Complexity Theory and What Ails Naturopathic Medical Education
David J. Schleich, PhD
Not too many days go by when our Deans don’t hear conflicting opinions about what naturopathic medical education should be concentrating on and preparing our candidates for. There are those NDs for whom the drift toward allopathic medicine’s systems and assumptions is alarming; this inclination, they feel, is at the expense of traditional naturopathy, whose roots, they feel, are fading macroscopically and in danger of disappearing altogether. There are others who champion the call for ever more science to back up traditional naturopathic approaches to healing and health in a world where the mantra, “evidence-based” is bandied, bruised and busked. Our Deans collectively wish, no doubt, that the universe of naturopathic medicine and its location in civil society were constant, simple to describe, and well protected from detractors and enemies vying to control market share.
No matter what classic rhetorical move we apply to this upsetting debate (e.g., post hoc ergo propter hoc – if B occurred after A, then A must have caused B; or the ‘slippery slope’ fallacy), for the naturopathic doctor, clinical practice intersects more frequently and fully these days than a generation ago with abundant new information coupled with those old rivalries, often bringing with it contrary imperatives. Many new young NDs like elements of “green allopathy” after all. Many new young NDs, however, also yearn for the revitalizing of the traditional naturopathic modalities. Thus, “the Gathering” annually; thus NCNM’s annual autumn “revitalization weekend.” The science of complex adaptive systems can help us to sort out why both extremes are part of the same process, even though its fundamentals are confusing to the uninitiated. Fear not; it’s rather interesting stuff.
Complexity theory arose when researchers in many fields, who were dealing with the intersection of massive waves of new data that make it increasingly difficult to describe or predict some phenomena, began thinking about how to systematically deconstruct the onslaught. In terms of naturopathic medicine, the health “systems” (whether orthodox or heterodox, to reference Baer [Baer, 2001, p. 82]) in which our medicine lives are large networks of what Mitchell (2009) calls “individual components, each typically following relatively simple rules with no central control or leader” (p. 12). Essentially, this means that there are “collective actions” which generate “changing patterns of behavior” (p. 12). It is the unrelenting change which gets confusing, in terms of understanding what to do at that place where entitlement, regulation and market share collide. The variables and components in the American health landscape are innumerable: hospitals, biomedicine and allied health care professionals, pharmaceutical enterprises, health administrators, medical educators and researchers, agencies and associations promoting and supporting specific health concerns and interests, food producers and distributors, and nutraceutical manufacturers and distributors including dietary supplement formulators, herbal product producers, genetically modified food and processed food, to name a few broad categories of social and economic activity with dozens of layers and offshoots for each. Within the manufacturing and distribution sector, there is a regulatory policy framework which determines whether, depending on ingredients and claims (therapeutic or not) what this group makes and sells is a food, food ingredient, or a dietary supplement.
There is also the complexity and organizational density of the pharmaceutical industry, focused as it is on generic and brand name medications and medical devices, with the overlay and intertwining filaments and leitmotifs of patenting, testing, marketing and research. Within such a kaleidoscope of information, entitlement, market control, corporate and intellectual history, it becomes significantly complicated to predict how a particular philosophy or regulatory prerogative will play out. For example, a familiar scenario is that at one time the Medical Trusts set out to brutally annihilate competition in the interests of “evidence-based” medicine. At the same time, consumer response to the self-interested foibles of the biomedicine industrial and professional complex [BIPC] redirects not only what is legally permissible in a particular jurisdiction, but what survives economically. Figuring out where naturopathic medicine is and where it is headed in such a terrain becomes exponentially difficult in terms of strategic planning and economic niche. It is really hard on our educational leaders to know what to emphasize and what to let go in a curriculum characterized by 30+ hours per week of seat time.
What is likely more helpful as a strategy is to shift away from prediction and control, in favor of attending carefully to the configuration of relationships among the ever-shifting galaxy of components. Rather than rallying instinctively against adversaries who are miserable to us in the marketplace as a central tactic, for example, complexity theory counsels us to understand what is creating patterns of order and behavior among those components before taking action. The “what” are outcomes: cost, effectiveness, and sustainability. Complexity theory speaks to self-ordering rules which provide both orthodox (MDs, DOs) and heterodox medical systems (Naturopathic Medicine, Chiropractic, Acupuncture and Oriental Medicine) a capacity to evolve differently and, at the same time, to “emerge to new patterns of order” (Mitchell, 2009, p. 27). Naturopathic professionals know that medicine and health promotion are not linear and predictable. Medicine and health promotion are characterized by a highly sophisticated, multi-layered, voluminous network of elements that interact. No one element in such a universe is in control, despite what the MDs, DOs, and pharmaceutical and big food producers may have in mind for the population. Complexity theory teaches us, instead, that, as Mitchell explains, “what emerges is directed by the recursive application of a small number of simple rules” (Mitchell, 2009, p. 143). One central rule is that a change in one element shifts the context for the whole enchilada. To illustrate: MDs are ranting these days about integration; their sudden attention to principles and practices long held in vulnerable moments by NDs is as much about the success of holism as it is about the momentum of the BIPC. Whether we’re talking about simple complex systems, complex adaptive systems, complex cognitive systems, complex social systems, or complex responsive processes [to list some of the conflicting lingo from complexity theory], naturopathic medicine (as a system) is as subject to transformation as any of the other elements in the system of health care in America. Going forward, we drink in the whole system and not merely our local experience and understanding. The disingenuity of the BIPC is, of course, not surprising within such a dynamic. Let’s drill down into how complexity theory can help us see what ails us in naturopathic medical education as we confront temptation to change what to teach.
