FDA’s New GMPs Will Not Ensure Quality Products
Rick Liva, RPh, ND
Before I begin to outline the strengths and weaknesses of the new FDA Dietary Supplement Good Manufacturing Practices (GMPs), let me simply detail the problem that I think exists and the goal all clinicians should shoot for when choosing suppliers.
The Problem
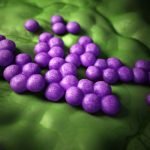
The problem is that a very large percentage of the 1200-1500 manufacturers of dietary supplements (retail or professional) in the U.S. do not test their raw materials or finished products; or the testing is so minimal that it is hugely deficient. Most rely on a “certificate of analysis” to assure their customers of authenticity, potency and freedom from contamination. That is what has been happening for years. A lot of substandard and contaminated product has been consumed by the end user because the product was never put through comprehensive quality verification testing.
The Goal: Verification Testing
Imagine there was no FDA, no GMPs, no regulation that anyone “must” follow to produce high-quality nutritional supplements. Imagine also that you were a member of a group practice with 1000 nutritionally oriented practitioners. Your dispensary sales were $75 million annually and many companies wanted an opportunity to sell their products to your practice because of the potential for a huge volume of sales. The practice had a very strict policy that every company it bought from must provide quality assurance verification of their products. Specifically, the requirement stated that all raw materials must be tested for authenticity (i.e., it is what it claims to be); potency; bacteria, yeast and mold; and a panel of contaminants (typically one would look for chemical solvent residue, herbicides and pesticides, aflatoxins and heavy metals in herbal raw materials, and solvent residue in non-herbal raw materials). In addition, all finished products must be tested for label claim potency. Finished product testing is a must to ensure that the manufacturing was done correctly so the final product had a homogenous and uniform composition and meets the label’s claim. The only way a company could even qualify to sell to your practice was to “prove” that it met these criteria. The company had to provide independent testing data as objective evidence. The practice had a designated person who would request this info from each company and was trained to evaluate the data provided. Armed with this knowledge, this “quality gate keeper” would only consider purchasing from the companies that met the criteria. If this was done by every practice we may not even need the FDA or GMPs. Alas, this is not the case. Not all manufacturers in this industry follow the rules, and so it requires government oversight.
The key is verification testing. If a company is not comprehensively testing its raw materials and finished products, there is absolutely no possible way to consistently achieve authenticity, potency claims and maximum freedom from contamination. You may be putting patients at risk if you buy from companies that do not perform comprehensive raw material and finished product testing.
The GMPs
GMPs are a set of rules and guidelines a manufacturer must follow to ensure sanitation, quality, safety, consistency; adequate documentation of all processes involved in manufacturing; that written procedures detail manufacturing and plant processes; personnel training; that products are made to meet their intended specifications; existence of a functional quality control department; correct laboratory practices; and proper distribution. The overall intent is to produce products that meet purity, strength and composition (uniformity) specifications.
Weaknesses of the New GMPs
The new FDA GMPs are a milestone for the industry, no question. However, there are three issues.
- The FDA is unlikely to enforce compliance with the rules due to lack of resources
- The new rules have so many holes, loopholes and unspecified areas that it is likely that many manufacturing companies will follow these rules in a diluted fashion.
- The suppliers of raw materials to the dietary supplement manufacturing facilities are “exempt” from the new FDA GMPs. The burden of quality assurance is on the manufacturer.
These three issues will breed massive confusion in the industry and for the consumer. In short, it is not possible to tell which companies are in compliance with the new GMPs without evaluation of each company’s quality practices and testing parameters.
There is a simple solution.
GMPs or not, it is up to each clinician to obtain “objective evidence and proof of quality” from each supplier before considering making a buying decision. In my next column I’ll discuss the “buying decision” and outline a simple tool each clinician can use to evaluate the quality practices (or lack thereof) of a supplier.
Major Highlights of the New GMPs
Overall Intent: The overall intent is to produce products that meet purity (authenticity and contamination), strength (potency) and composition (uniformity) specifications.
Who is subject to this? Anyone who manufactures, packages, labels or holds a dietary supplement.
What are the requirements to implement a production and process control system? A system of production and process controls must cover all stages of manufacturing, packaging, labeling and holding of the dietary supplement to ensure the quality of the dietary supplement.
Specifications that must be established?
- For any point, step or stage in the manufacturing process where control is necessary to ensure the quality of the dietary supplement.
- For each component used, component specifications must exist as follows:
- identity specification
- component specifications necessary to ensure the specifications for the purity, strength and composition
- limits on those types of contamination (the rule does not specify what types of contamination) that may adulterate the finished batch.
Note that this says manufacturers must establish written specs with acceptable limits and must ensure identity, purity, strength and composition.
Companies must determine whether the specifications as established are met. Before using a component, companies must:
- Conduct at least one appropriate test or examination to verify the identity
- Confirm the identity of other components and determine whether other applicable component specifications are met by conducting appropriate tests or examinations.
Companies must verify that the finished batch of the dietary supplement meets product specifications for identity, purity, strength, composition, and for limits on those types of contamination that may adulterate or that lead to adulteration of the finished batch of the dietary supplement. They must ensure that the tests and examinations used to determine whether the specifications are met are appropriate, scientifically valid methods.
What happens if established specifications are not met? Quality control personnel must reject the component, dietary supplement, package or label. No finished batch of dietary supplements may be released for distribution unless it passes identity and meets specs for purity, strength and composition.
Requirements that apply to laboratory methods for testing and examination?
- Companies must verify that the laboratory examination and testing methodologies are appropriate for their intended use.
- Companies must identify and use an “appropriate, scientifically valid method” for each established specification for which testing or examination is required to determine whether the specification is met.
Requirements under this subpart for written procedures? Companies must establish and follow written procedures for laboratory operations, including written procedures for the tests and examinations conducted to determine whether specifications are met.
Requirements for the laboratory facilities used? Adequate laboratory facilities must be used to perform whatever testing and examinations are necessary to determine that companies meet established specifications.
Requirements for laboratory control processes? Companies must establish and follow laboratory control processes that are reviewed and approved by quality control personnel, including:
- Use of criteria for establishing appropriate specifications
- Use of sampling plans for obtaining representative samples
- Components, packaging and labels
- In-process materials
- Finished batches of dietary supplements
- Product received for packaging or labeling as a dietary supplement (and for distribution rather than for return to the supplier)
- Packaged and labeled dietary supplements
- Use of criteria for selecting appropriate examination and testing methods
- Use of criteria for selecting standard reference materials used in performing tests and examinations
- Use of test methods and examinations in accordance with established criteria.
 Rick Liva, RPh, ND is the managing physician at the Connecticut Center for Health in Middletown. Dr. Liva is a founding member of the American Association of Naturopathic Physicians and past president of the Connecticut Society of Naturopathic Physicians. He has been involved in dietary supplements manufacturing since 1985 and is the president, CEO and director of quality control and quality assurance at Vital Nutrients, certified by NSF International and the Natural Products Association (NPA) in current Good Manufacturing Practices (cGMPs) for dietary supplements.
Rick Liva, RPh, ND is the managing physician at the Connecticut Center for Health in Middletown. Dr. Liva is a founding member of the American Association of Naturopathic Physicians and past president of the Connecticut Society of Naturopathic Physicians. He has been involved in dietary supplements manufacturing since 1985 and is the president, CEO and director of quality control and quality assurance at Vital Nutrients, certified by NSF International and the Natural Products Association (NPA) in current Good Manufacturing Practices (cGMPs) for dietary supplements.