Tolle Causam
Angela Knapp, ND
Abstract
Research has linked polymorphisms in the Mannose-Binding Lectin 2 (MBL2) gene to increased susceptibility for autoimmune and infectious diseases. A 2018 study published in Archives of Neuropsychiatry investigated the role of MBL2 variants in obsessive-compulsive disorder (OCD) and Pediatric Autoimmune Neuropsychiatric Disorder Associated with Streptococcus (PANDAS). Findings revealed that MBL2 polymorphisms were significantly more frequent among patients with PANDAS compared to controls, with certain genotypes (notably the BB variant of rs1800450) strongly associated with susceptibility. These results suggest that MBL2 variants may serve as genetic markers for PANDAS risk. While larger and more diverse studies are needed, this work contributes to the growing body of evidence connecting genetic predisposition, immune dysregulation, and post-infectious neuropsychiatric syndromes in children.
Introduction
A 2018 study, published in Archives of Neuropsychiatry, found an association between Mannose-Binding Lectin 2 (MBL2) genetic variants and obsessive-compulsive disorder (OCD), particularly the type of OCD featured in Pediatric Autoimmune Neuropsychiatric Disorder Associated with Streptococcus (PANDAS).1
Prevalence & Clinical Features
PANDAS and Pediatric Acute-onset Neuropsychiatric Syndrome (PANS) are estimated to affect 1 in 200 children worldwide, according to lead research scientist Sue Swedo.2
PANDAS is an inflammatory response in the brain resulting from an inappropriate response to streptococcal infection. Its dramatic onset is identified by the development of OCD and motor tics, among other neuropsychiatric symptoms.3 A clinical diagnosis of PANDAS is defined as:
- Presence of obsessions, compulsions, and/or tics
- Abrupt onset of symptoms or relapsing-remitting course of symptom severity
- Pre-pubertal onset
- Association with streptococcal infection
- Association with other neuropsychiatric symptoms
The etiology of brain inflammation is thought to be autoimmune in nature, yet the underlying mechanisms of the disorder remain unclear.1
The MBL2 Research Study
Mannose-binding lectin (MBL) is a protein responsible for the Lectin Mannose pathway of the complement system. Deficiency in mannose-binding lectin has been associated with increased vulnerability to infectious and autoimmune diseases through its role in the innate immune response.1 MBL2, the gene that codes for mannose-binding lectin, can have variations that have been associated with autoimmune diseases, such as systemic lupus erythematosus and rheumatoid arthritis.4 More recently, variations in the MBL2 gene have been associated with increased susceptibility to rheumatic heart disease.5-8 The frequency of MBL2 variations has been estimated to be 25-30% among Caucasians.1 In the “Mannose-Binding Lectin 2 Gene Polymorphism in PANDAS Patients” research study, the 3 most common MBL2 polymorphisms (D – rs5030737; B – rs1800450; and C – rs1800451) were investigated in 102 OCD patients and 60 controls.
MBL2 variants were significantly more common in OCD and PANDAS groups
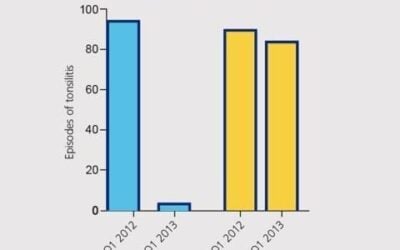
The number of variant alleles in MBL2 D, B, and C was significantly higher in the total OCD group and PANDAS subgroup.1 The BB genotype was higher in the PANDAS subgroup as compared to the OCD group, whereas this genotype was not found at all in the control group. As compared to the non-PANDAS subgroup, any MLB2 polymorphism was found 14.5 times more frequently in the PANDAS subgroup. Among the 102 OCD patients, 7 homozygous presentations were all found within the PANDAS subgroup. Of the 7 homozygous MBL2 genotypes, 6 were BB from the rs1800450, and 1 was from the rs5030737.
