PHRANQ D. TAMBURRI, NMD
Throughout the world, news of exciting advancements in prostate cancer (CaP) – which I hinted at last year – has been limited due to the coronavirus. Nevertheless, there have been exceptional developments in prostate imaging, eg, the currently experimental PMSA and the new, still-in-development, Micro-RNA testing that physicians will hopefully have access to by next year. Furthermore, there have been significant stirrings among urologists regarding what constitutes an acceptable “aggressive” prostate carcinoma. For instance, similar to Pluto being downgraded from full “planet” status, histopathologists are seriously considering reclassifying Gleason 6 (the lowest legal aggression level) cancer as “something else.” As research and medical conferences begin to reopen next year, coupled with the pronounced advancements stated above, urologists are noticing a profound positive shift in how prostate cancer will be managed in the near future. Please do not act on this information clinically yet, but it’s very exciting, not only for CaP specialists, but also for our patients and their families going forward.
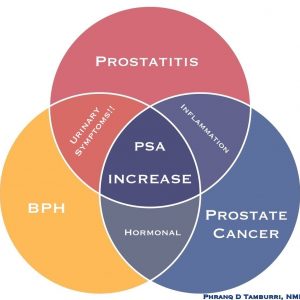
For the purposes of this article, I am extremely excited to share with the naturopathic community, and especially those who have followed these annual NDNR updates for the last 13 years, my Prostate Assessment Venn Diagram – the result of almost 20 years of patient consults that have enabled me to evolve differential strategies and identify patterns (Figure 1). Utilizing this tool, the practitioner can quickly focus on the most likely cause, or causes, of an elevated prostate-specific antigen (PSA) while concomitantly being guided toward appropriate treatment strategies. In fact, I have a laminated version of this chart in my consultation room, where I review it with every new patient. I myself did not recognize how useful it was until patients kept asking for copies or taking pictures of it with their phone.
The Need for a Proper PSA Assessment Tool
The experienced clinician quickly encounters complexity and confusion when trying to interpret an elevated PSA. Cynically speaking, the conventional physician does not find this matter as complicated, since the solution usually begins with a reflex biopsy of the prostate. Determining why a PSA is elevated is only a concern for the urologist after his or her liability risk has been reduced with a biopsy. To be fair, the prostate biopsy is quickly becoming more refined in both safety and accuracy in detecting carcinoma; however, it is still a procedure that most men wish to avoid if not deemed necessary. No patient (with their sanity intact) wants a biopsy, especially if it’s unnecessary. The only hope for these patients is often the naturopathic integrative physician, who is then stuck with this high liability decision. This Venn diagram assessment tool will greatly help you in this endeavor by more clearly separating out the causes of the elevated PSA while concomitantly illustrating for both you and your patient the proper way to rule out cancer before a biopsy is possibly needlessly performed.
The “Real” Reason to Avoid Biopsy
The typical patient concern of “tracking/seeding” a CaP outside the gland during a biopsy has not been shown to have much merit. After all, considering the explosion in routine biopsies performed over the past decades, if cancer was routinely spread throughout the body as a result of this procedure, we would have observed a commensurate increase in prostate cancer metastasis and mortality over those same decades. But we have not. Instead, CaP mortality has markedly decreased since routine biopsy was introduced. Of course, these biopsies have led to a proportionate explosion in diagnosed indolent (low-aggression) prostate cancers, the treatments for which often result in numerous serious post-surgical/radiation side effects, such as incontinence and erectile dysfunction. Whether this high chance of side effects is worth the low chance that a man will die from the condition is an exceptionally complicated and personal determination that has been outlined in prior NDNR issues in this series.
Although a biopsy-induced spreading of a cancer outside the prostate is considered very low, it is nonetheless conceivable that a biopsy could spread CaP cells throughout the prostate itself. This is an important distinction. Although this form of “seeding“ is not what most anxious patients are concerned about, this localized seeding can still cause difficulty when treating such an embedded cancer naturopathically, since there are now more CaP cells to treat within a now-damaged (inflamed) gland.
CaP contained within the gland does not necessarily lead to metastatic disease; I too once had concerns over this possibility. This is admittedly a loaded topic, which has also been discussed in previous NDNR updates.
