A Case Report and Literature Review
Student Scholarship – 2nd Place Case Study
Amanda Watters, NMS
Richard Barrett, ND
Otitis media with effusion (OME), or the presence of middle-ear effusion in the absence of acute signs of infection, is one of the most common childhood illnesses today. The prevalence of OME is 10% to 30% within the first 3 years of life, and a cumulative incidence of 80% at 4 years of age.1 Frequently, OME occurs following unrecognized or unresolved acute otitis media.1 The annual expenditure for treatment of otitis media in the United States totaled approximately $2.8 billion dollars in 2006.2 The most common complication associated with OME is conductive hearing loss, which can pose a significant barrier to a child’s language and speech development. The median loss of 25 decibels (dB) – the equivalent of wearing earplugs – may go undetected for extended periods of time until the child presents for medical attention or tests positive for hearing loss at school screenings.1
The American Academy of Family Physicians recommends initial management of a child with OME to consist of watchful waiting for 3 months from the onset of effusion (if known) or the time of diagnosis (if onset is unknown).3 Children become candidates for surgery under the following conditions: hearing loss of ≥40 dB; structural damage to the tympanic membrane or middle ear; OME of ≥4 months’ duration, with persistent hearing loss (≥21 dB); or a risk of speech, language, or learning problems, regardless of hearing status.3 In the absence of resolution during watchful waiting, the placement of tympanostomy tubes can allow for fluid drainage from the middle ear, and is recommended over myringotomy alone. While many studies following the management of OME have shown tube placement to improve hearing loss, especially during the first 6 months, several risks including recurrent infection, persistent middle-ear effusion, and several other late complications of tube placement, such as tympanosclerosis, focal atrophy, perforation, and cholesteotoma.4 If a child continues to experience further ear infections, he or she may undergo an adenoidectomy, with or without tonsillectomy, in an attempt to reduce recurrent episodes.5 For many parents, the risks associated with surgery to treat their child’s OME are far outweighed by the benefits. Surgery, however, is not the only option. Several different CAM therapies have been shown to be beneficial in the treatment of OME.
Alternative Therapies for OME
Allergy and upper respiratory inflammation are potential causative factors of Eustachian tube dysfunction and subsequent OME.6 Food allergies have the capacity to cause systemic inflammation, often extending beyond the gastrointestinal tract. The link between food allergies and OME is one that current research has only minimally explored. One study conducted by Nsouli et al followed the treatment of 104 children with recurrent OME.7 The children were evaluated through skin-prick testing, specific IgE tests, and food challenge; 81/104 presented with food allergies. Patients eliminated the suspect foods from their diet for 16 weeks, which led to significant amelioration of OME in 70/81 (86%), as determined through clinical evaluation and tympanometry. The suspected foods were then challenged through a reintroduction diet, which provoked a recurrence of OME in 66/70 (94%) of patients.
Food allergies often go undiagnosed. They can, however, be implicated as the primary cause of many chronic inflammatory conditions, including OME.8 Although cow’s milk has been identified as a common food allergen for children with OME,9,10 identifying an individual’s specific allergies can be far more effective in guiding dietary recommendations. The double-blind, placebo-controlled food challenge is the gold standard for identifying food allergies and sensitivities.11 This diagnostic procedure can be very time- and labor-intensive, so alternative testing methods are often performed. One option is to screen for IgG and IgE immune-mediated responses to food, although the role of IgG and IgE in food allergy is still debated in the literature.12 Another approach to resolving inflammation, besides the removal of allergens from the diet, is through appropriate nutritional supplementation. More specifically, essential fatty acids and probiotics have been shown to decrease symptoms associated with allergy.13
Physical manipulation has also been shown to be effective in treating OME. The endonasal technique is a form of Eustachian tube massage that supports the movement of blocked fluid.14 This treatment involves intraoral massage of the selected nasopharynx musculature, along with a tractional tug on the inferior tissues to mechanically open the blocked passageway.14
Autoinflation is another form of physical medicine that assists in clearing fluid from the Eustachian tube. For this technique, patients use a small 1-way valve to inflate a balloon with their nose, essentially equalizing the pressure and allowing for better drainage.15 Additionally, castor oil can be used topically to facilitate lymphatic circulation.16
Homeopathy is yet another treatment option for supporting the healing and resolution of OME. Although the highly individualized nature of homeopathy does not lend the modality to research very easily, preliminary studies have shown promising results for the treatment of OME with homeopathic medicine.17-19
Many of these treatment options have been studied independently; however, this case study is unique in that it demonstrates successful resolution of OME through a multifactorial approach.
