Autism Spectrum Disorder in Female Patients
KATRINA IIAMS-HAUSER, ND
Autism spectrum disorder (ASD) is a neurodevelopmental condition that presents in a stunning array of varieties. Hallmarks of ASD include difficulties with social interaction, restricted interests and behaviors, and symptoms that affect the ability to function in school, work, and other areas of life. Concomitant diagnoses like post-traumatic stress disorder, attention deficit hyperactivity disorder, and other cognitive disabilities add to the picture and must be properly evaluated. When sitting with an adult patient who has layers of life experiences, it can be difficult to distinguish neurodivergence from trauma, anxiety, or depression. Taking the time to gather enough information to make appropriate referrals can make the difference between spinning one’s proverbial wheels and arriving at proper treatments; though this is the case with all our medicine, it is especially meaningful for a person dealing with a mental health disorder.
Female experiences have not been well represented in the initial recognition of potentially autistic traits. The Interactive Autism Network acknowledges, “A growing number of studies suggest that girls with autism, particularly those without intellectual disability, may be hiding in plain sight.”1 Worse, many female patients receive multiple mental health diagnoses before they arrive at a diagnosis of ASD. As clinicians, let us be aware that women on the spectrum may present differently from men, gently connect our female patients with appropriate diagnostics and services, and help them develop structures in their lives so they may function optimally.
It would be a serious oversight not to mention the additional barriers to diagnosis caused by poverty, lack of access to medical care, and/or being a person of color. People of color are diagnosed at an even lower rate than white people.2 Also, there is a persistent bias in medical research that regularly ignores transgender and nonbinary people. There needs to be more awareness and support for both patients of color with autism and nonbinary/transgender patients with autism.
The Odds Are
The often-quoted ratio of ASD incidence in males:females is 4:1. A 2017 study found: “Of children meeting criteria for ASD, the true male-to-female ratio is not 4:1, as is often assumed; rather, it is closer to 3:1. There appears to be a diagnostic gender bias, meaning that girls who meet criteria for ASD are at disproportionate risk of not receiving a clinical diagnosis.”3 A clinician-led article just published this year (2022) looked at the male-female-odds ratio (MFOR), using data collected in a clinical practice focused on ASD in Australia. They found an MFOR closer to 3:4 for males:females with ASD, correcting for initial diagnosis biases and barriers to diagnosis for females.4
Knowing the true ratio is important to avoid “long-term severe negative consequences affecting mental health, self-perception and access to support.”4 Using an equation to extrapolate the percentage of females who missed diagnosis from known incidence data, they postulate that by age 18, 77% of females remain undiagnosed.4
Camouflaged
The diagnostic criteria are skewed toward the male expression of autism and fail to account for the impact of gender on behavior and overall presentation, including, quite notably, camouflaging behaviors. William Mandy, a professor of clinical psychology, states that “in the past 5 years, researchers have documented that many people on the spectrum learn to camouflage their traits. They may consciously suppress stimming behaviors in public or deliberately learn how to use certain gestures in social interactions. One person described this as ‘putting on my best normal.’”5 Camouflaging behaviors may include masking and compensating. Masking involves playing an appropriate role to avoid appearing unusual, while compensating involves planning out conversations ahead and practicing the right kinds of expressions/responses so as not to raise alarms.
The purpose of camouflaging is survival: to be part of the pack, to reduce stress, and most importantly, to stay safe. Safety does not merely involve a sense of mental or emotional security; physical and sexual safety is a vital concern. In a recent study, “the women who screened positive for autism had nearly 3 times the odds of having experienced sexual abuse as those who did not screen positive; those who screened positive for ADHD doubled their odds of sexual abuse.”6
Masking can lead to exhaustion, meltdowns, and frequent misunderstandings with others. If loved ones, teachers, and doctors are only seeing the mask, that can lead to many other problems with overall health and well-being. Breaking down may take place in private, but if it does take place in public, witnesses may simply dismiss or misread what might have caused it. “Difficult” behaviors are blamed on hormone problems; overstimulation is just being hypersensitive. Over time, low self-esteem patterns may develop, and if they take root, can escalate to a mental health crisis. Many neurodiverse folks live within these thresholds, and evidence of thriving is learning your own thresholds and how to work within them to maintain balance, avoiding crises.
