Traumatic Brain Injury: Impact, Assessment & Management of Concussion & mTBI
Matthew Bennett, ND, BaHSc, dAp
Christopher Knee, ND, MSc
Concussion is recognized as a clinical syndrome of biomechanically induced brain dysfunction, with or without loss of consciousness, as a result of rapid linear or rotational forces applied to the head or neck.1 Mild concussion would be classified as a mild traumatic brain injury (TBI); however, not all TBIs are concussions. While the majority of concussions resolve within 7 to 10 days, some symptoms persist for weeks, months, or even years beyond the initial injury.2 In fact, about 15% of those who experience a TBI will be persistently symptomatic,3 most commonly in the area of cognitive dysfunction and attention deficits, which cannot always be identified on neuropsychological testing.4,5 Additionally, about 95% of individuals who have sustained a mild TBI (mTBI) report chronic pain, compared to only 22% of individuals who have suffered a moderate-to-severe TBI.4
Over the past decade, the incidence of TBI in sport, workplace, and motor vehicle accidents has risen vastly in both individual reporting as well as media attention.6,7 Almost 4 million sport concussions occur each year in the United States; however, the reporting rate can be as low as 50%.2 In Canadian Junior Hockey players, TBI occurs at a rate of 21.5 per 1000 exposures.8 According to the Centers for Disease Control and Prevention (CDC), emergency departments within the United States admit 2.5 million TBI visits per year, with deaths totaling greater than 50 000; TBIs occurring from a fall account for 40.5% of total TBI visits.9 Repetitive concussions or mTBIs are increasingly being linked with chronic traumatic encephalopathy (CTE), a neurodegenerative condition appearing often decades after TBI exposure and which is prevalent in professional athletes. While the acute dangers of TBI are well documented, the goal of this article is to highlight the greatly underappreciated long-term health implications of TBI (even those that appear to have resolved), as well as describe its pathophysiology, propose a novel algorithm for management, and outline potential treatment approaches.
Definition and Pathophysiology of TBI
While the definition of TBI has changed over the past 60 years, it is most imperative as primary care practitioners to monitor patient progress throughout recovery, as the pathophysiology is complex with a thin foundation of supporting research for treatment and management. A number of events are occurring throughout a TBI – structurally, the acceleration or torque forces resulting in stretching and tearing of axonal fibers is referred to as “shear strain,” while neurochemically, a cascade of reactions occurs during any TBI, often resulting in cell death.10 The mTBI does not cause disruption seen via a CT scan of the brain; however, it does cause a rapid onset of neurophysiological and neural dysfunction, which may subside within seconds, minutes, or a few hours of the external force. At a cellular level, the rapid stretching of axons causes a disruption to sodium and calcium homeostasis, which may further cause depolarization of neurons, increased glucose consumption, reduced energy storage, and impaired oxidative metabolism and glycolysis, resulting in acidosis and neural edema. Unfortunately, the brain is extremely sensitive to shifts in cellular metabolism, as it has a very high metabolic rate and does not store glucose.11
Many of the pathological changes involved with CTE are similar to other neurodegenerative conditions, such as Alzheimer and Parkinson’s diseases, including widespread tau deposits.12,13 McKee et al (2009) described concerning CTE findings among football players, including mood disorders, memory loss, confusion, and poor concentration.14
There have been a number of proposed mechanisms to explain the slowly progressive encephalopathy (CTE) resulting from repetitive TBI. Recently, Blaylock et al (2011) outlined the process of immunoexcitotoxicity as a central mechanism in CTE.12 Briefly, the trauma triggers an interaction between CNS immune receptors and excitatory glutamate receptors, leading to a cascade of reactions involving reactive oxygen and nitrogen species generation, lipid peroxidation, prostaglandin activation, and ultimately synaptic injury and mitochondrial suppression.12 Walker et al (2013) have also provided a detailed description of the molecular mechanisms involved after a TBI.15 Most recently, Morley et al (2014) introduced the concept of “diminished brain resilience syndrome,” essentially a functional nutrient deficiency and disrupted homeostasis leading to increased susceptibility of second impact syndrome (SIS), discussed below.16 The syndrome is especially characterized by deficiencies of glutathione, melatonin, zinc, and magnesium, and can be worsened by environmental toxin exposure and gut dysbiosis.16
Long-Term Implications