Self-Fulfilling Prophecy
Instead, the most profound problem I face with a biopsy, whether cancer is officially diagnosed or not, is that the damage created by the procedure can produce an elevated PSA that causes the very cancer “scare” that the urologist was looking for! In other words, the physician creates his own “reality” by attributing a post-biopsy elevated PSA to his reflex cancer concern. What is especially dubious – and this typically occurs unknowingly by the urologist – is that this forces a repeat biopsy if cancer was not determined, yet reinforces their alarming concern, especially if it was.
This is exceptionally important to understand, since the majority of elevated PSA values under 10.0 ng/mL point to inflammation. This means that the PSA is likely elevated as a result of a direct prostatitis, or indirectly as a result of a systemic inflammatory process (diabetes, trauma, autoimmune flare-up, etc).
And, if this inflammation as the cause is not identified before the reflex biopsy, then what effect do you think subjecting a gland to 12 needles through a patient’s rectal wall, coated with bacteria, will further do to an already inflamed prostate? The effect can be extensive acute inflammation, with some cases lasting years. To reiterate this key point, if even an indolent carcinoma is discovered in the slightest amount, understand that both the prior and future PSA values will likely be attributed to this new diagnosis, whether warranted or not.
Please recognize that I am not, nor was ever, opposed to a prostate biopsy as long as due diligence was done in first explaining the PSA. However, I have unfortunately witnessed first-hand, after following thousands of PSA-tracking assessment cases, this very medical version of Three’s Company, with Jack, Chrissy, and Mr Roper, where the PSA is being understandably misunderstood – just not as amusing! Although I do not blame the urologist for this growingly apparent loophole, it is certainly a function of a broken system. The pressure from liability concerns, coupled with the stereotypical 5-minute insurance visit, forces the biopsy to be performed before conducting a very lengthy and complicated prostatitis determination.
One must understand the position of the urologist. He can be sued for missing a cancer diagnosis, which he can confirm quickly and legally with a biopsy. Conversely, he will likely not be sued for missing a prostatitis whose determination may require multiple visits containing uncomfortable questions and multiple treatments and testing. Biopsies simply pay more, have lower liability, there is no need to speak with the patient, and the legally acceptable diagnosis is quick. From within their conventional fishbowl, this makes sense.
It was precisely this patient quandary and urologist quagmire that illuminated the need for an effective analysis of their patient’s PSA – one that could be accomplished in a few weeks, keep the patient safe, keep the doc’s liability low, and also offer a treatment strategy that attacks a suspect cancer while really helping to unmask the cause of the PSA.
We will first explore my Venn diagram, and then conclude with specific treatment steps you should use in your practice when presented with an elevated PSA in a patient.
Understanding the Venn Diagram
1. The 3 Main PSA Pathologies
Although there are exceptions, the 3 dominant causes of a PSA increase are prostatitis (colored in red for inflammation), benign prostatic hyperplasia (BPH, colored in yellow for moderate), and CaP (colored in traditional blue) (see Figure 1). Also note that the likelihood of the PSA elevation being due to each pathology is in that same order. In other words, prostatitis is most common, followed by BPH, and CaP is the least likely as long as a patient’s unexplained elevated PSA is under 10.0. Although CaP must be your first concern for liability reasons, if you are playing the “Las Vegas odds,” you should put your chips on prostatitis.
[Insert Figure 1; jpg in Dropbox]:
Figure 1. 3 Main PSA Pathologies
2. Pathology Considerations
Although the practitioner reading this will likely be aware of these distinctions, when I explain this diagram to patients in my office, I expand on it in the following ways:
- Prostatitis does not necessarily mean an infection. It is an inflammation. In fact, only 10% of prostatitis cases turn out to be infectious.1 As stated above, the majority of a proper PSA investigation is determining the non-bacterial underlying cause of a prostatitis. We will soon see how much more complicated this becomes when/if a biopsy is involved.
- BPH does not mean a “big” prostate. The “H” in BPH stands for “hyperplasia,” not “hypertrophy.” A hyperplasia simply refers to an increased production of cells. Although the tendency is for the prostate to increase in volume, it is often more likely to become more dense as these cells are packed together. This is why 5-alpha reductase inhibitors, such as finasteride, are best for a very large prostate (they shrink the gland), while alpha-1 blockers, such as tamsulosin, are best for the dense variants that cause, ironically, more urination symptoms (they relax the muscles around the prostate). This is due to the compression on the prostatic urethra. The point is that, although each form of BPH can cause varying degrees of urination symptoms, they both involve an increase in PSA-producing cells.
