The Role of Insulin in Metabolic Syndrome
Mary Shackleton, ND, MPH
Metabolic syndrome, also known as Syndrome X, was researched initially by Gerald Reaven. He defined metabolic syndrome as a cluster of cardiovascular risk factors, including hypertension, visceral adiposity (obesity), high triglycerides and low HDL cholesterol (Reaven, 1988). Subsequent findings of metabolic derangements exist that also contribute to metabolic syndrome, including: microalbumuinuria, impaired fibrinolysis, procoagulation, chronic and systemic inflammation, and insulin resistance.
Epidemiology of Metabolic Syndrome
A cross-sectional health survey of the American population showed that metabolic syndrome as defined by the National Cholesterol Education Program and Adult Treatment Panel (NCEP ATP III) affects one in four individuals (Ford, 2002). The overall prevalence of metabolic syndrome is similar in men and women; however, some metabolic features were more commonly observed in men (hypertriglyceridemia, hypertension, elevated fasting glucose).
The prevalence of metabolic syndrome increases sharply with age – more than 40% of individuals are older than 60 years. Ethnicity influences distribution of the features of metabolic syndrome: African-Americans had the highest prevalence of hypertension, Mexican-Americans had the highest age-adjusted prevalence of hyperglycemia. Overall, the prevalence of metabolic syndrome was higher among Mexican-Americans (32%) than in other ethnic groups, especially in women (Ford, 2002).
Symptoms of Metabolic Syndrome
Many people are unaware that they have metabolic syndrome, even though the American Heart Association estimates that 20%-25% of the adult U.S. population suffer from this disorder – between 58 and 73 million men and women.
Metabolic syndrome is characterized by having at least three of the following symptoms:
- Insulin resistance
- Abdominal adiposity – a 40-inch waist or larger in men; 35 inches or larger in women
- High blood sugar levels – at least 110 milligrams per deciliter (mg/dL) after fasting
- High triglycerides – at least 150 mg/dL in the blood stream
- Low HDL – less than 40 mg/dL
- Pro-thrombotic state (e.g., high fibrinogen or plasminogen activator inhibitor in the blood)
- Blood pressure of 130/85 mmHg or higher.
All these findings substantially raise the bar on the seriousness of metabolic syndrome, making it even more important that doctors correctly diagnose the condition and instruct their patients about one of its underlying causes – insulin resistance.
 How Does It Happen?
How Does It Happen?
Insulin resistance is the result of decades of consuming too many carbohydrates, a genetic predisposition for the disorder, a lack of physical activity, stress and a nutrient-deficient diet. These factors create insulin resistance, which can contribute to metabolic syndrome in two distinct ways.
First, insulin resistance reduces the number of insulin receptor sites on the cell wall. The average healthy person has some 20,000 receptor sites per cell, while the average overweight individual with metabolic syndrome can have as few as 5,000. The greater the amount of insulin produced in the body, the greater the resistance of the body to use it. It is unclear what causes this downregulation; however, it is this reduction of receptor sites that causes an inability to lower blood glucose.
The second way that insulin resistance causes metabolic syndrome is by raising insulin levels in the blood stream. Downregulation of receptors, unhealthy lifestyles and genetic conditions cause the pancreas to overproduce insulin. The excess insulin causes direct damage to the lining of the cardiovascular vessels and contributes to the formation of atherosclerosis, hypertension and dyslipidemia, leading to an increased risk of heart attack or stroke.