As early as 1962, it was recognized that concussions, regardless of severity, might result in permanent neurologic impairment.10 Tragically, the long-term implications of concussion and TBI, whether through sport or general trauma, are horribly underappreciated. However, there is now overwhelming evidence to demonstrate that TBIs are risk factors for organic personality changes, anger, depression, suicide, anxiety, and neurodegenerative conditions such as Alzheimer’s and Parkinson’s diseases.3
Due to the typical reduction of clinical symptoms within 1-2 weeks, many patients and clinicians fail to forego follow-up treatment and prevention of further physiological changes. However, long-term effects can be more difficult to measure; for example, a recent case study found that athletes with a history of 3 or more concussions performed more poorly on pre-season neuropsychological testing, suggesting lingering memory deficits.17 The collection of the trauma, neuropathology and neuropsychiatric changes are fueling attention for the early detection of CTE through novel fluid biomarkers.18-20 While research is limited, the observation and collection of total tau protein and gamma-enolase via cerebrospinal fluid (CSF) and blood appear to have the greatest traction.21 Notably, CTE is not a continuation of post-concussive syndrome or symptoms from a previous concussion, but rather an organic condition often developing decades after exposure.2
Unrelated to CTE, second impact syndrome (SIS) occurs when an individual who has recently sustained a head injury, but has not recovered completely, sustains a second injury; often the second injury is milder, but can be fatal in 50% of cases.22 In fact, after 1 brain injury, the risk for a second is 3 times higher; after a second injury, the risk for a third is 8 times higher.3
Primary Assessment and Diagnosis
The most common signs and symptoms of a concussion are presented in Table 1. Symptoms can be subjective or objective, and are often vague or nonspecific; worse, there is no proven correlation between the severity of a concussion and the likelihood of 1) having post-concussive symptoms; 2) having any structural damage; or 3) the presence of any psychological factors.2 Approximately 20% of the TBI population also meets criteria for chronic daily headaches, beginning as early as 1 week post-trauma; additionally, post-traumatic headache accounts for about 4% of all headaches in primary care.23 In a 2012 cross-sectional study conducted by Theller et al within a cohort of 978 soldiers, an extraordinary 78% (761) reported episodic headaches.24
[Insert table]:Table 1. Common Signs & Symptoms of a Concussion
| Physical | HeadacheNausea/vomitingBalance problemsDizziness
Visual problems Fatigue Sensitivity to light/noise Numbness/tingling |
| Cognitive | Brain fogSlower thoughtsPoor concentrationPoor memory
Confusion Language problems |
| Emotional | IrritabilitySadnessMore emotionalNervousness |
| Sleep | DrowsinessSleeping more/less than usualDifficulty falling asleep |
Sideline evaluation and management (return to play) is out of the context of this article and may be less relevant to the naturopathic clinician. Generally, imaging is reserved for athletes with suspected intracranial hemorrhage only,2 and is of limited use, since emerging evidence supports the notion that concussion is a functional, not structural, disturbance.22,25,26 Relevant assessment tools the reader should consult, and which may help in objectively measuring the resolution of symptoms, include: Sport Concussion Assessment Tool, 3rd ed (SCAT3),27 ImPACT,28 King-Devick Test,29 and HEADS UP.30
Integrative Management
Recently, Marshall et al (2012),31 among several other organizations, including the American Medical Society for Sports Medicine (AMSSM)2 and the Ontario Neurotrauma Foundation (ONF),32 developed comprehensive clinical guidelines for the management of mTBI.31
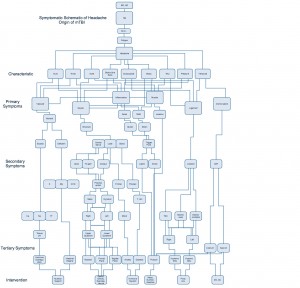
Secondary Symptoms (from left to right): optic nerve, tri-gem (trigeminal nerve), occipital and frontal lobes, pituitary glands (T: testosterone, GH: growth hormone). Interventions (from left to right): nutrition support, spatial training, gravity training, exercise, neural training, hormone support, meso (mesotherapy), prolo (prolotherapy), acupuncture, DO (osteopathic-) and DC (chiropractic-) manipulation.
However, the high incidence of headaches seen in clinical practice drove the current author Bennett to investigate multiple causes of the reports. Through collection of patient data (manuscript in preparation), Figure 1 was created as a novel algorithm to aid the practitioner in the assessment of TBI and to outline the most effective treatment approaches. Bennett implies by Figure 1 the most efficient interventions, culminating from an investment of over 8 years of extensive clinical exposure and investigation of mTBI within the athletic population aged 14-55 years.
