David J. Schleich, PhD
Helpful in this exercise was the eloquent work of Yon Maley (1987), whose pioneering analysis of the characteristics of the language used in legislation gave us a lens through which to look. So much of the language (words, paragraph structure, jargon, terminology) affecting naturopathic professional formation includes elements from history, social function, participant roles, the political goals of the actual legislation, and language use itself. What it boils down to, as Maley contends, is that the language of legislation (and, by extension, of the regulations) becomes “frozen authoritative text so that the language itself becomes a component of the law” (p.25). It is in this way that lay regulators end up with so much power to “interpret” regulatory language, often literally, on behalf of the profession, even though those very regulators are overseen by elected boards, most often whose members include a plurality from the profession.In recent months, we conducted a short study of the assumptions in the state and provincial legislation regulating naturopathic medicine. We examined the fundamental frameworks, essential scope detail, and definitions in 5 Canadian and 5 American “naturopathic” regulatory frameworks, as well as at the 4 regional higher-education accreditation language architectures, and their single specialty, accreditation companion (CNME). We were looking for what the language of that legislation and the ensuring civil practice regulations were actually predicated upon and how they were built into documents. That is, we were seeking to understand more clearly what the underlying assumptions were by which regulation (R) and accreditation (A) lead to professional formation (PF), if they do at all.
From the nature of the words chosen in the covenants, articles, codicils, and qualifiers, the professional member risks alienation from the very framework governing his or her actions as a healer. Those who study the language of legislation are not very praising of its nature, once the words [the rubber] hit(s) the profession’s rule book [the road].
The most frequently mentioned are archaic, foreign, uncommon words; long complex sentences with intricate patterns of coordination and subordination, repetition, passive voice, and a complete absence of color and humanity. It is commonly agreed to be a complex, intricate, even bizarre style of language.
(Maley, 1987, p.25)
Couple this with bureaucratically-inclined laypersons holding sway over what a particular article of the legislation means, and we might not be remiss in shuddering. Just when we think we’re making progress because a new law – such as the Regulated Health Professions Act (RHPA) in Ontario, or pending legislation SB 538 in California – is making headway, the defining end of the legislative body or assembly can get wobbled by the regulatory practice itself, especially if the “regulators” do not understand the philosophical and social purposes of the profession as it tries hard to take form in the 21st century.
As one ascertains what scope, entitlements, controlled acts, disciplinary processes, registrarial process, and the like are in place, it is but a short hop to judging whether the profession is on the way to increasing mastery, autonomy, and purpose (M-A-P) or is simply being side-swiped, that is, contained by the dominant, orthodox provider groups who control all the turnstiles.
For example, the legislation in Washington, Vermont, Arizona, and Oregon uses language which does not principally and cumulatively limit acts on the part of those contemplated in the laws. In contrast, the legislation in Minnesota, North Dakota, Colorado, Kansas, Ontario, Nova Scotia, and Manitoba, as cases in point, includes a number of phrases and terms which delimit what a naturopathic doctor can do, more than it leaves those very turnstiles open for augmented professional formation. And, when the guardians of the legislation, the so-called “regulators,” have no commitment to modern professional formation for naturopathic medicine, malaise ensues.
Regulation, Self-regulation, and Accreditation
By “regulation,” we mean the supervision and oversight of the profession itself, usually by organizations determined in part by the actual professions being regulated within the covenants of the legislation in their particular jurisdiction. Where the “regulators” are identified strongly with the professional formation goals of the historical group, professional formation is less ambiguous and proceeds with more confidence (as in Oregon, Vermont, and British Columbia). Where the “regulators” are unduly influenced by lay bureaucratic personnel and have less understanding of and experience with the history and character of the profession in that jurisdiction (as in present-day Ontario, for example), professional formation is slow, and dangers of assimilation by the dominant, orthodox medical system are more likely.
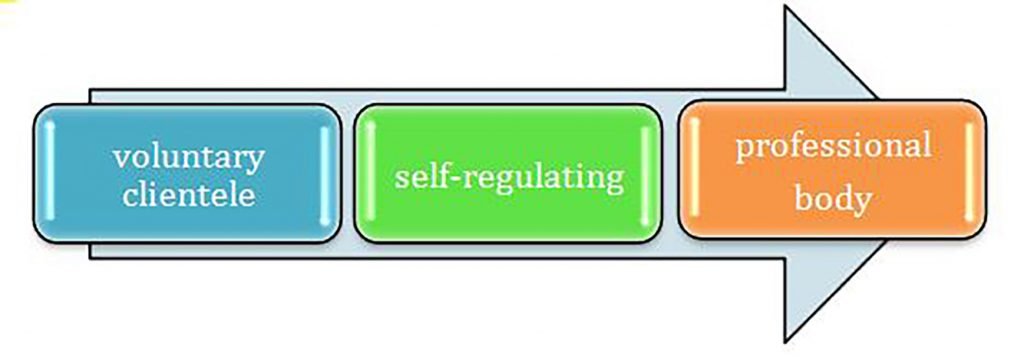
“Self-regulation” is an essential element of professional status, along with attracting a voluntary clientele (Figure 1). In the literature of professional formation, there have been recurrent debates that rust away the fabric of professionalism by virtue of the group’s protected guild status in civil society. This has been especially the case with biomedicine/allopathic workforce, whose grip on the factors of health promotion are guarded and sustained by sharply enforced entitlement, legislative monopoly, and remarkable success in long-term branding.