- In the vast majority of cases, CaP is not fatal, especially if diagnosed as the most common Gleason 6. Although most men are aware of this point by the time they reach my office, it often bears repeating for their concerned partner who is typically sitting beside them.
- Another new CaP research highlight I mention to my patients is that, to date, over 1000 different variants of prostate cancer have been discovered! This statistic, a result of the continuing genome breakdown in this disease, was presented at the 2018 Prostate Cancer Research Institute’s 2018 research summit. Although this finding may not be surprising to the integrative practitioner, as we view disease as individually as we view our patients, the urologists in the audience were aghast, since they’re accustomed to a simple CaP classification system, such as the Gleason score simply being between 6 and 10. In fact, at this conference the presenter half-jokingly stated that his colleagues were starting to think, “Perhaps it’s time we just stop counting them!” The point here is that prostate cancers are comprised of individual mutations that are as different from each other as human beings, all having their own quirks and producing varying amounts of PSA. A one-size-fits-all classification favors the medical system but not necessarily the patient.
3. The Venn Overlap
Lastly, we arrive at the true value of this diagram. Noting where these 3 PSA pathologies overlap significantly helps practitioners refine their differential while also hinting at initial treatment strategies (Figure 1).
- Prostatitis and CaP share the property of inflammation. As stated above, prostatitis is, by definition, inflammation. But keep in mind that cancer is also inflammatory! This means that, technically, an additional cause of an inflamed prostate can be an embattled immune system’s response to CaP. I have seen countless heightened color Doppler blood flow imaging tests, performed at my office on a patient with a previously diagnosed CaP, that indicate high metabolic activity and an inflammatory process. In fact, asymmetric focal blood flow provides a differential for prostatitis or CaP, not BPH (which typically is symmetrical).
- In addition, CaP and prostatitis share similar PSA kinetics, in particular a high PSA velocity over 1.0 ng/mL per year and an elevated PSA density over 0.15. In general, both of these inflammatory conditions can cause a rapid increase in the PSA, whereas a PSA elevation associated with BPH tends to be slow, steady, and commensurate with the size of the gland.
- Finally, prostatitis and CaP equally share the same treatment strategy, which is high-intensity anti-inflammatories. Liposomal curcumin, fish oil, contrast hydrotherapy, and even Sitz bath, are just some of the powerful methods that are appropriate for either problem.
- CaP and BPH share the trait of an underlying hormonal problem. This is a much larger and involved topic than this summary article can explore. However, in general, each of these conditions seems to be influenced by an imbalance between the primary sex hormones (ie, testosterone and estrogen) and their intermediaries, such as dihydrotestosterone (DHT). As a consequence, notice how the treatments for both are very similar: They often involve reducing estrogen and DHT, while stabilizing or possibly increasing testosterone and progesterone levels.
This is why, to put it extremely simplistically, if a patient wants to “shrink his prostate,” he is put on 5-alpha reductase inhibitors (eg, finasteride or Serenoa repens); similarly, if a patient wants to “shrink his prostate cancer,” he too is put on 5-alpha reductase inhibitors (eg, finasteride or Serenoa repens) or complete androgen deprivation therapy (eg, bicalutamide).
Unfortunately, this has led to saw palmetto (Serenoa) becoming a cliché. Please note why it is important to identify the primary source of the PSA increase, since countless patients are being put on prostate formulas that are basically saw palmetto and African pygeum. These common herbs are meant for hormone modulation; yet, as stated above, the most likely cause of the PSA elevation is inflammation. You need to use the right tool for the job so that you don’t waste your patient’s money with these “grab bag” prostate formulas.
And now we arrive at the keystone…
- BPH and prostatitis share the trait of urinary symptoms. This last point cannot be stressed enough!
You see, if the problem is CaP and the PSA is under 10.0 ng/mL, then the suspect CaP is likely relatively small within the gland. This means that such a cancer is insidious; so, other than an elevated PSA that is concerning his physician, the patient is otherwise completely unaware that he has a problem. In contrast, BPH and prostatitis (especially if both are present) can cause myriad urination difficulties, such as frequency, urgency, incomplete voiding, and especially nocturia.
