Catherine Price, NMD, MSAc
The most common use of acupuncture throughout the world is for pain management.1,2 In the United States, the primary reasons for acupuncture use are low back pain (34%), joint pain (16%), neck pain (14%), and headache or migraine (10%).3 It logically follows that pain management is a primary role of acupuncture in the naturopathic treatment of cancer. Interest in research on the efficacy of acupuncture was piqued by the 1997 National Institutes of Health consensus conference on acupuncture (http://www.nih.gov/news/pr/nov97/od-05.htm), as well as by an increase in federal funding for complementary and alternative medicine research since 1999. While most evidence-based medicine supports the use of acupuncture in cancer therapy or the treatment of pain, few randomized controlled trials (RCTs) specifically address the use of acupuncture in cancer pain management.4 However, the findings of pain RCTs and cancer RCTs may be translatable to cancer-specific pain because they address universal concerns about quality of life, such as fatigue, analgesia, and the psychosocial influences of both musculoskeletal pain and cancer.4 This should create a clear demand for RCTs on cancer-specific pain and for increased use of acupuncture by all physicians as its role as a valid indispensable treatment modality becomes evident.
Initially, several RCTs demonstrated that acupuncture was an effective treatment of pain compared with nontreatment, but few RCTs demonstrated that point-specific acupuncture was better than sham acupuncture.5 However, subsequent imaging investigations suggested that, although sham acupuncture did not often perform better than point-specific acupuncture, they each stimulated different deep cortical areas.5 Placebo stimulations were found to stimulate only the sensory cortex; electroacupuncture was shown to also decrease activation of the amygdala and hippocampus, the primal fear and memory centers.5,6 Therefore, the science of acupuncture could be altering how we interpret pain on a cognitive level.
Acupuncture was found to stimulate the release of β-endorphin, encephalin, endomorphin, dynorphin, and serotonin in animal models.5,6 These neurotransmitters were shown to modulate brainstem, thalamus, hypothalamus, and pituitary function in acupuncture-treated animals. These endogenous opioids and serotonin have been well documented to elicit pain relief in humans. However, until imaging studies were refined, the significance of these neurotransmitter effects was not translated from animal investigations to human studies.
Human imaging studies that included electroencephalography, functional magnetic resonance imaging, and positron emission tomography coalesced the results of clinical trials and animal neurotransmitter studies to suggest that acupuncture changes the way the brain works and that this is fundamental to its mechanism of action as a treatment modality that differs from placebo. In humans, wide neural networks of cortical and subcortical brain regions are affected by acupuncture, and response depends on the degree of paresthesia the practitioner is able to elicit. This paresthesia can be variously described as deqi, qi sensation, qi arrival, or dull pain. It differs from sharp pain, and most practitioners and American patients consider it harmful, as supported by functional magnetic resonance imaging.5,7 Qi can be defined as breath or vital energies.8 A recent human study by Qin et al demonstrated via functional magnetic resonance imaging that deqi, described as “[n]umbness, fullness, dull pain, heaviness and soreness,”9(Figure 2) mapped to specific neural networks that formed a hub at the posterior cingulate cortex and precuneus.
Acupuncture as a Treatment of Cancer Pain
According to Schrijvers, “30–40% of patients [with cancer] present this symptom [pain] at diagnosis, 40–70% during treatment and 70–90% during the palliative care phase.”10(pix37) Cancer type correlates with likelihood of cancer pain. For example, 5% of patients with leukemia have pain vs 52% of patients with lung cancer.10 About 80% of the time, the pain is from the tumor itself, but other cancer-related causes of patient, such as anticancer treatment (15%-25% of cancer pain prevalence), can contribute.
If given the choice, patients with cancer who have insurance may choose acupuncture and naturopathy as treatments. The cost of these treatments is modest compared with allopathic care. Patients with cancer most commonly seek complementary and alternative medicine for musculoskeletal pain, not for treatment of the cancer itself.
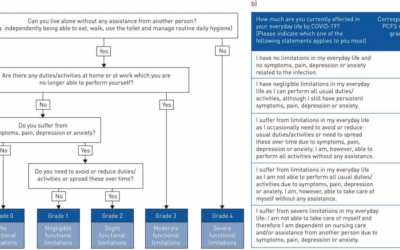
The World Health Organization11 created a plan for treatment of cancer pain called the 3-step ladder. Despite this protocol, a recent Cochrane review found that “[40%] of individuals with early or intermediate stage cancer and 90% with advanced cancer have moderate to severe pain and up to 70% of patients with cancer pain do not receive adequate pain relief.”12(abstract) According to the World Health Organization,11 if pain occurs, there should be prompt oral administration of drugs in the following order: nonopioids (aspirin and paracetamol); then, as necessary, mild opioids (codeine); followed by strong opioids, such as morphine, until the patient is free of pain. To calm fears and anxiety, additional drugs (adjuvants) should be used. To maintain freedom from pain, drugs should be given by the clock (ie, every 3-6 hours) rather than on demand. This 3-step approach of administering the right drug in the right dosage at the right time is inexpensive and is 80% to 90% effective. Surgical intervention on appropriate nerves may provide further pain relief if drugs are not wholly effective.