Case Study
Concerned parents brought their 5-year-old son into a naturopathic clinic after he failed the hearing test at his yearly check-up. Prior to coming to the clinic, the young boy had experienced 1 case of acute otitis media and had a history of a chronically enlarged right tonsil for approximately 2 years. He presented to the naturopathic clinic after 2 ½ months of watchful waiting with his primary care physician, and an appointment had been scheduled with his ENT specialist for an adenotonsilectomy. The parents were running out of time before the scheduled surgery and were interested in exploring other treatment options.
History
Most recently the boy had experienced upper respiratory congestion following a fall and possible fracture to the left side of his nose, which lasted about 5 weeks. He had received all immunizations recommended by the CDC, starting at 6 months of age, he began eating solid foods at 1 year, and he was breastfed until he was 2 ½ years old. His past medical history was positive for atopy, which included allergic rhinitis and eczema. His diet consisted primarily of whole grains, fruits, vegetables, chicken, beef, nut butters, cheese, yogurt, rice milk, and tofu. Notable family history for the patient’s parents included asthma, eczema, and allergic rhinitis.
Physical Exam
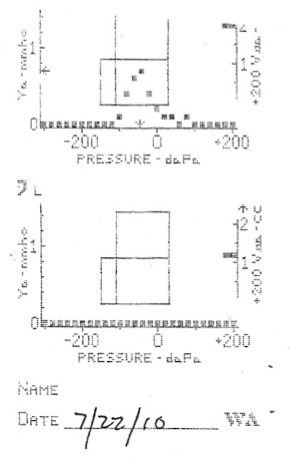
Examination of the patient’s left ear revealed a retracted, amber-colored tympanic membrane (TM) with no visible landmarks noted, and serous fluid behind the immobile TM. A tympanogram was used to assess the relative compliance and impedance of the TM, which gave an abnormal Type B reading, consistent with fluid behind the eardrum (Figure 1). In comparison, the right ear showed no signs of inflammation and was charted as a normal Type A. All landmarks could be visualized through the pearly gray, right TM. The light reflex could be clearly seen and the TM was mobile. Further physical examination exposed significant tonsillar lymphadenopathy. The left tonsil was given a grade of 4+, and the right tonsil was slightly less inflamed and was graded as 3+. No exudate was seen on either side. He also had mild anterior cervical and submandibular lymphadenopathy.
Figure 1
Diagnosis & Treatment
The patient was diagnosed with chronic OME and significant lymphadenopathy. The doctor suggested a possible etiology of food sensitivity, with consideration of the patient’s family history of allergies and hay fever. A serum IgG/IgE food sensitivity panel was ordered, and the results came back positive for a variety of foods. These included numerous beans such as kidney, lima, pinto, and soy, as well as almonds, asparagus, eggs, and whole wheat. The parents were advised to provide a strict diet for their son, avoiding all identified allergens for at least 6 weeks.
In addition to addressing his diet, the patient was given a daily supplement of essential fatty acids (including omega 3s and oleic acid) vitamins A, D and E, and probiotics. The parents were trained in-office on how to perform the endonasal technique on their son, and were instructed to do lymphatic massage with castor oil on his neck and shoulders. These treatments were to be completed once or twice per day. A homeopathic dose of Calcarea carbonica 12C was given sublingually daily for 1 month. Indications for Calcarea carbonica include purulent discharge, swelling of the tonsils, and loss of hearing.20
Follow-up
Two months later the patient returned to the clinic and tympanograms were taken. These images were consistent with the initial readings, so the patient was instructed to continue with all treatments and asked to return in 1 month. To provide additional support in clearing the Eustachian tube, a 1-way valve for autoinflation was ordered. The patient was instructed to implement this technique into his daily treatment regimen.