By “accreditation,” we mean the 3rd-party confirmation that our entry-to-practice education and training meet standards acceptable to governments who act on behalf of civil society to protect students and patients. These accreditors, invariably “peers assessing peers,” summatively assess the skills acquisition methods which lead to the entrusting of graduates who are “registered, certified, or licensed,” depending on the strength of the language of the particular legislation in their state or province. In both cases, the core audience is just that, “civil society,” represented by elected officials who decide what is best for their constituents. If the equation, R + A = MAP(PF) works, one can assume that the legislative language and its accompanying regulatory framework and covenants have benefited from a commitment to grow the presence of the group in civil society. If it does not work, one can determine that the language has either been dulled by interest groups trying to contain professional formation (PF), or the regulators have lost sight of the vision and mission of the profession they serve and the needs of the community which has entrusted that role to them.
Fearing Regulators Is Professionally Disempowering
Reviewing the language of the legislation in question, one is left with several key questions…
- Who are the actual regulators (persons with what qualifications and what histories) affecting naturopathic professionals?
- Who are the accreditors (persons with what qualifications and what histories) affecting naturopathic educators?
- Does compliance with both of these truly generate sustainable professional formation (PF) characterized by equally sustainable mastery, autonomy, and purpose (MAP)?
As in every terrain, the roads across landscapes of higher education and health design/delivery scrutiny are fraught with signs, potholes, on-ramps, off-ramps, cul-de-sacs, law-abiding fellow travelers, and not-so-law-abiding fellows in passage, including some afflicted with road rage.
Let’s begin, though, with why we bother with professional formation in the first place. It isn’t, some say, just so that the AMA cannot sic investigators on those who would practice medicine (defined by the dominant group) without a license and compete with its members. It isn’t, others add, just so that we can benefit from 3rd-party reimbursement. It is that we wish naturopathic medicine to be considered a “profession” and that the profession will do good in the world. It is significant in this regard to distinguish between careerism and professionalism at the outset. The behavior of the biomedicine profession, in recent years, for example, with regard to how quickly it is assimilating holistic modalities, protocols, and practices into its repertoire, is seen by many as arrogant, careerist co-opting. The market is headed that way; so, let’s not miss the wave, since we own the water and the shore, anyway. Into that same reflective mix, it becomes less difficult to contrast the professionalism of a modestly compensated naturopathic doctor – going about his or her business of preventing disease – with the all-too-often economically-motivated behavior of biomedicine health systems salivating at the idea of more tests sooner and calling it “prevention.” When the complex skills, judgment, and patient-focused behavior of a healthcare provider are compromised by 3rd-party intrusions that guide service and relationship, we are not observing professionalism, but rather, commodified health services and careerism.
Whether we are talking about the legislation (which has the blessing of an elected civil body, such as a state legislature) or the accreditation standards (which have the blessing of a regional body or specialty body affiliated with the Department of Education), there are certain pivots which affect naturopathic legislation. In those common law traditions (case law, principally) that influence North American legislative practice, there is legislative law and there is common law; they exist in parallel. Most often, the legislation prevails over common law in situations where there is disagreement. Within legislative traditions, there are 2 main kinds: “acts” and “subsidiary legislation.” The key to MAP in a profession is to monitor closely any links between the 2 types. Who should do that monitoring is the voluntary medical association, guided and served by the legislative law and common law. In any case, subsidiary legislation “fills in the details not covered by the “Act” under which it is made.” It is in the detail and application of such statutory interpretation that tension arises most often. Indeed, it is in the subsidiary stuff, which shows up as regulations, local laws, by-laws, planning schemes, and rules, where tempers flare.
A particular manifestation of naturopathic “regulation,” though, may be fraught with landmines. For example, in several of the legislative frameworks we studied, reference to “license” or “registration” or “certification” is often confused by those terms not appearing elsewhere in a particular segment of the legislation itself. Very relevant questions, such as determining what “lawful authority” means, becomes crucial when hired laypersons interpret regulations. All too often the penalties for infractions are arbitrary, not articulated in point of fact in the legislation or in its subsidiary versions at all. Recourse, for example, is vague in most legislation affecting naturopathic professionals, and where a specific penalty is listed in a regulatory covenant, there is ambiguity about that penalty being fixed, maximum, or minimum.
