and longus, extensor digitorum, extensor digiti minimi, and extensor carpi ulnaris muscles. This tendon is activated with wrist extension and is susceptible to microinjuries that continue to provide nociceptive input if not allowed to fully heal. Continued, repetitive mechanical stressing will prevent the tendon from healing, which keeps the injury symptomatic. Thus, when diagnosing lateral epicondylitis, the more specific diagnosis is usually tendinosis of the common extensor tendon. It is important not to miss radial collateral ligament instability, sprain, or tears when evaluating lateral elbow pain. The acuteness of the injury is what differentiates lateral epicondylitis/common extensor tendinitis from lateral epicondylosis/common extensor tendinosis; the former can be diagnosed from the onset of symptoms to 6 weeks, while the latter involves 6 weeks or more of lateral elbow pain.
The actual health of the tendon and the severity of the pathology cannot be well established without imaging. The level of pain and dysfunction alone associated with this condition cannot predict the severity of the tendinopathy. Ultrasound imaging can provide a high-resolution visualization of the tendon and associated structures (like the radial collateral ligament). This can help the practitioner accurately grade the severity of the tendinopathy and effectively direct treatment. X-ray imaging does not provide direct visualization of the soft tissue extensor tendon. An MRI is sensitive and specific in diagnosing common extensor tendon pathology, but MRI is much more expensive than ultrasound and cannot be performed at point of care.
In this patient case, the diagnostic ultrasound showed hypoechoic changes and thickening of the common extensor tendon, both expected with tendinosis. But it also revealed multiple small partial tears. The individual tears were low grade but taken as a whole, the partial tearing was rated as moderate. This, then, was not a straightforward case of lateral epicondylosis, but a case of a moderate grade, partial common extensor tendon tear, the complexity of which had significant implications for the treatment plan.
Therapeutic Intervention
Several studies have shown that platelet rich plasma (PRP) injection therapy can be effective for the treatment of tendinosis, including common extensor tendinosis.1-5 Yet there has been limited data on treating common extensor tendon partial tears. PRP is known to be very fluidlike, with low viscosity. If used solely to treat partial tendon tears, there is concern that the injected PRP may flow away from the tears and not provide as much of a local perfusion of the tendon as is needed to heal them. Injection of PRP may confer a temporary reduction in symptoms, optimization of the intact tendon fibers, and allow for a temporary increase in function. Orthopedic surgeons and sports medicine specialists may consider a palliative corticosteroid injection around or into the tendon. However, this should not be considered in this case, since a corticosteroid injection is likely to cause more harm than good by thinning the already-partially torn tendon fibers, possibly predisposing this tendon to a full rupture, necessitating surgical repair.
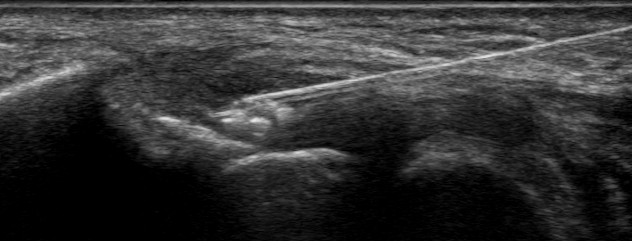
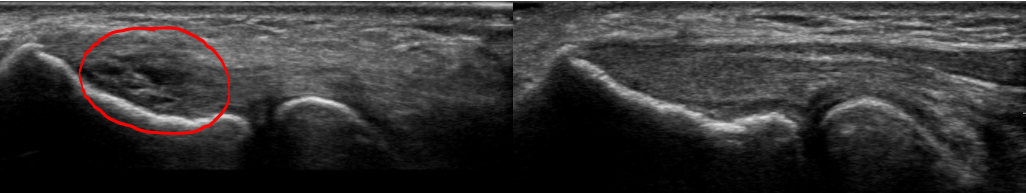
