Student Scholarship Honorable Mention
Nicole Gansemer
Jennifer Brusewitz, ND
Hidradenitis suppurativa (HS), also known as acne inversa, is a chronic, inflammatory skin condition primarily affecting the sweat glands. The primary lesions are painful, inflamed, deep-seated nodules in the intertriginous areas. The most common sites of involvement include the axillae, groin, inframammary folds, gluteal folds, and the perianal area. The practitioner may see comedones that are open or closed. Later in the disease progression, one might see double-headed or multi-headed open comedones (also known as “tombstone comedones”), and as the disease progresses, sinus tracts form and cause scarring. HS is relatively uncommon: it is estimated that only 0.1%-4.1% of people have this condition, with women being almost twice as likely to be affected than men.1 If left untreated, HS can lead to several complications, such as fistula formation, depression, infectious sequelae, and squamous cell carcinoma. Several concomitant diseases have been linked to HS, including metabolic syndrome, inflammatory bowel disease, and acne vulgaris.1,2
The Patient
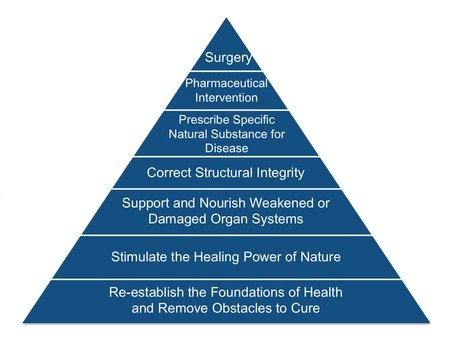
A 60-year-old obese woman presented to our clinic for management of hidradenitis suppurativa that began 5 years prior. The primary lesion originated on the vulva and was surgically drained – a common treatment for this condition. In the years following, the patient experienced deep, painful, inflamed nodules in the vulvar, perianal, gluteal and axillary areas, all of which spontaneously drained. During the previous 6 months, the patient had experienced 9 flares, most recently on the buttocks. Considering this patient’s history with HS, it was clear that her vital force was diminished. We began our consideration of the Therapeutic Order (see Figure 1): establishing foundations for health, supporting the body’s inherent healing mechanisms, and aiding the restoration of challenged organ systems.
Figure 1. Therapeutic Order
The patient’s health history was significant for obesity and various environmental and drug allergies, including severe reactions to corticosteroids, multiple antibiotics, and most metals. Triggers for an outbreak in this patient included stress and excessive sweating. When she came to us, she had just completed treatment for colorectal cancer and had been recovering from stoma reversal surgery. She presented with a scaling, pruritic, markedly erythematous rash that was present on the buttocks bilaterally. The rash was most prominent near the gluteal folds, with numerous deep-seated nodules surrounding the rash. She reported sleeping only 4-5 hours a night due to the stress of her surgery, and she was not exercising, under the recommendation of her surgeon. The patient previously tried antiseptics and antibiotics to treat HS outbreaks topically, including chlorhexidine 4% and mupirocin 2% ointment. The patient had already been utilizing naturopathic therapies as well, including homeopathy, immune-modulating herbal teas, poultices to help drain the cysts, and topical herbal tinctures to aid in wound healing. The patient was significantly distressed about the state of her health, appeared fatigued and expressed feeling hopeless due to her condition. We were interested in further optimizing our patient’s vital force, as we understood hidradenitis suppurativa could likely be influenced by stress levels, inadequate sleep, and disturbances in gut function.
Therapeutic Order-Directed Treatment
This patient had a complicated health history and a long list of allergies and sensitivities. With these challenges, it was imperative to consider the naturopathic Therapeutic Order in order to obtain positive outcomes. Our treatment recommendations for this patient included establishing a strong foundation for health, with adequate sleep and movement, guidelines for a gut-healing diet, and focused herbal support.
As a way to stimulate her vital force, the patient was encouraged to walk in green spaces at least 30 minutes a day, 5 days per week, and extensive motivational interviewing techniques were utilized to establish an achievable goal.3 There is ample research outlining the benefits of walking in nature, which include immune regulation, increasing parasympathetic tone, increasing oxygenation of tissues, and decreasing blood glucose levels.4 Stress was a major trigger of HS flares for this patient, so tonifying the nervous system was essential to her healing process. There have been numerous studies showing that forest bathing deceases salivary cortisol and symptoms of anxiety and depression.4 One Japanese study that evaluated heart rate variability (HRV) in 625 participants showed that walking in green spaces increased parasympathetic tone by 80%.5 Spending time in nature has also been shown to improve sleep, the lack of which was a major obstacle to cure in this patient.6
The patient reported sleeping only 4-5 hours per night because she was busy attending doctor’s appointments and volunteering with her church. Since she was recovering from cancer treatment and significant complications from surgery, we encouraged her to prioritize sleep. It was recommended that she sleep 8 hours per night, as adequate sleep has been shown to regulate the immune system, regulate the sympathetic nervous system, and modulate inflammatory responses.7 Ensuring that this patient got sufficient rest fostered a strong foundation of health and strengthened the vital force.