Acupuncture would easily fit into the adjuvant category. Because it increases endogenous opiate concentrations, it may have a place alongside the mild and strong opioids of the second and third steps.
Electroacupuncture effects cancer pain analgesia by decreasing substance P concentrations in the dorsal horn (sensory region) of the spinal cord and by increasing β-endorphin concentrations in the brain and blood.13 β-Endorphins can not cross the blood-brain barrier; although their levels increased by almost 52% in the blood, the more significant finding was a 12.6% increase in the brain. This study by Lee et al13 was performed in a neuropathic cancer pain mouse model that was inoculated with sarcoma cells around the sciatic nerves of mice.
Allopathic physicians have found that acupuncture is an appropriate and safe treatment of cancer pain, specifically lung cancer pain. Acupuncture received a 1A grade of recommendation (consistent, high-quality, likely reliable evidence) from the American College of Chest Physicians as a complementary, but not primary, treatment “when pain is poorly controlled or when side effects such as neuropathy or xerostomia from other modalities are clinically significant.”14(recommendation 7) “In patients with lung cancer with symptoms such as dyspnea, fatigue, chemotherapy-induced neuropathy, or postthoracotomy pain, a trial of acupuncture is recommended,”14(recommendation 11) receiving a 2C grade of recommendation (inconsistent, low-quality evidence). When “reducing the amount of pain medicine becomes a clinical goal,” acupuncture is “strongly recommended.” Auricular and electroacupuncture are recommended alongside standard acupuncture. Included in the rationale for these recommendations by the American College of Chest Physicians are the 1997 consensus statement by the National Institutes of Health that acupuncture is an effective treatment of postoperative pain, a large RCT showing improvement with acupuncture as an adjunct to standard care of knee osteoarthritis, and an RCT demonstrating that auricular acupuncture was better than placebo in treating patients with cancer pain, despite stable medication (most of the patients had neuropathic pain, which often resists standard treatment).14
Suggested Protocols
Few high-quality RCTs have shown that specific acupuncture points in humans surpassed placebo in treating cancer pain. In fact, after careful meta-analysis of acupuncture cancer treatments and cancer-related morbidity, the only acupuncture intervention that Chao et al15 recommended was acupressure on P6 for chemotherapy-induced nausea and vomiting. However, a handful of studies indicated successful acupuncture treatment of postoperative pain, arthralgias, or breast cancer-related lymphedema (which in turn causes pain) among patients with breast cancer.
In a small study of patients with operable non–small cell lung carcinoma, Wong et al16 found that acupressure to LI4, GB34, GB36, and SJ8 reduced the need for analgesic agents immediately after throracotomy compared with sham acupuncture. In another small study by Filshie et al,17 sternal and LI4 acupuncture successfully treated dyspnea related to the presence of malignant neoplasms. In a study by Sim et al18 of women undergoing elective gynecologic lower abdominal surgery, preoperative electroacupuncture reduced intraoperative and postoperative analgesic requirements. Electroacupuncture was applied at 2 Hz to acupuncture points ST36 and PC6 and at 100 Hz around the skin incision in a method similar to the “surround the dragon” technique. Lee et al13 used electroacupuncture at ST36 to effectively treat cancer-related pain in mice. The cancers in their mouse model were induced over the sciatic nerve. Therefore, translation of these findings may be questionable for cancer pain in a remote area, such as the brain, or in non–nerve-related pain, such as in leukemia. Lin et al19 used electroacupuncture stimulation of ST36 to treat non–cancer-related pain associated with lower abdominal surgery in humans.
Alimi et al20 demonstrated that cancer pain could be ameliorated by needling points on the ear where an electrodermal signal could be detected. There was no improvement in pain when needling was performed at spots without a signal. The authors recommended the use of auricular acupuncture to treat cancer pain that persists with steady medication.
Massage, specifically tui na, is an integral part of Traditional Chinese Medicine. Mehling et al showed that “[p]roviding massage and acupuncture in addition to usual care resulted in decreased pain and depressive mood among postoperative cancer patients when compared with usual care alone.”21(p258) This is true naturopathic medicine—combining the best of all available modalities.