Within the field of orthobiologics (the use of biological products to treat orthopedic conditions), there are other autologous tissue grafts that can be used to mount a profound and local healing response. The 2 main tissue grafts are bone marrow aspirate concentrate (BMAC) and microfragmented adipose tissue (MFAT). These tissues are both reservoirs for mesenchymal stem cells (MSCs) that can differentiate into tissues including tendon, ligament, bone, and cartilage.6 Despite concern for patient tolerability of the bone marrow aspiration procedure, there have been several studies showing optimal technique, safety of the procedure, and an almost pain-free experience.7-10 BMAC shares significant physical attributes with PRP; both have low viscosity and flow easily. Likewise, when injected, BMAC is unlikely to stay and fill in the partial tears; although it may provide temporary pain relief and improved function, a patient’s condition will return if the tears do not fully heal. MFAT is acquired by performing a mini-liposuction procedure within the subcutaneous adipose layer; this procedure is generally well tolerated by patients if performed using ultrasound guidance and the proper tissue planes are interrogated. In contrast to the fluidlike BMAC and PRP, an MFAT graft is very viscous, does not flow easily, and has more solid adipose tissue, including a collagen matrix and MSCs. This tissue can be directly placed using ultrasound guidance into the partial tears of tendons, ligaments, and fibrocartilage (as seen in menisci and labra). Further, MFAT can be used to fill in the tendon defect while having a cellular effect to heal the tendon.11 Due to these advantageous physical characteristics, an MFAT graft in combination with PRP delivered under direct ultrasound guidance was chosen as the treatment. The goal of the therapy was primarily to heal the partial tears without surgery and enable the patient to return to pain-free full normal function. Figures 3a and b demonstrate the ultrasound guided administration of the MFAT+PRP directly into the tendon tears.
Follow-up and Outcome
At the 6-week follow-up, the patient reported resolution of resting pain and 3/10 pain with repetitive wrist extension. He reported 80% overall improvement and noted that he was continuing to improve. He had completed 4 weeks of post-treatment physical therapy and was discharged after meeting all treatment milestones and objectives. At this follow-up, a post-procedure ultrasound scan was deferred since it was too soon after the intervention.
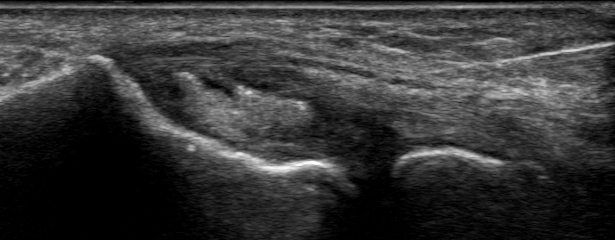
At the 12-week follow-up, the patient noted a complete resolution of symptoms, both at rest and with repetitive movements. He had no restrictions and was extremely satisfied with the progress. Figure 4 demonstrates the post-intervention tendon appearance on ultrasound scan. Of note, the adipose graft remains intact despite full activity level. In addition, the echotexture of the adipose graft resembles adipose tissue more than tendon during this phase of healing.

At the 20-week follow-up, the patient continued to have significant improvement. The clinical exam was negative, and Figure 5 demonstrates the 20-week post-intervention tendon appearance. The adipose graft is still visualized, yet the appearance of the graft is more tendinous.
At the 36-week follow-up, the patient noted 95% improvement, no pain at rest or with activities, and only very occasional low-grade pain after using hedge clippers for several hours. Figure 6 demonstrates the 36-week post-intervention diagnostic ultrasound showing a near-normal appearance of the common extensor tendon. Here, the areas of partial tearing have fully resolved, and where the adipose graft was placed, now is a normal fibrillar collagen appearance. Figure 7 shows comparison of the pre- and post-intervention diagnostic ultrasounds, showing a healed tendon that appears nearly normal.
Discussion
Even though lateral epicondylitis is the most common underlying cause of patients who complain of elbow pain, this is often an inaccurate or incomplete diagnosis. Ultrasound evaluation of the elbow, including the common extensor tendon, can result in a more precise diagnosis. In this case, the underlying cause of lateral elbow pain was a moderate grade partial tear of the common extensor tendon, a condition that is unlikely to heal without intervention.