There are 2 main components of this patient’s diet that may have contributed to her flares of HS: dairy and refined carbohydrates. It is hypothesized that androgens play a role in the pathophysiology of HS.8 Furthermore, it is known that dairy raises both insulin levels and insulin-like growth factor (IGF-1).8 These 2 factors make androgen receptors more sensitive to circulating androgens in the body, thereby increasing skin keratinization, which leads to follicular plugging.8,9 Unfortunately, double-blind, placebo-controlled studies on the effects of diet on HS are lacking. However, in one informal study with 47 participants, 83% of patients improved on a dairy-free diet, and none worsened.8 Even with the lack of formal evidence, a dairy-free diet that is also low in refined carbohydrates could help reduce the hormonal effect on HS and aid in weight loss, which might prevent future outbreaks.
Golden Milk, a warm beverage made of high-fat milk, turmeric, and black pepper, was already a part of the patient’s nightly routine at the time of presentation to the clinic. Unsweetened, full-fat coconut milk was substituted for cow’s milk, since dairy was to be eliminated from the diet. Turmeric (Curcuma longa) is a vibrant yellow spice that is high in antioxidants. Turmeric has been shown to decrease inflammation, fight off infections, and prevent cancer.10 Curcumin, the active ingredient in turmeric, has been shown to inhibit lipoxygenase (LOX), cyclooxygenase-2 (COX-2), and inflammatory cytokines, actions which contribute to its anti-inflammatory effects.11 Curcumin is a lipophilic molecule with poor bioavailability. Combining turmeric with black pepper (Piper nigrum) in a high-fat base of coconut milk has been shown to increase bioavailability and absorption of curcumin.10 Since HS is an inflammatory condition with the possible sequelae of cancer, taking turmeric may help reduce the severity and longevity of flares and prevent the development of malignant sequelae.
The skin is our largest organ of elimination, so it can be inferred that patients with skin conditions, such as HS, are releasing toxins through the sweat glands. When the patient presented to clinic, she was drinking a daily immune-regulating tea daily for several months with no relief. Since the patient expressed that she enjoyed drinking tea every day, we switched the formula to a blend that would support liver detoxification pathways. The patient was prescribed an herbal tea with detoxifying herbs including burdock root (Arctium lappa), a potent herb that stimulates organs of elimination and aids in detoxification10; dandelion root (Taraxicum officinalis), to stimulate the liver and gallbladder and help eliminate toxins10,12; Oregon grape root (Mahonia spp), another potent alterative with antimicrobial properties that can correct intestinal dysbiosis and aid in the resolution of skin conditions10,12; yellow dock root (Rumex crispus), which is another mineral-rich alterative herb that both supports detoxification pathways and aids in small intestinal absorption10; ginger root (Zingiber officinalis), to help drive the herbs through the bloodstream10; and fennel seed (Foeniculum vulgare), orange peel (Citrus sinensis), licorice root (Glycyrrhiza glabra), and cinnamon bark (Cinnamonum verum) for flavor. The patient was encouraged to drink 1 quart of the tea daily.
Outcomes
At the 4-week follow-up, the patient reported that she had not experienced any HS flares since initiating the treatment plan. The patient was compliant with the treatment plan, which included increasing sleep to 7-8 hours nightly, walking at least 30 minutes 3 times weekly, eliminating dairy and refined carbohydrates from the diet, drinking dairy-free Golden Milk nightly, and ingesting 1 quart of Detoxifying Tea daily. The patient was encouraged to continue with the treatment plan. The rash on her left glute appeared much smaller than at the initial visit. The rash on the right had completely resolved. All of the nodules had completely resolved as well. The patient was upbeat and lively and was excited that she had not experienced any breakouts since the last office visit. She reported having significantly more energy and was highly motivated to continue the treatment plan and increase her exercise to 4-5 days per week.
At the 8-week follow-up, the patient continued to report being symptom-free despite being under high stress and engaging in activities that usually trigger flares. The remaining rash on the left glute had completely resolved and there were no visible signs of HS. The patient continued to stay motivated to improve her health and had a positive outlook on her well-being.