Figure 1. Assessment & Management of Concussion and mTBI: Proposed Algorithm
As an example, a patient with a history of TBI presents with the complaint of fatigue and temporal headache. The physician explores the mechanism of injury, symptoms, characteristics, and rules out cranio-sacral involvement, as there was no evidence of disrupted CSF or signs of cranium or sacral fracture. The investigation should then, according to Bennett’s algorithm, focus on ligamentous origin, during which the location of pain is discovered at the atlanto-axial joint, with hypermobility on the right side. According to clinical records and experience, the most efficient intervention at this point would be prolotherapy or acupuncture, in order to proliferate and strengthen the associated ligament and reduce symptoms of the headache (Figure 1). The practitioner can follow this process according to clinical presentation and physical findings.
Nutritional Supplementation in TBI
There is obviously a wide variety of options available for the natural health practitioner regarding the treatment and prevention of mTBI, including nutritional supplementation, physical therapy, acupuncture, and homeopathy. Individually, the evidence for each agent could be deserving of its own review. To date, much of the research involving mTBI is focused on either the resolution of symptoms or reducing the risk of long-term complications, most commonly through correcting nutritional deficiencies, slowing or protecting against neurodegeneration, and reducing the immunoexcitatory response. It is not the purpose of this article to review all of the evidence for naturopathic treatments of mTBI; however, it is worth noting a few interventions for which a higher degree of evidence exists. Recently, Petraglia et al (2011) provided an extensive review of the evidence surrounding a variety of natural medicines.33 Blaylock et al (2012) have also provided detailed evidence of several compounds (including curcumin, quercetin, and magnesium), which may be effective against TBI-associated inflammation and excitotoxicity.34 Practitioners are encouraged to continue to use therapies they believe to be safe and effective based on clinical experience. Overall, high-quality human data are lacking; however, hundreds of preclinical studies have been performed with promising results.
Omega-3 Fatty Acids
Omega-3 fatty acids, specifically docosahexaenoic acid (DHA) from marine sources, are a crucial component of neuronal membranes and play a vital role in the structure and function of neurons, supporting membrane fluidity and helping to control oxidative stress and inflammation.35,36 DHA supplementation can significantly reduce the axonal damage caused by a TBI,33 and within just a few weeks has been shown to reduce the effects of subsequent brain trauma and improve cognitive function.35 When fed an omega-3-enriched diet for 2 months, mice exhibited reduced short- and long-term behavioral deficits and reduced neuronal loss and inflammation after an induced TBI.37
Polyphenols
Specifically those derived from flavonoids, polyphenol compounds found in berries and green tea have a high antioxidant capacity, have been shown to reduce stroke risk, and may improve cognitive deficits resulting from mTBI. Resveratrol, which has antioxidant and neuroprotective effects, can cross the blood-brain barrier (BBB) and has been shown to improve TBI outcomes in animal models.33
Curcumin
Curcumin has been found to be effective in reversing neuronal dysfunction in several models of neurodegenerative disease, including Alzheimer’s.35 Curcumin can cross the BBB and has a strong antioxidant capacity, which may help reduce lipid peroxidation and protect the hippocampus against learning impairments. Additionally, recent animal research has shown curcumin to improve TBI outcomes by restoring energy homeostasis in the brain and reducing neuroinflammation.33,35
Creatine
An amino-acid like compound, creatine plays a large role as a fast-energy reserve in both brain and skeletal muscle; however, it is also found in the CNS, crosses the BBB, and contributes to proper neuronal structure and function, membrane potential, calcium homeostasis, and neurotransmission.33
Branched-Chain Amino Acids (BCAAs)
A recent study found that levels of BCAA metabolites were reduced 24 hours after mTBI, which may lead to decreased energy production and neurotransmitter synthesis; therefore, supplementation with BCAAs or their metabolites may reduce TBI pathology and improve outcomes.11
Zinc
Urinary zinc excretion is increased, and serum zinc levels decreased, in patients with acute brain injury.38 Further, data shows that treatment using dietary and parenteral zinc supplementation can reduce TBI-associated depression and improve cognitive function, specifically spatial learning and memory.38
Conclusions
While previously focused on the validation of assessment tools, concussion research is now shifting attention towards education, acute biomarkers, and treatment. Overall, standards of care should include postural education, ROM exercises, cognitive and physical rest until asymptomatic, and a graded exertion protocol.39 Coordinated clinical care with regular follow-up is of utmost importance, as emerging evidence continues to illustrate the far-reaching, often fatal, long-term impact of mTBI and concussion.
 Matthew Bennett, ND, BaHSc, dAp, is the founder of Active Solutions Medicine in Vancouver, BC, and focuses his practice on performance and pain relief. Individuals receive the highest care with nutrition and physical medicine for the purpose of prevention and reconditioning of musculoskeletal injuries. He has worked in professional leagues (NHL, CFL, MLB, and AHL), completing daily assessments and rehabilitation of various biomechanical and structural dysfunctions. For more information, visit www.activesolutionsmedicine.com.