When the boy returned for his third visit 6 weeks later, he showed significant improvement. The parents reported compliance with the diet and treatment recommendations. Their son had started kindergarten and teachers reported no attention or hearing deficits. Physical exam revealed bilateral pearly gray, mobile TMs with visible landmarks. No erythema or exudates were observed, and there was no bulging or retraction noted. Tympanograms measured both ears as normal Type A (Figure 2). Tonsillar examination revealed a marked decrease in edema bilaterally. The right side was now graded as 2.5+, and the left was 1+. No erythema or exudates were observed. The patient was instructed to continue with dietary allergen avoidance and supplementation with probiotics and essential fatty acids. His parents were extremely satisfied with the improvement and were motivated to maintain treatment and diet modifications.
Figure 2
Discussion
Guided by the contemporary medical model, many young individuals undergo surgery to relieve Eustachian tube pressure caused by OME. Although tympanostomy tubes are shown to improve hearing and decrease the time spent with effusion during the first 6 months postoperatively, the improvement appears to diminish over time. By taking a less invasive approach, this patient was able to eliminate unnecessary systemic inflammation and treat his health problems at their root. This proactive approach occupies the middle ground between watchful waiting and surgery, and would perhaps best suit many patients. It is important to recognize the multidimensional quality of the treatment application. While numerous studies have looked at independent CAM therapies and found varying degrees of success, many medical practitioners in both the western and alternative medicine fields alike are beginning to recognize the value of a whole-system’s approach in order to effectively treat the individual. The treatments in this case were mutually supportive and therefore created a strong support for the patient’s body to heal itself. For example, the removal of allergens from the diet decreased mucus membrane inflammation, which then allowed for mechanical opening of the Eustachian tube through autoinflation and the endonasal technique. This case demonstrates a well-rounded treatment plan for OME, and supports the value of a holistic approach to medicine. This family gained a deeper understanding of their son’s specific dietary needs, and helped pave his way for a healthier future.
Conclusion
The success of this case strongly supports the need for further research regarding the relationship between food allergy and otitis media. A multifactorial study would be beneficial in addressing the added benefit of physical manipulation, such as autoinflation, as well as other supplemental treatment modalities. The identification of an individual’s specific food sensitivities, and the subsequent implementation of an allergen avoidance diet, has the potential to serve as an effective and non-invasive treatment for children with OME.
 Amanda Watters, NMS is a 4th year naturopathic student at National College of Natural Medicine. She graduated summa cum laude from the University of North Carolina at Greensboro, with an undergraduate degree in therapeutic recreation. Amanda loves working with children and hopes to someday open a naturopathic practice geared towards developmental and behavioral pediatrics.
Amanda Watters, NMS is a 4th year naturopathic student at National College of Natural Medicine. She graduated summa cum laude from the University of North Carolina at Greensboro, with an undergraduate degree in therapeutic recreation. Amanda loves working with children and hopes to someday open a naturopathic practice geared towards developmental and behavioral pediatrics.
Richard Barrett, ND is a professor at NCNM and a faculty investigator at the Helfgott Research Institute. He has been an active participant in NCNM’s NCCAM/NIH-funded R 25 grant to integrate evidence-based medicine in the naturopathic program. His research interests include clinical trials assessing naturopathic treatment protocols for ears, eyes, nose and throat (EENT) conditions, botanical medicinal applications, and naturopathic diagnostic techniques. Dr Barrett obtained his ND from NCNM in 1986 and earned the Certificate in Human Investigations from the OHSU School of Medicine in 2003. In 2012 he was named a Harvard Macy Scholar in the Program for Healthcare Educators. Dr Barrett has received several awards for excellence in teaching.