Since the patient’s HS has stabilized, the focus of treatment transitioned to weight loss for additional prevention. Weight loss is being addressed by further improving the diet and increasing the frequency, intensity, and duration of exercise. Overall, the patient has been extremely happy with the outcomes. She stated, “This is the best that I have ever felt.”
Conclusion
This case sheds light on the importance of using the Therapeutic Order to guide our approach to patients as well as the profound efficacy of treatments informed by the foundational principles of our medicine. This patient started her healing journey with a surgical procedure, the highest level of the Therapeutic Order, followed by numerous medications and natural substances to control symptoms. By taking a step back and considering the whole person, we were able to remove obstacles to cure, support detoxification pathways, and initiate therapies that stimulated and strengthened the Vis. Furthermore, by addressing foundations for health we were able to empower our patient and inspire her to take control of her well-being. The effect that this empowerment had on her constitution was increasingly more visible at each visit and played a key role in her healing journey.
References:
- Ingram JR. Hidradenitis suppurativa: Pathogenesis, clinical features, and diagnosis. Last updated April 30, 2018. UpToDate. Available at: https://www.uptodate.com/contents/hidradenitis-suppurativa-pathogenesis-clinical-features-and-diagnosis/. Accessed August 20, 2018.
- Woodruff CM, Charlie AM, Leslie KS. Hidradenitis Suppurativa: A Guide for the Practicing Physician. Mayo Clin Proc. 2015;90(12):1679-1693.
- Miller WR, Rollnick S. Motivational Interviewing: Helping People Change. 3rd ed. New York, NY: The Guilford Press; 2013.
- Hansen MM, Jones R, Tocchini K. Shinrin-Yoku (Forest Bathing) and Nature Therapy: A State-of-the-Art Review. Int J Environ Res Public Health. 2017;14(8): pii: E851. doi:10.3390/ijerph14080851.
- Kobayashi H, Song C, Ikei H, et al. Analysis of Individual Variations in Autonomic Responses to Urban and Forest Environments. Evid Based Complement Alternat Med. 2015;2015:671094.
- Morita E, Imai M, Okawa M, et al. A before and after comparison of the effects of forest walking on the sleep of a community-based sample of people with sleep complaints. Biopsychosoc Med. 2011;5:13.
- Irwin MR. Why sleep is important for health: a psychoneuroimmunology perspective. Ann Rev Psychol. 2015;66:143-172.
- Danby FW. Diet in the prevention of hidradenitis suppurativa (acne inversa). J Am Acad Dermatol. 2015;73(5 Suppl 1):S52-S54.
- Riis PT, Ring HC, Themstrup L, Jemec GB. The Role of Androgens and Estrogens in Hidradenitis Suppurativa – A Systematic Review. Acta Dermatrovenerol Croat. 2016;24(4):239-249.
- Tilgner S. Herbal Medicine: from the Heart of the Earth. 2nd ed. Creswell, OR: Wise Acres; 2009.
- Vaughn AR, Branum A, Sivamani RK. Effects of Turmeric (Curcuma longa) on Skin Health: A Systematic Review of the Clinical Evidence. Phytother Res. 2016;30(8):1243-1264.
- Godfrey A, Saunders P. Principles & Practices of Naturopathic Botanical Medicine. Vol 1. Toronto, Ontario: CCNM Press; 2010.
 Nicole Gansemer is a naturopathic medical student in her final year at the National University of Natural Medicine (NUNM) in Portland, OR. She has a passion for women’s health, environmental medicine, and complex chronic disease. Nicole furthered her botanical medicine studies at the Elderberry School of Botanical Medicine, and she has played an active role in NUNM’s Food As Medicine Institute, teaching community nutrition in the greater Portland area and in her hometown in rural Iowa.
Nicole Gansemer is a naturopathic medical student in her final year at the National University of Natural Medicine (NUNM) in Portland, OR. She has a passion for women’s health, environmental medicine, and complex chronic disease. Nicole furthered her botanical medicine studies at the Elderberry School of Botanical Medicine, and she has played an active role in NUNM’s Food As Medicine Institute, teaching community nutrition in the greater Portland area and in her hometown in rural Iowa.
***
 Jennifer Brusewitz, ND, is a 2000 graduate of the National University of Natural Medicine (NUNM). Dr Brusewitz currently practices in Portland, OR, and is academic faculty at NUNM and a clinical supervisor at NUNM’s teaching clinics. She also investigates, develops, and implements quality assurance standards in the university’s dispensary.
Jennifer Brusewitz, ND, is a 2000 graduate of the National University of Natural Medicine (NUNM). Dr Brusewitz currently practices in Portland, OR, and is academic faculty at NUNM and a clinical supervisor at NUNM’s teaching clinics. She also investigates, develops, and implements quality assurance standards in the university’s dispensary.