Treating Prehypertension and Hypertension
Stephen Parcell, ND
Being male puts a patient at increased risk of getting cardiovascular disease (CVD) mostly because men get CVD approximately 10 years earlier than women. Increased risk begins at age 55 for men and 65 for women. Hormonal factors are hypothesized to be responsible for this difference in risk. Overall risk of hypertension does differ appreciably between men and women. Because hypertension is an important modifiable risk factor, one could argue that aggressive early detection and treatment in the male population could help to delay the progression of CVD.
The purpose of this article is to discuss the classification of prehypertension and hypertension and discuss how early detection and naturopathic treatment may delay the progression of CVD. Exercise is a well-known key component of therapeutic lifestyle changes, but will not be discussed here due to space limitations.
Prehypertension Defined
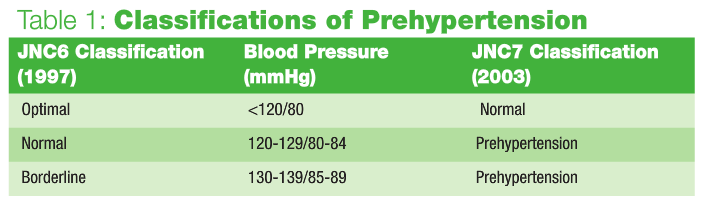
In 2003 the National Institutes of Health came out with a new category in blood pressure guidelines called prehypertension. Called the “Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure” (JNC7), it provides a new guideline for hypertension prevention and management. Prehypertension is an independent risk factor because it is closely correlated with risk of developing stage I and II hypertension. Patients with prehypertension also tend to have more CVD risk factors than normotensive individuals. Thus, patients with prehypertension are considered an ideal group for early intervention.
An estimated 70 million American adults have prehypertension. Prehypertension describes a range of blood pressure levels that previously had been categorized as normal or borderline: 120-139mmHg systolic and/or 80-89mmHg diastolic (see Table 1).
Prehypertension is not a disease category, and drug therapy is not recommended. The exception is individuals who also have diabetes or chronic kidney disease if lifestyle modification alone fails to reduce their blood pressure to ≤130/80mmHg. To reduce blood pressure, prevent or delay the onset of hypertension and enhance antihypertensive drug efficacy, the JNC7 recommends lifestyle modifications that include weight loss, a healthy diet, limited alcohol intake and aerobic exercise (30 minutes/day 6-7 days/week).
It is estimated that in patients with stage I hypertension and with additional cardiovascular risk factors, achieving a sustained 12mmHg reduction in systolic blood pressure over 10 years will prevent one death for every eleven patients treated.
Effective Dietary Advice
Numerous epidemiological studies and intervention studies agree that the following foods either protect against CVD and stroke or are associated with reduced risk of cardiovascular-related mortality:
- Whole grains: 2-3 servings/day
- Legumes (including soy protein, peas, lentils, peanuts, beans): 2-3 servings/day
- Wine/alcohol: 1-3 servings/day. For those without an alcohol problem I recommend one 4oz glass of dry white or red wine per day. For those who weigh more than 180lbs, two 4oz glasses may be consumed per day.
- Fruits/vegetables: 1-2 servings of fruit; 5 or more servings of vegetables
- Nuts: 1-2 servings/day. Almonds, Brazil nuts, cashews, hazelnuts, macadamias, peanuts (really a legume), pecans, pine nuts, pistachios and walnuts are good choices. Raw, unsalted nuts are preferable. Nut butters are also good. Almonds are the highest in fiber, and peanuts are highest in protein. Walnuts are the only nut with appreciable amounts of omega-3 fats.
- Fish: 2 servings minimum/week. I recommend fish oil supplements if at least two servings of fish per week are not consumed.