I highly recommend that every practitioner utilize the American Urological Association (AUA)’s 7-question urination symptom quiz with each of your prostate patients.2 A PDF of the quiz can easily be downloaded. The point is that whenever a man has an elevated PSA, I absolutely want to see urinary symptoms. In fact, the more symptoms, the better! Looking at the Venn diagram, it should now become obvious as to why. If a patient has an elevated PSA but no symptoms, then where is the PSA elevation coming from? If BPH and/or prostatitis are not present, then the differential has “collapsed” and I am unfortunately forced to place CaP at the top of my differential diagnosis. My medical students will remember my mantra that, for the patient’s own benefit, “Dr Tamburri loves to see ‘peeing problems’”!
Art of the Interview
With regard to this symptom consideration, I wish to add a special note regarding the psychology I use when collecting this information during the consultation.
Although I am not playing games with my patient, my detailed interview with a new patient has become strategic in terms of what and when I ask questions. For instance, reconsider asking a patient about urinary tract infections if his partner is sitting right next to him. With regard to the importance of determining a proper urination symptom profile, my patient is given the AUA’s symptom score during his vitals so that I always have the objective evaluation in front of me.
However, I never reveal the correlation between the lack of urinary symptoms and CaP until the end of the consultation. Instead, I typically reveal it during the last part of the Venn diagram explanation, as I just did above with you, the reader. Why? Because you never want to bias the patient’s description of their urination symptoms by telling them about this correlation too early. Always listen first. Some patients start right off complaining about their urination problems, such as how many times they wake up at night and wake up their wife. Sometimes, as they lament how they can’t hold their urine for more than 30 minutes, they don’t even seem to care about their PSA. Other men like to proudly gloat about how healthy they are, how many marathons they run, how virile they are. Some will deny problems the more you press them. Sometimes pride in one’s health or being accompanied by a new sexual partner during the consultation can influence their response. Nevertheless, the presence or absence of these symptoms is a critical factor in the PSA differential, so it is critical that you acquire an unbiased description from your patient without them overthinking it. And, trust me, if they realize that you are looking for symptoms so that you can tell them “You don’t have cancer,” they will suddenly describe “forgotten” episodes of “frequency” because they drank a 6-pack during the Super Bowl!
Differentiating BPH from Prostatitis
Prostatitis symptoms tend to be due to inflammation and swelling, whereas BPH symptoms are due to compression upon the urethra. As such, each can superficially yield apparently similar frequency symptoms. However, prostatitis frequency, being inflammatory in nature, typically results in an empty bladder because the prostate is “vomiting” out the urine whenever it is produced. BPH frequency, in contrast, results from urine retention. Urethral compression results in frequent micturition because the weight of the new urine is needed to push out an equal amount below it through the constriction. Over time, this constant “topping off” of urine in and out results in frequency, but is also often associated with a sense of incomplete voiding and urine retention.
Of course, your patient can have real “fun” if these 2 problems coexist. The typical scenario is a BPH-induced urine retention that subsequently leads to a urinary tract infection, which, in turn, can cause either an acute or chronic prostatitis. Don’t forget that unrecognized urine retention for years can further lead to interstitial cystitis.
Although this combination diagnosis is more complicated to treat, such a compiling of problems will certainly help explain the worrisome PSA kinetics that typically brought your patient to see you in the first place. Yet, incredibly, I have been referred many patients with this obvious situation, who were set up for a biopsy by their “5-minute” urologist.
PSA Assessment Strategy & Treatment
Finally, using the Venn diagram as a visual guide, here is my recommended differential strategy that I initiate with a new patient with an elevated PSA:
- Talk to your patient! Once I have a good rapport with my patient, about 35% of the time I can figure out the case with a thorough discussion, albeit sometimes with embarrassing questions.
- Check the urine for infection. This increasingly includes microscopic testing for yeast, which is missed more times than you would believe.
- Determine if/how much post-void urine retention is present. A 2-second cheap bladder scan by the urologist is the easiest way. Although that is one function of the trans-rectal ultrasound of the prostate (TRUSP) imaging that I conduct in my own office, I have had a few patients purchase their own bladder scan machine (fairly cheap on eBay) and run it on themselves.
- If possible, try to have an ultrasound/MRI of the prostate to at least secure a proper volume. This allows the calculation of the important PSA Density (PSA/gland volume) and will help confirm what type of BPH may be present. There is much more significant assessment data that can be gleaned on prostate imaging, such as suspect cancer lesions, inflammatory patches, etc, but these have been discussed in prior NDNR issues.