References
1. Lous J, Burton MJ, Felding JU, et al. Grommets (ventilation tubes) for hearing loss associated with otitis media with effusion in children. Cochrane Database Syst Rev. 2005;1(1):CD001801.
2. Soni A. Ear Infections (Otitis Media) in Children (0−17): Use and Expenditures, 2006. Statistical Brief #228. December, 2008. Medical Expenditure Panel Survey Web site. http://www.meps.ahrq.gov/mepsweb/data_files/publications/st228/stat228.pdf.
3. American Academy of Family Physicians; American Academy of Otolaryngology-Head and Neck Surgery; American Academy of Pediatrics Subcommittee on Otitis Media With Effusion. Otitis media with effusion. Pediatrics. 2004;113(5):1412-1429.
4. Kay DJ, Nelson M, Rosenfeld RM. Meta-analysis of tympanostomy tube sequelae. Otolaryngol Head Neck Surg. 2001;124(4):374-380.
5. Cheong KH, Hussain SS. Management of recurrent acute otitis media in children: systematic review of the effect of different interventions on otitis media recurrence, recurrence frequency and total recurrence time. J Laryngol Otol. 2012;126(9):874-885.
6. Alles R, Parikh A, Hawk L, et al. The prevalence of atopic disorders in children with chronic otitis media with effusion. Pediatr Allergy Immunol. 2001;12(2):102-106.
7. Nsouli TM, Nsouli SM, Linde RE, et al. Role of food allergy in serous otitis media. Ann Allergy. 1994;73(3):215-219.
8. Ramakrishnan JB. The role of food allergy in otolaryngology disorders. Curr Opin Otolaryngol Head Neck Surg. 2010;18(3):195-199.
9. Tikkanen S, Kokkonen J, Juntti H, Niinimaki A. Status of children with cow’s milk allergy in infancy by 10 years of age. Acta Paediatr. 2000;89(10):1174-1180.
10. Juntti H, Tikkanen S, Kokkonen J, et al. Cow’s milk allergy is associated with recurrent otitis media during childhood. Acta Otolaryngol. 1999;119(8):867-873.
11. Gushken AK, Castro AP, Yonamine GH, et al. Double-blind, placebo-controlled food challenges in Brazilian children: Adaptation to clinical practice. Allergol Immunopathol (Madr). 2013;41(2):94-101.
12. Bernardi D, Borghesan F, Faggian D, et al. Time to reconsider the clinical value of immunoglobulin G4 to foods? Clin Chem Lab Med. 2008;46(5):687-690.
13. Blazek-O’Neill B. Complementary and alternative medicine in allergy, otitis media, and asthma. Curr Allergy Asthma Rep. 2005;5(4):313-318.
14. Mootz RD, Bowers LJ. Otitis Media: A Conservative Chiropractic Management Protocol. In: Chiropractic Care of Special Populations. Gaithersburg, MD: Aspen Publishers; 1999:30-38.
15. Perera R, Haynes J, Glasziou P, Heneghan CJ. Autoinflation for hearing loss associated with otitis media with effusion. Cochrane Database Syst Rev. 2006 Oct 18;(4):CD006285.
16. Grady H. Immunomodulation through castor oil packs. Journal of Naturopathic Medicine. 1999;7:84-89.
17. Harrison H, Fixsen A, Vickers A. A randomized comparison of homoeopathic and standard care for the treatment of glue ear in children. Complement Ther Med. 1999;7(3):132-135.
18. Friese K, Moeller H, Ludtke R, Moeller H. The homoeopathic treatment of otitis media in children–comparisons with conventional therapy. Int J Clin Pharmacol Ther. 1997;35(7):296-301.
19. Jacobs J, Springer D, Crothers D. Homeopathic treatment of acute otitis media in children: a preliminary randomized placebo-controlled trial. Pediatr Infect Dis J. 2001;20(2):177-183.
20. Phatak S. Calcarea carbonica. Materia Medica of Homeopathic Medicines. 2nd ed. New Delhi, India: B. Jain Publishers; 1999:151-156.