Below is a graphic that details common motivations and consequences of camouflaging:
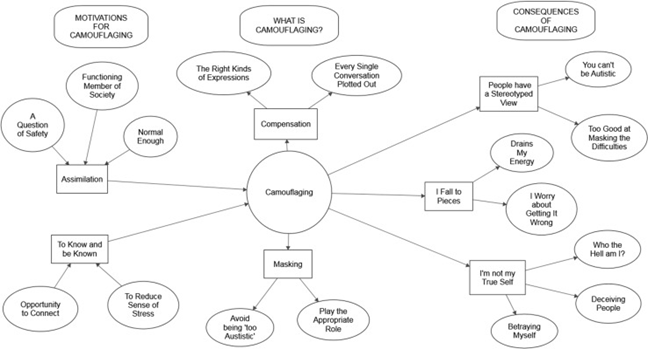
from “Putting on My Best Normal: Social Camouflaging in Adults with Autism Spectrum Conditions.”7
Addressing the Female Autistic Patient
If you have a woman or girl in your practice (or in your life) with consistent distress not explained well by other reasons, or have a patient who is extra sensitive, consider the possibility of ASD. Some of the pervasive challenges you can listen for when working with a female patient are:
- Difficulty with transitions/changes
- Trouble understanding social cues (ie, “reading the room” or recognizing personal boundaries)
- Conflicts with social maneuvering in general
- Feeling vulnerable (not understanding someone’s intent can create unsafe situations)
- Frequently feeling overstimulated or overwhelmed
- Anxiety at appearing odd or weird
Action Steps for Clinicians
Ask your patients if they can remember a time they did not feel anxious, depressed, or overwhelmed. If there is not another explanation (ie, childhood trauma), and it is difficult for them to answer, you may have a person with ASD or a related neurodevelopmental condition. Search for referral partners in your area who are experienced with seeing female patients and offer thorough and sensitive evaluations.
Adaptive Coping
For autistic women, the practice of recognizing one’s own distress signal and tending to oneself when distressed is critical and difficult work. In the naturopathic spirit of prevention, understanding one’s own thresholds and when one is approaching a threshold can allow a course correction to avoid a meltdown. We can help our patients plan decompression strategies into their environment and help them learn how to balance and re-regulate their nervous systems. Helping our patients have a solid care team, including supportive family and friends, and a therapist well-versed in working with autistic people, goes a long way towards learning how to adapt.
Adaptive coping mechanisms are unique to each individual. Here are a few general examples:
- Self-soothing practices (using noise-canceling headphones or watching a favorite show)
- Pleasant sensory stimulation (petting a dog or cat or wearing fabrics that are pleasing)
- Checking-in practices (“what do I observe about my body/mind/heart today?”)
- Regular routines
- Thinking ahead about the week or day and considering what will support best comfort and function
- Creating more time for decision-making: allowing oneself appropriate time and respectfully alerting others
- Eating, sleeping, and moving your body on a regular basis
- Trying experiments and seeing what works and what doesn’t, then making changes based on these observations
Conclusion
Hannah Gadsby, a comedian who often speaks about her ASD, said: “Once I understood that I was always going to have difficulty with self-regulation, I stopped worrying about it. Once I am distressed, my moods are not mine to control, but my environment is. I am always working to remove myself from all the cycles and patterns of hostile environments. I no longer search my behaviours exclusively for revelations about my character; I use my occasions of distress as ways to map the circumstances and environments I move through, and look for ways I can reduce my exposure to distressing situations. I have learned how to advocate for my own experiences instead of being ashamed of my pain and confusion. I stopped worrying about what I was expected to do and worked on building an understanding of what I could do to make myself feel safe and calm.”8 May all your patients (and you as well) find refuges of safety and calm.
[REFS]
- Sarris M. Are girls with autism hiding in plain sight? Are Girls with Autism Hiding in Plain Sight? | Interactive Autism Network. https://iancommunity.org/ssc/girls-autism-hiding-plain-sight. Published April 29, 2015. Accessed May 1, 2022.
- Aylward BS, Gal-Szabo DE, Taraman S. Racial, Ethnic, and Sociodemographic Disparities in Diagnosis of Children with Autism Spectrum Disorder. J Dev Behav Pediatr. 2021;42(8):682-689.
- Loomes R, Hull L, Mandy WPL. What Is the Male-to-Female Ratio in Autism Spectrum Disorder? A Systematic Review and Meta-Analysis. J Am Acad Child Adolesc Psychiatry. 2017;56(6):466-474.
- McCrossin R. Finding the True Number of Females with Autistic Spectrum Disorder by Estimating the Biases in Initial Recognition and Clinical Diagnosis. Children (Basel). 2022;9(2):272.
- Mandy W. In DSM-5, guidance on girls with autism is short but savvy. Spectrum. https://www.spectrumnews.org/opinion/dsm-5-guidance-girls-autism-short-savvy/. Published May 29, 2018. Accessed May 2, 2022.
- Ohlsson Gotby V, Lichtenstein P, Långström N, Pettersson E. Childhood neurodevelopmental disorders and risk of coercive sexual victimization in childhood and adolescence – a population-based prospective twin study. J Child Psychol Psychiatry. 2018;59(9):957-965.
- Hull L, Petrides KV, Allison C, et al. “Putting on My Best Normal”: Social Camouflaging in Adults with Autism Spectrum Conditions. J Autism Dev Disord. 2017;47(8):2519-2534.
- Gadsby H. Hannah Gadsby on her autism diagnosis: ‘I’ve always been plagued by a sense that I was a little out of whack’. The Guardian. https://www.theguardian.com/stage/2022/mar/19/hannah-gadsby-autism-diagnosis-little-out-of-whack. Published March 19, 2022. Accessed April 24, 2022.
[BIO]
Katrina Iiams-Hauser, ND (she/her), practices in the state of Washington. When not enjoying a deep dive into her special interests or sitting in silence, Dr Iiams-Hauser enjoys hearty laughter, singing, observing and experiencing nature, and spending quality time with her family.