Matthew Bennett, ND, BaHSc, dAp, is the founder of Active Solutions Medicine in Vancouver, BC, and focuses his practice on performance and pain relief. Individuals receive the highest care with nutrition and physical medicine for the purpose of prevention and reconditioning of musculoskeletal injuries. He has worked in professional leagues (NHL, CFL, MLB, and AHL), completing daily assessments and rehabilitation of various biomechanical and structural dysfunctions. For more information, visit www.activesolutionsmedicine.com.
 Christopher Knee, ND, MSc, is a naturopathic clinician, researcher, health and wellness author, and guest speaker. Currently, he is the Nutrition director and naturopathic doctor for the Ottawa Police Real You corporate wellness program in Ottowa, Ontario, and is also a research associate for the Canadian College of Naturopathic Medicine. For more information, visit www.christopherkneend.com or follow him on Twitter @drcknee.
Christopher Knee, ND, MSc, is a naturopathic clinician, researcher, health and wellness author, and guest speaker. Currently, he is the Nutrition director and naturopathic doctor for the Ottawa Police Real You corporate wellness program in Ottowa, Ontario, and is also a research associate for the Canadian College of Naturopathic Medicine. For more information, visit www.christopherkneend.com or follow him on Twitter @drcknee.
References:
- Giza CC, Kutcher JS, Ashwal S, et al. Summary of evidence-based guidelines update: Evaluation and management of concussion in sports: Report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2013;80(24):2250-2257.
- Harmon KG, Drezner J, Gammons M, et al. American Medical Society for Sports Medicine Position Statement: Concussion in Sport. Clin J Sport Med. 2013;23(1):1-18.
- Kiraly M, Kiraly SJ. Traumatic brain injury and delayed sequelae: a review – traumatic brain injury and mild traumatic brain injury (concussion) are precursors to later-onset brain disorders, including early-onset dementia. ScientificWorldJournal. 2007;7:1768-1776.
- Beaupre M, De Guise E, McKerral M. The Association Between Pain-Related Variables, Emotional Factors, and Attentional Functioning Following Mild Traumatic Brain Injury. Rehabil Res Pract. 2012;2012:924692.
- Peterson CL, Ferrara MS, Mrazik M, et al. Evaluation of neuropsychological domain scores and postural stability following cerebral concussion in sports. Clin J Sport Med. 2003;13(4):230-237.
- Benson BW, Meeuwisse WH, Rizos J, et al. A prospective study of concussions among National Hockey League players during regular season games: the NHL-NHLPA Concussion Program. 2011;183(8):905-911.
- Gilchrist J, Thomas KE, Xu L, et al. Nonfatal traumatic brain injuries related to sports and recreation activities amount persons < 19 years – United States, 2001-2009. Morbidity and Mortality Weekly Report. 2011;60(39):1337-1342. CDC Web site. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6039a1.htm. Accessed March 1, 2015.
- Clay MB, Glover KL, Lowe DT. Epidemiology of concussion in sport: a literature review. J Chiropr Med. 2012;12(4):230-251.
- Centers for Disease Control and Prevention. Traumatic Brain Injury in the United States: Fact Sheet. Updated January 12, 2015. CDC Web site. http://www.cdc.gov/traumaticbraininjury/get_the_facts.html. Accessed March 1, 2015.
- Kelly JC, Amerson EH, Barth JT. Mild traumatic brain injury: lessons learned from clinical, sports, and combat concussions. Rehabil Res Pract. 2012;23012:371970.
- Jeter CB, Hergenroeder GW, Ward NH 3rd, et al. Human mild traumatic brain injury decreases circulating branched-chain amino acids and their metabolite levels. J Neurotrauma. 2013;30(8):671-679.
- Blaylock RL, Maroon J. Immunoexcitotoxicity as a central mechanism in chronic traumatic encephalopathy – a unifying hypothesis. Surg Neurol Int. 2011;2:107.
- Saulle M, Greenwald BD. Chronic traumatic encephalopathy: a review. Rehabil Res Pract. 2012;2012:816069.
- McKee AC, Cantu RC, Nowinski CJ, et al. Chronic traumatic encephalopathy in athletes: Progressive tautopathy after repetitive head injury. J Neuropathol Exp Neurol. 2009;68(7):709-735.
- Walker KR, Tesco G. Molecular mechanisms of cognitive dysfunction following traumatic brain injury. Front Aging Neurosci. 2013;5:29.