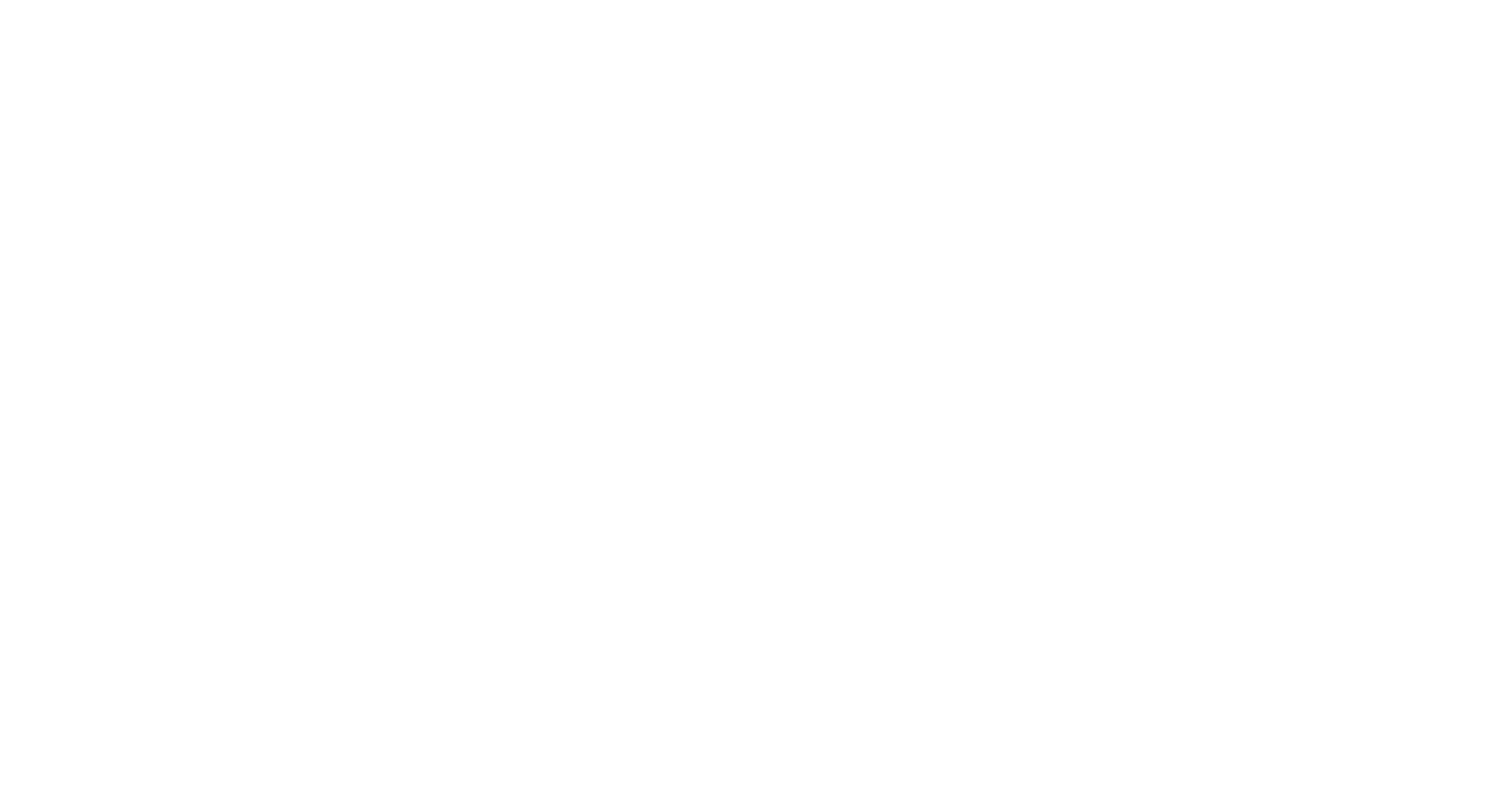
Insulin Resistance and Metabolic Syndrome
Many clinicians and researchers believe that insulin resistance underlies the cardiovascular pathologies of metabolic syndrome. One main reason for this is the role of insulin in fat homeostasis. Insulin’s major role is to induce the storage of fuel, and the most efficient form of fuel storage is fat – primarily triglycerides (TGs) in adipose tissue or in carbohydrate in the form of glycogen in liver and skeletal muscle. The effect of insulin resistance is an increase in circulating TGs. Due to insulin resistance, there is an increase in delivery of peripheral fatty acids to the liver, which, in turn drives hepatic TG synthesis. These TGs are then packaged into VLDLs, which are returned to the circulation.
Insulin resistance and its negative effects on metabolism, the increased levels of circulating TGs, the reduced levels of HDLs and hypertension all contribute to the progression of atherosclerosis. With associated coagulation and fibrinolysis pathologies, the cardiovascular events of metabolic syndrome can be devastating.
Obesity and Metabolic Syndrome
Obesity, in particular the accumulation of fat around one’s abdomen, is measured by waist-to-hip ratio or waist circumference, and plays a key role in the pathophysiology of metabolic disorders. Abdominal obesity is strongly predictive of coronary artery disease, more so than BMI, and has been associated with a cluster of dyslipidemic features, such as elevated triglycerides; increased VLDL; presence of small, dense LDL particles; and a decrease in HDL (Meigs, 2002). These abnormalities of lipoprotein metabolism relate to insulin resistance or hyperinsulinemia, and are proposed to be key diagnostic features of metabolic syndrome.