Alexander (2010), for example, meticulously utilizes complexity theory to demystify the causes of what he calls nonlinear diseases (such as coronary heart disease, osteoarthritis, rheumatoid arthritis, multiple sclerosis, osteoporosis, asthma, varicose veins, and more). Many NDs contend that allopathic doctors use a “linear approach to what are complex biological systems” (p. 19) and thus have treatments which are either “ineffectual or non-existent” (p. 20). NDs report that scientific realism in medicine is hampered by scientific theories that only approximate universal truths about health. Biomedicine insists, for its part, that its theories about disease and the human body describe the world as it really is, “independent of human expectations, perceptions, and measurements” (Cacioppo et al, 2004, p. 214). The BIPC claims “evidence-based medicine” for itself as the standard for all care, the best of all possible worlds (referenced with apologies to Voltaire). In fact, the naturopathic community is not wary of science in medicine at all; rather, our community often points out that the defensiveness (manifesting in regulatory privileges of MDs beyond what they deserve when one considers the medical system they have developed and its track record, especially recently) can “impede progress and encourage defensiveness of and commitment to a theory well beyond its utility” (Cacioppo at el, 2004, p. 217). Reductionist medicine tends to salvage worthwhile protocols and treatments, and “leave in its wake the ruins of worthwhile beginnings and the lost utility of theories that have fallen out of fashion” (Cacioppo et al, 2004, p. 217). NDs reserve the right to combine medical knowledge, intuition and judgment. These, as Braunwald et al point out, “define the art of medicine, which is as necessary to the practice of medicine as a sound scientific base.” (Braunwald, 2000, p. 112). How, then, to negotiate the densely layered intersections of scientific medicine and traditional naturopathy?
Melanie Mitchell (2009), cited earlier, can help us to wade through this remarkable, helpful literature, outlining some common properties of complex systems, such as the health services delivery system in America, often depicted as very much alive, but also as broken and shockingly expensive. At the same time, our naturopathic doctor graduates, whether recent or not, find that system terribly upsetting because of its inequalities and ineffectiveness. It is the very complex system into which our grads are propelled each and every year. What makes it so confusing are the contrary elements. Mitchell suggests, for example, an interplay among three factors.
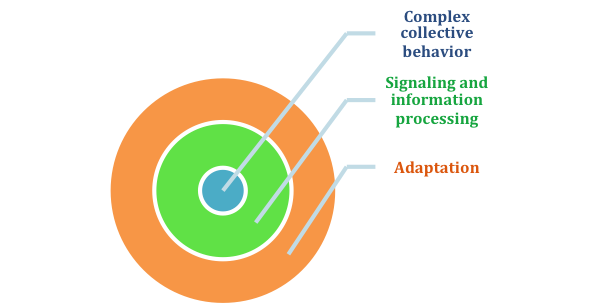
Mitchell explains that complex collective behavior references the “collective actions of vast numbers of components that give rise to the complex, hard-to-predict, and changing patterns of behavior” in the health care landscape faced by our ND grads (Mitchell, 2009, p. 13). It is incumbent upon naturopathic medical educators, then, to describe as many of those elements as possible in history and philosophy curriculum, in practice management curriculum, and in policy and regulatory affairs curriculum. Our graduates need to understand this terrain before diving into it.
Signaling and information processing means that all of these elements are going to barrage our profession with information and signals, both from individuals within the naturopathic profession and from outside of it. Some of the information and key messages will overlap; some will conflict. Our students and our grads need time to weigh in, reflect, and understand the larger patterns at work here. Integrative Medicine, from this perspective, is both an opportunity and a danger.
Finally, Mitchell suggests, as we go forward in this complex terrain, the varying systems (often competing) will continuously change their behavior to enhance survival. This process she labels adaptation. The BIPC is changing and adapting constantly, through learning and the evolution of its own market segments and differentiated parts. We have to be smart enough to know how to participate and to respond. For example, we are the trainers of choice in natural medicine theory, practice, modalities, products and treatment protocols, not MDs or DOs. Complexity theory makes the world, well, less complex and our place in it clearer.
 David Schleich, PhD is president and CEO of NCNM, former president of Truestar Health, and former CEO and president of CCNM, where he served from 1996 to 2003. Previous posts have included appointments as vice president academic of Niagara College, and administrative and teaching positions at St. Lawrence College, Swinburne University (Australia) and the University of Alberta. His academic credentials have been earned from the University of Western Ontario (BA), the University of Alberta (MA), Queen’s University (BEd), and the University of Toronto (PhD).
David Schleich, PhD is president and CEO of NCNM, former president of Truestar Health, and former CEO and president of CCNM, where he served from 1996 to 2003. Previous posts have included appointments as vice president academic of Niagara College, and administrative and teaching positions at St. Lawrence College, Swinburne University (Australia) and the University of Alberta. His academic credentials have been earned from the University of Western Ontario (BA), the University of Alberta (MA), Queen’s University (BEd), and the University of Toronto (PhD).
References
- Alexander, M. (2010). Complexity and Medicine: The Elephant in the Waiting Room. Nottingham, England: Nottingham University Press.
- Baer, H. (2001). Biomedicine and Alternative Healing Systems in America: Issues of Class, Race, Ethnicity, & Gender. Madison, WI: University of Wisconsin Press.
- Braunwalk (2000). Harrison’s Principles of Internal Medicine. 15th New York, NY: McGraw-Hill.
- Cacioppo, J.T., Semin, G.R., and Berntson, G.G. (2004). Realism, Instrumentalism, and Scientific Symbiosis: Psychological Theory as a Search for Truth and the Discovery of Solutions. American Psychologist. Vol 59, No. 4, 214-223.
- Mitchell, M. (2009). Complexity: A Guided Tour. New York, NY: Oxford University Press.