- Morley WA, Seneff S. Diminished brain resilience syndrome: a modern day neurological pathology of increased susceptibility to mild brain trauma, concussion, and downstream neurodegeneration. Surg Neurol Int. 2014;5:97.
- Iverson GL, Echemendia RJ, Lamarre AK, et al. Possible lingering effects of multiple past concussions. Rehabil Res Pract. 2012;2012:316575.
- Conti A, Sanchez-Ruiz Y, Bachi A, et al. Proteome study of human cerebrospinal fluid following traumatic brain injury indicates fibrin(ogen) degradation products as trauma-associated markers. J Neurotrauma. 2004;21(7):854-863.
- Davis GA, Iverson GL, Guskiewicz KM, et al. Contributions of neuroimaging, balance testing, electrophysiology and blood markers to the assessment of sport-related concussion. Br J Sports Med. 2009;43 Suppl 1:i36-i45.
- Fraser DD, Close TE, Rose KL, et al. Severe traumatic brain injury in children elevates glial fibirillary acidic protein in cerebrospinal fluid and serum. Pediatr Crit Care Med. 2011;12(3):319-324.
- Geyer C, Ulrich A, Gräfe G, et al. Diagnostic value of S100B and neuron-specific enolase in mild pediatric traumatic brain injury. J Neurosurg Pediatr. 2009;4(4):339-344.
- Terrell TR, Nobles T, Rader B, et al. Sports concussion management: part I. South Med J. 2014;107(2):115-125.
- Seifert TD. Sports concussion and associated post-traumatic headache. Headache. 2013;53(5):726-736.
- Theller BJ, Flynn FG, Erickson JC. Chronic daily headache in U.S. soldiers after concussion. 2012;52(5):732-738.
- Grindel SH, Lovell MR, Collins MW. The assessment of sport-related concussion: the evidence behind neuropsychological testing and management. Clin J Sport Med. 2011;11:134-143.
- Prabhu SP. The role of neuroimaging in sport-related concussion. Clin Sports Med. 2011;30(1):103-114.
- SCAT3[TM symbol]. Sport Concussion Assessment Tool – 3rd BJSM Web site. http://bjsm.bmj.com/content/47/5/259.full.pdf. Accessed March 1, 2015.
- The ImPACT Test. Available at: https://www.impacttest.com/products/?The-ImPACT-Test-2. Accessed March 1, 2015.
- King-Devick Test©® A Remove-From-Play Sideline Concussion Screening Test. In association with Mayo Clinic. Available at: http://kingdevicktest.com/for-concussions/. Accessed March 1, 2015.
- Centers for Disease Control and Prevention. HEADS UP Resource Center. Updated February 16, 2015. CDC Web site. http://www.cdc.gov/headsup/resources/index.html. Accessed March 1, 2015.
- Marshall S, Bayley M, McCullagh S, et al. Clinical practice guidelines for mild traumatic brain injury and persistent symptoms. Can Fam Physician. 2012;58(3):257-267.
- Guidelines for Concussion/mTBI & Persistent Symptoms: Second Edition. Toronto, Ontario: Ontario Neurotrauma Foundation; 2013. Available at: http://onf.org/documents/guidelines-for-concussion-mtbi-persistent-symptoms-second-edition. Accessed March 1, 2015.
- Petraglia AL, Winkler EA, Bailes JE. Stuck at the bench: potential natural neuroprotective compounds for concussion. Surg Neurol Int. 2011;2:146.
- Blaylock RL, Maroon J. Natural plant products and extracts that reduce immunoexcitotoxicity-associated neurodegeneration and promote repair within the central nervous system. Surg Neurol Int. 2012;3:19.
- Gomez-Pinilla F. The combined effects of exercise and foods in preventing neurological and cognitive disorders. Prev Med. 2011;52 Suppl 1:S75-S80.
- Malone MA, Gloyer K. Complementary and alternative treatments in sports medicine. Prim Care. 2013;40(4):945-968.
- Pu H, Guo Y, Zhang W, et al. Omega-3 polyunsaturated fatty acid supplementation improves neurologic recovery and attenuates white matter injury after experimental traumatic brain injury. J Cereb Blood Flow Metab. 2013;33(9):1474-1484.
- Morris DR, Levenson CW. Zinc in traumatic brain injury: from neuroprotection to neurotoxicity. Curr Opin Clin Nutr Metab Care. 2013;16(6):708-711.
- Lynall RC, Guskiewicz KM. Concussion research: new horizons. Lancet Neurol. 2015;14(1):14-16.