Of all the diets associated with lower blood pressure, only the Dietary Approaches to Stop Hypertension (DASH) diet has been studied extensively and shown to be effective as an intervention. The DASH diet is low in sodium (<2400mg/day) and high in magnesium, potassium and calcium. Traditional diets such as the “Paleo diet” also mimic this mineral profile. In the U.S., sodium intake is roughly 4,200mg per day for men. It is the pattern of low sodium coupled with high potassium, magnesium and calcium that is most effective, whereas individual mineral supplementation is not very effective.
The DASH diet is easily obtained online. My office uses a modified version of the DASH diet, which includes lower glycemic carbohydrate, healthier fats, whole grains and more fiber. We also customize it for those needing to lose weight, and conduct a bioimpedance analysis to monitor fat and muscle mass. I also give patients a shopping list to take with them to the store.
Dark chocolate administration has been shown to lower blood pressure and improve insulin sensitivity in humans, and a flurry of research on cacao as a constituent of dark chocolate and its effects on blood pressure, heart disease and diabetes has been conducted. Cacao beans contain more than 600 plant chemicals, including antioxidant phytochemicals, such as flavonoids, and high amounts of magnesium, which could explain a beneficial role in heart disease prevention. A bar of dark chocolate supplies the recommended daily allowance of magnesium as well.
Supplements
Arginine 3-6g/day Individuals with hypertension exhibit blunted epicardial and vascular dilation to endothelium-derived nitric oxide (EDNO) in the peripheral and coronary circulation. This likely contributes to altered vascular tone in hypertension. The amino acid L-arginine serves as the principal substrate for vascular NO production. Some studies demonstrate a beneficial effect of acute and chronic L-arginine supplementation on EDNO production and endothelial function. Numerous studies of IV-administered L-arginine in humans have shown that endothelial function is improved in patients with hypertension, hypercholesterolemia and diabetes. Preli et al. (2002) summarized the results of studies on the effect of oral L-arginine on the cardiovascular system in humans. In contrast to animal studies, the results from human studies have varied. Five of the 17 human studies showed no vascular health benefit from oral L-arginine supplementation. The remaining 12 studies demonstrated beneficial effect of oral L-arginine supplementation as evidenced by decreased platelet aggregation and adhesion, decreased monocyte adhesion or improved endothelium-dependent vasodilation. IV administration is more effective for acute blood pressure lowering.
A new sustained-release form of arginine shows promise. At 2.1g daily, sustained-release arginine lowered systolic blood pressure in 10 individuals who were hypertensive (mean systolic reduction of 11mmHg) while normotensives had a mean systolic decrease of only 0.22mmHg.
Magnesium Chelate (citrate, glycinate, malate) 200-500mg/day Some trials show that magnesium supplements (350-500mg/day) lower blood pressure. Magnesium appears to be particularly effective in people who are taking potassium-depleting diuretics, probably because these diuretics also deplete magnesium. Magnesium also has mild calcium channel blockade effects.
Coenzyme Q10 100-200mg/day (depending on bioavailability) I get good results with this one. CoQ10 has been primarily used for the treatment of congestive heart failure, but evidence also suggests utility in angina, diabetes and hypertension. Langsjoen et al. (1994) looked at the effect of CoQ10 on 424 patients with various cardiovascular diagnoses over an eight-year period to determine the effect of CoQ10 on cardiovascular diseases. CoQ10 was added to each patient’s medical regimen; patients were then monitored during regular clinic visits, where various cardiologic studies were performed. The dosage range used in this analysis varied from 75mg to 600mg per day with the aim of producing a whole blood level greater than or equal to 2.10mg/ml.