Note that obesity alone does not always lead to insulin resistance, as some individuals who are obese do not experience insulin resistance and, conversely, some individuals who manifest insulin resistance are not obese. These latter observations point to the added role of genetics in the acquisition of insulin resistance.
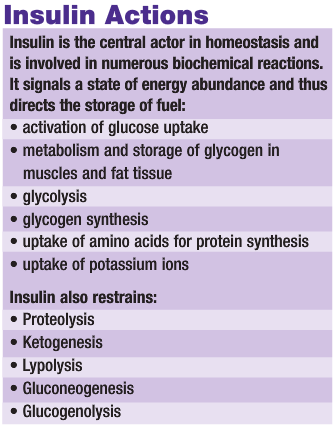
A Naturopathic Protocol
Insulin resistance is an underlying cause of metabolic syndrome, and many factors contribute to its presence. In essence, our environment and lifestyles have evolved too rapidly for our bodies to keep pace. We are still genetically “wired” to thrive on the entrenched habits of our ancestors, who consumed different, nutrient-rich foods and a diet low in carbohydrates, as well as sustained greater levels of movement and exercise.
At present, there is no single pharmaceutical drug that can reverse the symptoms of metabolic syndrome. A complete naturopathic approach that combines diet, exercise and nutrient supplementation is needed to treat the major cause of insulin resistance. See the accompanying text, Naturopathic Approach to Insulin Resistance, for recommendations.
References
Reaven GM: Role of insulin resistance in human disease, Diabetes 37:1595-607, 1988.
Meigs JB: Epidemiology of the metabolic syndrome, Am J Manag Care 8 (11 suppl):S283-92, 2002.
Ford ES et al: Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey, JAMA 287:356-9, 2002.
Striffler et al: Overproduction of insulin in the chromium-deficient rat, Metabolism Aug; 48(8):1063-8, 1999.
Anderson RA: Chromium in the prevention and control of diabetes, Diabetes Metab Feb;26(1):22-7, 2000.
Mertz W: Chromium in human nutrition: a review, J Nutr Apr;123(4):626-33, 1993.
Wang J et al: Effect of vanadium on insulin sensitivity and appetite, Metabolism Jun;50(6):667-73, 2001.
Willsky GR et al: Effect of vanadium(IV) compounds in the treatment of diabetes: in vivo and in vitro studies with vanadyl sulfate and bis(maltolato)oxovandium(IV), J Inorg Biochem May;85(1):33-42, 2001.
Evans JL, Goldfine ID: Alpha-lipoic acid: a multifunctional antioxidant that improves insulin sensitivity in patients with type 2 diabetes, Diabetes Technol Ther. Autumn;2(3):401-13, 2000.
Delarue J et al: N-3 long chain polyunsaturated fatty acids: a nutritional tool to prevent insulin resistance associated to type 2 diabetes and obesity?, Reprod Nutr Dev. May-Jun;44(3):289-99 Review, 2004.
Storlien LH et al: Skeletal muscle membrane lipids and insulin resistance, Lipids Mar;31 Suppl:S261-5 Review, 1996.
Storlien LH et al: Fatty acids, triglycerides and syndromes of insulin resistance, Prostaglandins Leukot Essent Fatty Acids Oct;57(4-5):379-85, 1997.
Khamaisi M et al: Lipoic acid acutely induces hypoglycemia in fasting nondiabetic and diabetic rats, Metabolism Apr;48(4):504-10, 1999.
Yaworsky K et al: Engagement of the insulin-sensitive pathway in the stimulation of glucose transport by alpha-lipoic acid in 3T3-L1 adipocytes, Diabetologia Mar;43(3):294-303, 2000.
Min Y et al: Adverse effects of obesity on red cell membrane arachidonic and docosahexaenoic acids in gestational diabetes, Diabetologia Jan;47(1):75-81, 2004.
 Mary Shackleton graduated from Southwest College of Naturopathic Medicine in Tempe, Ariz., in 1998. Shackelton also has a masters in public health from San Diego State University, and was the naturopathic physician on staff for the first disabled ascent of Mt. Everest in 1998. She is the co-founder and medical director of Insulite Laboratories, a supplement company dedicated to reversing disorders related to insulin.
Mary Shackleton graduated from Southwest College of Naturopathic Medicine in Tempe, Ariz., in 1998. Shackelton also has a masters in public health from San Diego State University, and was the naturopathic physician on staff for the first disabled ascent of Mt. Everest in 1998. She is the co-founder and medical director of Insulite Laboratories, a supplement company dedicated to reversing disorders related to insulin.