As evidenced by comparing the pre-procedure and 36-week ultrasound scans, this case demonstrates the healing of a moderate grade partial thickness tearing of the common extensor tendon using MFAT plus PRP. There has been a study showing healing of a partial-thickness supraspinatus tendon tear using MFAT plus PRP, but healing of a common extensor tendon tear with this treatment has not been previously documented.12 MFAT is a particularly good choice of orthobiologic substance to treat partial-thickness tendon tears. Moreover, its regenerative potential enables it to engraft and differentiate into normal tendon through its resident MSCs. MFAT also has the advantageous physical properties of high viscosity and intact collagen matrix that allow it to fill in tendon tissue defects. This patient was a particularly good candidate for this therapy: he was fit, healthy, and had no medications or medical comorbidities that would be barriers to an optimal outcome. Furthermore, the patient complied with post-procedure physical therapy and rehabilitation, which helped ensure complete healing and normal remodeling of the tendon after the MFAT graft.
Regenerative medicine and/or orthobiologic procedures are gaining popularity within the naturopathic profession. This author would like to point out that proficiency in diagnostic musculoskeletal ultrasound takes years of post-graduate training. In addition, multi-year post-graduate training is recommended to acquire and administer orthobiologic therapy safely and effectively. Despite the need for advanced training and compliance with the scope of practice in the naturopathic doctor’s respective state, orthobiologic therapy is firmly within the principles of our profession. Harnessing not just the physical components, but the vital force of a tissue and directly administering it to a diseased or dysfunctional tissue is naturopathic medicine. Orthobiologic therapy works with the body’s innate healing mechanism to treat the root cause of a patient’s musculoskeletal dysfunction, as exhibited by this outstanding outcome.
[REFS]- Ma KL, Wang HQ. Management of Lateral Epicondylitis: A Narrative Literature Review. Pain Res Manag. 2020;2020:6965381.
- Van Schaik KD, Lee KS. Orthobiologics: Diagnosis and Treatment of Common Tendinopathies. Semin Musculoskelet Radiol. 2021;25(6):735-744.
- Dallaudière B, Pesquer L, Meyer P, et al. Intratendinous injection of platelet-rich plasma under US guidance to treat tendinopathy: a long-term pilot study. J Vasc Interv Radiol. 2014;25(5):717-723.
- Ford RD, Schmitt WP, Lineberry K, et al. A retrospective comparison of the management of recalcitrant lateral elbow tendinosis: platelet-rich plasma injections versus surgery. Hand (N Y). 2015;10(2):285-291.
- Raeissadat SA, Sedighipour L, Rayegani SM, et al. Effect of Platelet-Rich Plasma (PRP) versus Autologous Whole Blood on Pain and Function Improvement in Tennis Elbow: A Randomized Clinical Trial. Pain Res Treat. 2014;2014:191525.
- Caplan AI. Mesenchymal stem cells. J Orthop Res. 1991;9(5):641-650.
- Bain BJ. Bone marrow aspiration. J Clin Pathol. 2001;54(9):657-663.
- Bain BJ. Bone marrow biopsy morbidity and mortality. Br J Haematol. 2003;121(6):949-951.
- Friedlis MF, Centeno CJ. Performing a Better Bone Marrow Aspiration. Phys Med Rehabil Clin N Am. 2016;27(4):919-939.
- Long JR, Stensby JD, Wiesner EL, et al. Efficacy and safety of bone marrow aspiration and biopsy using fluoroscopic guidance and a drill-powered needle: clinical experience from 775 cases. Eur Radiol. 2020;30(11):5964-5970.
- Clevenger TN, Luna G, Fisher SK, et al. Strategies for bioengineered scaffolds that support adipose stem cells in regenerative therapies. Regen Med. 2016;11(6):589-599.
- Marathe A, Song B, Jayaram P. Microfragmented Adipose Tissue With Adjuvant Platelet-Rich Plasma Combination Therapy for Partial-Thickness Supraspinatus Tear. Cureus. 2021;13(6):e15583.
Terrance Manning II, ND, RMSK, is an interventional orthopedic and orthobiologic medicine specialist focusing on nonsurgical treatment of joint, tendon, and ligament issues. Dr Manning’s 3-year post-graduate CNME-accredited residency in regenerative medicine is unique among his peers. He is an expert in diagnostic and interventional musculoskeletal ultrasound. He is an adjunct clinical faculty member at National University of Natural Medicine and hosts an off-site shift for training students in this field. Dr Manning is a founding member and current vice president of the Naturopathic Orthopedic Medicine Academy (NOMA).