Patients were subdivided into six categories for the purposes of the analysis: those with idiopathic dilated cardiomyopathy, primary diastolic dysfunction, hypertension, ischemic cardiomyopathy, valvular heart disease and mitral valve prolapse. In general, the investigators observed symptomatic improvements in occurrence of chest pain, fatigue, dyspnea and palpitations. Overall, 58.2% (247) of patients demonstrated improvements. Patients with hypertension (P <.02) and mitral valve prolapse (P <.06) also showed some improvement in the left ventricular end diastolic dimension compared with baseline. Left ventricular wall thickness showed a significant improvement in all groups of patients except for patients with valvular heart disease (P <.05). This study, compared with others, enrolled a larger number of patients and had a longer follow-up period. Langsjoen et al. (1994) also reported a significant decrease in the number of cardiovascular drugs used: a 19% decrease in the use of digoxin, 51% decrease in use of beta blockers, 21% decrease in use of long-acting nitrates, 61% decrease in the use of antiarrhythmic drugs, 24% decrease in use of calcium channel blockers, 32% decrease in the use of angiotensin-converting enzyme inhibitors and 37% decrease in the use of other antihypertensive drugs.
Aged Garlic Extract 1-3 capsules/day, and Dietary Garlic Epidemiologic studies show an inverse correlation between garlic consumption and progression of cardiovascular disease, and evidence from clinical trials points toward garlic having a role to play in either preventing or delaying cardiovascular disease. However, more research is required. Since 1993, nine studies have been published on the effects of various forms of garlic on blood pressure, and six of those studies showed a reduction in blood pressure. A meta-analysis published in 2001 concluded that garlic has insignificant effects on blood pressure. Though effects on blood pressure are small, garlic has other proven cardiovascular benefits, including inhibition of platelet aggregation, mild hypolipidemic effects and reduction in oxidative stress.
Fish Oil 2g/day Omega-3 fats have mild effects on blood pressure but help modulate lipids, platelet function, blood viscosity and heart rhythm. Omega-3 intake is also independently associated with lower overall cardiovascular mortality.
Rauwolfia serpentina Rauwolfia is a source of reserpine, which depletes stores of serotonin and norepinephrine in the brain, adrenal medulla and other tissues, and reduces the reuptake of catecholamines by adrenergic nerve terminals. The drug binds tightly to catecholamine storage vesicles in the adrenergic neuron, eventually destroying these vesicles so that the terminals cannot concentrate or store norepinephrine or dopamine. This process also occurs in vesicles that store serotonin. The result of reserpine’s effects on biogenic amines is a decrease in sympathetic tone, with a subsequent decrease in peripheral vascular resistance and a lowering of blood pressure and bradycardia. Because the therapeutic index is narrow and the potential for interactions and side effects is significant, I use this agent only as a last resort.
Fish Peptides and Milk Peptides Various peptides from “Katsuo-bushi,” a Japanese traditional food processed from dried bonito, have been studied for their ability to inhibit angiotensin I-converting enzyme (ACE). Effects appear to be close to the ACE inhibitor captopril. To my knowledge, no studies have yet been done on humans. Other peptides from milk, sesame, sake and blue mussel have also been studied.
Milk peptides have support from a number of human clinical trials. Fermentation of milk by the microorganism Lactobacillus helveticus LBK-16H or hydrolysis of casein by protease of Aspergillus oryzae generates the tripeptide casokinines (Val-Pro-Pro and Ile-Pro-Pro). These peptides inhibit ACE. Daily intake of these peptides decreases the blood pressure in hypertensive patients similar to that seen by pharmacologic ACE inhibitors. The same precautions and contraindications must be used as with any ACE inhibitor, especially monitoring of renal function.
Numerous natural therapeutics exist for treating prehypertension and hypertension. Most of these measures may be used in combination with pharmacologic agents. Achieving even modest reductions in blood pressure (10-12mmHg) can significantly reduce cardiovascular mortality. Men with prehypertension should be screened for other CVD risk factors and treated early to delay the progression of CVD. A DASH or modified DASH diet coupled with a customized supplement plan provides very good clinical results for lowering blood pressure.