Thus, naturopathic professionals in a variety of jurisdictions could resort to other legislation (sometimes called “Interpretation Acts”) or delve into case law to figure out whether to comply without challenge some edict or demand on the part of a regulator. Answers can be found in other legislation or in case law. But, finding those answers costs money and time, and puts the naturopathic professional at risk with a regulatory body most often composed of peers assisted by hired laypersons, and not by legal experts, although the latter may well be consulted (with the accompanying running meter). Things can get particularly complex if an individual piece of legislation affecting naturopathic doctors sits among other pieces of legislation which are germane. Where the issue boils down to conflict or inconsistency, the time and money consumed in unraveling the disagreement can discourage a challenge and, over time, contribute to a dilution of the formula:
R + A = MAP(PF).
Who Gets to Revise the Laws That Govern Us?
It is vital for the profession to remember, though, that despite the trust accorded to the regulators, subsidiary legislation or rules are made “under” an Act because the Act itself is what makes the subsidiary material possible. Every naturopathic “law” we reviewed made it clear who can generate subsidiary legislation and what the legislation can involve. When hired laypersons (that is, those serving the profession by appointment and not by election) are determined by members of the profession to not have its best interests at heart, it is entirely possible to revisit the “Act” and shift the levers of control. At one extreme, a court may remind the petitioner that some of the words causing the stir may not be part of the “Act” at all, but are headings and footnotes to individual sections, regulations, clauses, by-laws, or provisions. Even definitions may be relevant to a section of legislation and only applicable to that section. Interpretations of definitions apart from the context of the specific section keep the meter running for hours in potential challenges later, whether those changes are simple textual amendments or wholesale replacement of an entire Act. The latter is rare in our world, requiring another piece of subsidiary legislation (as in the recent shifts in the RHPA in Ontario) made under the Act itself.
At the other extreme, a civil proceeding to challenge an employee of a regulatory body could energize political action to revisit the statute itself and rework the language that made the offending behavior possible in the first place. Whatever we do, we will want to be familiar with the legislative piece as a whole, with an eye on giving effect to its purpose or object. There is nothing more annoying to a naturopathic professional than a lay bureaucrat interfering with his or her medical practice and predicating that interference on interpretations. Keeping in mind that we did not find any examples of legislation that, in its very language, explains why it was enacted, it is a good idea to encourage institutional memory and oversight among the profession and not rely on regulators to carry that wisdom.
We did find some least common denominators among the various “legislative” language we explored. For example, invariably, a substantial portion of the profession’s members was depicted as not engaged in activities under the jurisdiction of another division of government. Also frequent was language which referenced the primary objective of the treatments naturopathic professionals perform being about the promotion or restoration of health. Further, there was language frequently referencing risk of harm. Thus, the expression of legislative controls and privileges were predicated on the assumption of a substantial risk of physical or emotional harm to individual patients that could arise in the practice of the profession.
Following often on this element, in the various legislative examples we studied, was the notion of sufficiency of supervision. That is, the language of the legislation alluded to, by its content, a significant number of the members of this profession who, without the legislation, would not have the quality of their performance monitored effectively by supervisors in regulated institutions, or by supervisors who are themselves regulated professionals, or by regulated professionals who prescribe this profession’s services. Thus, the need for regulations based on primary legislation. Not surprisingly, we found recurrent reference to there being no alternative regulatory mechanisms, and that the profession was not already regulated effectively or would soon be regulated effectively under an alternative regulatory mechanism. And, finally, all the legislative examples we looked at referenced a body of knowledge which members of the profession had to call upon. That “codified knowledge” had to be distinctive and systematic in assessing or treating patients, and the core activities the affected professionals perform must constitute a clear, integrated, and broadly accepted whole. Also, not surprisingly, the education requirements for entry to practice showed up in the legislative detail, often with language contemplating the successful completion of a postsecondary program offered by a recognized educational institution.
Where That Leaves Us
While legislative platforms for naturopathic medical practice legitimize and augment the profession, the ensuing regulatory detail must encourage professional formation, rather than contain or dilute it. Many initial naturopathic laws kick-start a process which strengthens the profession across time. When the “regs,” though, get in the way of some fundamental principles and philosophical pillars for the medicine, the time may be ripe to revisit the language of the legislation itself.
 David J. Schleich, PhD, is president and CEO of the National University of Natural Medicine (NUNM), former president of Truestar Health, and former CEO and president of CCNM, where he served from 1996 to 2003. Previous posts have included appointments as vice president academic of Niagara College, and administrative and teaching positions at St. Lawrence College, Swinburne University (Australia) and the University of Alberta. His academic credentials have been earned from the University of Western Ontario (BA), the University of Alberta (MA), Queen’s University (BEd), and the University of Toronto (PhD).
David J. Schleich, PhD, is president and CEO of the National University of Natural Medicine (NUNM), former president of Truestar Health, and former CEO and president of CCNM, where he served from 1996 to 2003. Previous posts have included appointments as vice president academic of Niagara College, and administrative and teaching positions at St. Lawrence College, Swinburne University (Australia) and the University of Alberta. His academic credentials have been earned from the University of Western Ontario (BA), the University of Alberta (MA), Queen’s University (BEd), and the University of Toronto (PhD).
Reference
Maley, Y. (1987). The Language of Legislation. Language in Society, 16 (1), 25-48. Available at: http://www.jstor.org/stable/4167814.