- Digital rectal exam (DRE) must be performed properly to help differentiate between the 3 PSA pathologies: a) Hard nodules or ridges, especially when they correlate on imaging, would be suspect for CaP; b) An extra firm, symmetric, and smooth gland would suggest BPH. A firmer gland often suggests the more dense variant of BPH, with more urethral compression (and concomitant symptoms); c) A gland that is slightly soft, boggy, or warm will suggest an acute prostatitis. Unfortunately most prostatitis tends to be a low-grade chronic form, with clear urine, and thus less symptomatic and harder to identify.
- With the above 5 target strategies, you should easily have at least a target pathology (BPH and/or prostatitis) to begin treating and subsequently retest to confirm a lowered PSA. Always start with opening the bladder. If the PSA is very worrisome, than I typically start with tamsulosin, since it has a very low short-term side-effect profile and should clear the bladder within only days. Then hammer the prostate with anti-inflammatories, obviously targeting the assumed source of the inflammation. The best part is that, as the Venn diagram illustrates, the treatments you will use for BPH and prostatitis – hormone influencing and anti-inflammatories, respectively – are both the same treatments and strategies you would use if this becomes a cancer case! If you have read this far, then consider this your “prize.” Understand that your patient will be very anxious about treating “the cancer” immediately, even though he may not even have a diagnosis of it. Although you just met him today, he has most likely been anxiously pondering whether he has cancer for weeks or months until he could see you. Although you are approaching this elevated PSA with an exceptionally logical differential to keep him from an unnecessary biopsy, the patient (and often his wife) will not feel comfortable leaving without “active cancer treatments.” The Venn diagram strongly explains to the patient that we are addressing “the cancer” if it exists, yet we are more importantly both determining and treating any other cause of the elevated PSA along the way. Patients are typically very satisfied with this explanation, which also helps with compliance.
- As you wait for these treatments to work and for the PSA to decrease, I strongly advise the addition of an FDA-approved RNA molecular prostate cancer test. Prior versions have been the PCA-3 and the SELECT MDX (discussed in prior NDNR articles); however, the most current is the new EXO DX. Remember that these modern tests are independent of the PSA, are about 75% reliable in detecting an aggressive prostate cancer, and can give you and your patient both an anxiety and liability buffer from the “biopsy happy“ urologist until, hopefully, the PSA is under control or properly assessed.
- IMPORTANT: If you decide to track your patient’s PSA over time, as it continues to increase or is over 10.0, then you must be agile in the use of PSA kinetics such as the PSA velocity, PSA density, PSA pattern, the % free PSA, and the often-forgotten prostatic acid phosphatase (PAP).
- Lastly, encourage your patient to educate himself. Apologizing for any perceived self-promotion, journal articles such as this one can greatly help your patient understand what you are doing. The Prostate Cancer Research Institute (PCRI.org) is another fantastic information resource that even holds annual conferences for both urologists and informed patients. And, of course, I still highly recommend the classic book, Invasion of the Prostate Snatchers, to all patients as they embark on this sometimes lengthy and tedious prostate assessment journey.
Conclusion
CaP rule-out and PSA assessing is admittedly a complicated affair, but truly becomes more manageable and transparent with experience and time. Hopefully, this Venn diagram, which I use every day, will help you to better compartmentalize your strategies and approach. Finally, understand that the complexity of this disease is not suited for a top-down myopic insurance/protocol medical system. To reasonably understand what is behind an elevated PSA takes time and understanding from both you and, especially, your patient. Your patient must become your partner in this journey, through education, communication, and this trust… the purview of naturopathic medicine.
References:
- Coker TJ, Dierfeldt DM. Acute Bacterial Prostatitis: Diagnosis and Management. Am Fam Physician. 2016;93(2):114-120.
- Barry MJ, Fowler FJ Jr, O’Leary MP, et al. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol. 1992;148(5):1549-1557; discussion 1564.

Phranq D. Tamburri, NMD, is founder of Prostate Second Opinions, with an international patient clientele in Scottsdale, Arizona. Dr Tamburri has been Professor of Urology at his alma mater, Southwest College of Naturopathic Medicine (SCNM), for 20 years, and educates in all media forums for both patients and physicians on pragmatic approaches to refining the diagnosis and tracking of prostate cancer. He was uniquely medically cross-trained, from western Mayo Clinic surgeons to a Buddhist monastery while graduating from Kansai Gaidai, Japan. When not conducting prostate ultrasounds, Dr Tamburri loves Arizona desert rides on his obnoxious green Vaquero while blaring Tangerine Dream.