Causes of Hypertension
Identifiable
- Sleep apnea
- Drug-induced or related causes (see list further below)
- Chronic kidney disease
- Primary aldosteronism
- Renovascular disease
- Chronic steroid therapy and Cushing’s syndrome
- Pheochromocytoma
- Coarctation of the aorta
- Thyroid or parathyroid disease
Resistant Hypertension
- Improper blood pressure measurement
- Volume overload
- Excess sodium intake
- Volume retention from kidney disease
- Inadequate diuretic therapy
- Identifiable causes of hypertension
Drug-Induced or Other Causes
- Nonadherence
- Inadequate doses
- Inappropriate combinations
- Nonsteroidal anti-inflammatory drugs (NSAIDS); cyclooxygenase 2 inhibitors
- Cocaine, amphetamines, other illicit drugs
- Sympathomimetics (decongestants, anorectics)
- Oral contraceptives
- Adrenal steroids
- Cyclosporine and tacrolimus
- Erythropoietin
- Licorice (including some chewing tobacco)
- Select over-the-counter dietary supplements and medicines (e.g., ephedra, bitter orange, caffeine)
 Stephen W. Parcell, ND earned his doctor of naturopathic medicine degree at Bastyr University, and performed his premedical studies at the University of Vermont. He has a background in medical research, especially in CAM. Dr. Parcell worked at the American Institute for Biosocial and Medical Research, has co-authored National Institutes of Health (NIH) research grant proposals, and recently authored a chapter for a book entitled Biochemical and Nutritional Influences on Pain. He is a member of the American College for the Advancement of Medicine (ACAM), the American Association of Naturopathic Physicians (AANP) and the Colorado Association of Naturopathic Physicians (CANP). Dr. Parcell specializes in men’s health, cardiology, clinical nutrition, sports medicine and anti-aging medicine in Boulder, Colo.
Stephen W. Parcell, ND earned his doctor of naturopathic medicine degree at Bastyr University, and performed his premedical studies at the University of Vermont. He has a background in medical research, especially in CAM. Dr. Parcell worked at the American Institute for Biosocial and Medical Research, has co-authored National Institutes of Health (NIH) research grant proposals, and recently authored a chapter for a book entitled Biochemical and Nutritional Influences on Pain. He is a member of the American College for the Advancement of Medicine (ACAM), the American Association of Naturopathic Physicians (AANP) and the Colorado Association of Naturopathic Physicians (CANP). Dr. Parcell specializes in men’s health, cardiology, clinical nutrition, sports medicine and anti-aging medicine in Boulder, Colo.
References
Grassi D et al: Short-term administration of dark chocolate is followed by a significant increase in insulin sensitivity and a decrease in blood pressure in healthy persons, Am J Clin Nutr 81:611-4, 2005.
Cylwik D et al: L-arginine and cardiovascular system (review), Pharmacol Rep Jan-Feb;57(1):14-22, 2005.
Preli RB et al: Vascular effects of dietary L-arginine supplementation, Atherosclerosis 162(1):1-15, 2002.
Miller A: The effects of sustained-release-L-arginine formulation on blood pressure and vascular compliance in 29 healthy individuals, Altern Med Rev Mar;11(1):23-9, 2006.
Langsjoen H et al: Usefulness of coenzyme Q10 in clinical cardiology: a long-term study, Mol Aspects Med 15(suppl):S165-S175, 1994.
Rahman K, Lowe GM: Garlic and cardiovascular disease: a critical review, J Nutr Mar;136(3 Suppl):736S-740S, 2006
Ackermann RT et al: Garlic shows promise for improving some cardiovascular risk factors, Arch Intern Med 161:813-24, 2001.
Fujita H, Yoshikawa M: LKPNM: a prodrug-type ACE-inhibitory peptide derived from fish protein, Immunopharmacology Oct 15;44(1-2):123-7, 1999.
Nussberger J: Blood pressure lowering tripeptides derived from milk protein, Ther Umsch Mar;64(3):177-9, 2007.