Dr. Catherine Price, NMD, MSAc, is a graduate of Southwest College of Naturopathic Medicine and Health Sciences. She is interested in cancer care coordination and currently has a general practice at Woodstock Wellness Center and Zen Space Healing Center, in Portland, Oregon, where she focuses on pain issues, dermatology, and cancer. She also consults for GlaxoSmithKline and works with consumers who take the weight loss drug orlistat. She researched breast cancer at the University of California and Lawrence Berkeley National Laboratory, where she studied what the effect of electromagnetic fields is on breast cancer treatments and how breast cancer drugs and natural compounds interact with human cells and estrogen receptor α and β.
References
1. Vincent A, Kruk KM, Cha SS, Bauer BA, Martin DP. Utilisation of acupuncture at an academic medical centre. Acupunct Med. 2010;28(4):189-190.
2. Park J, Linde K, Manheimer E, et al. The status and future of acupuncture clinical research. J Altern Complement Med. 2008;14(7):871-881.
3. Mao J, Kapur R. Acupuncture in primary care. Prim Care. 2010;37(1):105-117.
4. Lu W, Dean-Clower E, Doherty-Gilman A, Rosenthal DS. The value of acupuncture in cancer care. Hematol Oncol Clin North Am. 2008;22(4):631-648, viii.
5. Campbell A. Point specificity of acupuncture in the light of recent clinical and imaging studies. Acupunct Med. 2006;24(3):118-122.
6. Lin JG, Chen WL. Acupuncture analgesia: a review of its mechanisms of actions. Am J Chin Med. 2008;36(4):635-645.
7. Hui KK, Sporko TN, Vangel MG, Li M, Fang J, Lao L. Perception of deqi by Chinese and American acupuncturists: a pilot survey. Chin Med. 2011;6(1):e2.
8. Britannica Online Encyclopedia. qi (Chinese philosophy. http://www.britannica.com/EBchecked/topic/109995/qi. Accessed May 29, 2011.
9. Qin W, Bai L, Dai J, et al. The temporal-spatial encoding of acupuncture effects in the brain. Mol Pain. 2011;7:e19.Quin et al
10. Schrijvers D. Pain control in cancer: recent findings and trends. Ann Oncol. 2007;18(suppl 9): ix37-ix42.
11. World Health Organization. Cancer: WHO’s pain ladder. http://www.who.int/cancer/palliative/painladder/en/. Accessed May 29, 2011.
12. Paley CA, Johnson MI, Tashani OA, Bagnall AM. Acupuncture for cancer pain in adults. Cochrane Database Syst Rev. 2011;(1):CD007753.
13. Lee HJ, Lee JH, Lee EO, et al. Substance P and beta-endorphin mediate electro-acupuncture induced analgesia in mouse cancer pain model [retraction in J Exp Clin Cancer Res. 2009;28:e137]. J Exp Clin Cancer Res. 2009;28:e102.
14. Cassileth BR, Deng GE, Gomez JE, Johnstone PA, Kumar N, Vickers AJ. Complementary therapies and integrative oncology in lung cancer: ACCP evidence-based clinical practice guidelines (2nd edition). Chest. 2007;132(3)(suppl):340S-354S.
15. Chao LF, Zhang AL, Liu HE, Cheng MH, Lam HB, Lo SK. The efficacy of acupoint stimulation for the management of therapy-related adverse events in patients with breast cancer: a systematic review. Breast Cancer Res Treat. 2009;118(2):255-267.
16. Wong RH, Lee TW, Sihoe AD, et al. Analgesic effect of electroacupuncture in postthoracotomy pain: a prospective randomized trial. Ann Thorac Surg. 2006;81(6):2031-2036.
17. Filshie J, Penn K, Ashley S, Davis CL. Acupuncture for the relief of cancer-related breathlessness. Palliat Med. 1996;10(2):145-150.
18. Sim CK, Xu PC, Pua HL, Zhang G, Lee TL. Effects of electroacupuncture on intraoperative and postoperative analgesic requirement. Acupunct Med. 2002;20(2-3):56-65.
19. Lin JG, Lo MW, Wen YR, Hsieh CL, Tsai SK, Sun WZ. The effect of high and low frequency electroacupuncture in pain after lower abdominal surgery. Pain. 2002;99(3):509-514.
20. Alimi D, Rubino C, Pichard-Léandri E, Fermand-Brulé S, Dubreuil-Lemaire ML, Hill C. Analgesic effect of auricular acupuncture for cancer pain: a randomized, blinded, controlled trial. J Clin Oncol. 2003;21(22):4120-4126.
21. Mehling WE, Jacobs B, Acree M, et al. Symptom management with massage and acupuncture in postoperative cancer patients: a randomized controlled trial. J Pain Symptom Manage. 2007;33(3):258-266.