MBL2 genotypes may serve as markers for PANDAS susceptibility
Based on the regression analysis, MBL2 genotypes may be associated with PANDAS and can thus potentially serve as a marker for susceptibility to the disorder. Before this marker takes off as an identification of risk, additional research should be completed. This particular study was limited to patients within a Turkish Child and Adolescent Psychiatry Outpatient Department. Additionally, primary MBL serum levels were not evaluated in this study, and were therefore not correlated with risk of infection and autoimmunity.1
Future Genetic Studies for PANDAS & PANS
MBL2 is not the only promising gene in the field of PANDAS research. Columbia University Agalliu Laboratory has been leading the genetic research for PANDAS. In 2016, Tyler Cutforth, PhD, a research scientist at Columbia University Agalliu Lab, published a study9 suggesting numerous contributors to PANDAS pathogenesis, including the following:
- a unique bacterial strain or strains that induce an autoimmune response toward the host’s CNS;
- genetic risk factors that predispose children toward an autoimmune response following infection; and
- repeated infections of the throat or tonsils that, when left untreated, induce a robust Th17 cellular and humoral immune response targeted toward the brain
More recently, Dr Cutforth has continued his work by producing a key study of 44 patients with PANDAS that provides conclusive evidence that Streptococcus is at play in the disorder.10
According to Dr Cutforth,
We conducted this study using a combination of whole-exome sequencing and genome-wide association studies. We have identified two candidate genes in human PANDAS/SC patients (all from the Children’s Hospital of Philadelphia (CHOP), Center for Applied Genomics) that seem to implicate immune function and T cell regulation in these diseases (we call PANS/PANDAS/Sydenham’s collectively as post-infectious basal ganglia encephalitis). We have also validated these genes preliminary in our mouse PANDAS model. These genes are also completely different from risk genes recently described for the related diseases anti-NMDA receptor encephalitis, anti-Caspr2 encephalitis and anti-LGI1encephalitis, meaning that these illnesses likely have distinct biological origins and mechanisms and therapeutic targets. (Cutforth, 2016)10
Increasing genetic research will support the validity of the disease and continue to support identification of risk of PANDAS susceptibility prior to onset, as well as illuminate appropriate modalities to treat PANDAS. MBL2 has opened a doorway into genetic research that will help to prevent the disorder in children born to families with an autoimmune disease history, siblings of children with PANDAS, and children with recurrent strep infections.
References:
- Celik GG, Arslan Tas D, Yolga Tahiroglu A, et al. Mannose-Binding Lectin 2 Gene Polymorphism in PANDAS Patients. Arch Neuropsychiatry. 2018. Available at: http://pandasnetwork.org/wp-content/uploads/2018/10/erkenBaski-NPA22811MannosebindingLectin-ebpbik.pdf. Accessed April 15, 2019.
- PANDAS Network. Statistics. 2018. Available at: http://pandasnetwork.org/statistics/. Accessed April 15, 2019.
- PANDAS Network. About PANDAS, PANS, and AE. 2018. Available at: http://pandasnetwork.org/medical-information/. Accessed April 15, 2019.
- Panda AK, Parida JR, Tripathy R, et al. Mannose binding lectin: a biomarker of systemic lupus erythematosus disease activity. Arthritis Res Ther. 2012;14(5):R218.
- Gomaa MH, Ali SS, Fattouh AM, et al. MBL2 gene polymorphism rs1800450 and rheumatic fever with and without rheumatic heart disease: an Egyptian pilot study. Pediatr Rheumatol Online J. 2018;16(1):24.
- Marzetti V, Di Battista C, Ferrante R, et al. MBL2 and FCN2 gene polymorphisms in a cohort of Italian children with rheumatic fever: A case-control study. Semin Arthritis Rheum. 2017;47(2):264-268.
- Schafranski MD, Pereira Ferrari L, Scherner D, et al. High-producing MBL2 genotypes increase the risk of acute and chronic carditis in patients with history of rheumatic fever. Mol Immunol. 2008;45(14):3827-3831.
- Messias Reaon IJ, Schafranski MD, Jensenius JC, Steffensen R. The association between mannose-binding lectin gene polymorphism and rheumatic heart disease. Hum Immunol. 2006;67(12):991-998.
- Cutforth T, DeMille MM, Agalliu I, Agalliu D. CNS autoimmune disease after Streptococcus pyogenesinfections: animal models, cellular mechanisms and genetic factors. Future Neurol. 2016;11(1):63-76.
- PANDAS Network. Breakthrough Genetic Research in PANDAS. 2018. Available at: http://pandasnetwork.org/2016/08/new-book-for-educators-and-parents/. Accessed April 15, 2019.

Angela Knapp, ND, believes in the symbiosis of humanity and the environment. It was during her work as a small farmer after college that Dr Knapp recognized her goal to heal the earth by helping its inhabitants heal themselves. In 2013, Dr Knapp received her doctorate from NCNM, with a specialty in Natural Childbirth. She currently practices at the Peirson Center for Children, in Portland, OR. Dr Knapp is Staff Physician at Kashi Clinical Laboratories. She enjoys spending time with her family, preparing meals with locally procured foods, and grounding herself by getting her feet wet in any nearby body of water.