Trauma, the Amygdala and Post-Traumatic Stress Disorder: Part 1
Kelly Green Jennings, ND, MSOM
There are moments in our lives when the world splits open and forces us to decide what is most important to us and what we are going to do. These moments are highlighted by a clarity of memory that may seem uncanny, and often are tinged with the emotional surge associated with the event. When I saw the black silhouettes of planes crashing into the World Trade Center on September 11, 2001, I froze. My next moves were to spring into action, get into the City any way that I could and help out where I might be needed. My recall of that day and the week after seems fixed in my brain and body, vivid, clear and complete.
Our response to a given situation is very likely dependent on how our brain has matured. What kinds of environments were we exposed to? Nurturing and loving? Or fearful and anxious? Were our parents and families supportive in our development as individuals? Were we expected to fulfill a certain role, or behave a certain way? Did we grow up feeling safe and secure? Or was food scarce, and home an uncertain and transitory place? Countless factors influence the complex and impressionable development of the brain. In every moment, the brain patterns our perspective and, thus, our personal histories profoundly affect the way we see the world.
Past injuries are imprinted in our minds and impact our baseline response. Brain processes that underlie the basic emotions of fear, love, sadness and hate are designed to remember and give value to the past so that we don’t repeatedly find ourselves in harm’s way. However, these memories can also inhibit our physical, emotional and spiritual growth in the present moment.
What if we could help patients pinpoint past injuries that create conditioned responses, and see how these color their current state of well-being? What if we could learn how to use past ‘trauma’ to more effectively cope with present and future difficulties as they occur? Life’s stressors would ideally become vehicles for positive transformation, a way to help patients discover their higher purpose in life. Ultimately, if we can tease out the profound influences that have molded patients’ worldview, we can use these to help them learn how to live more fully, no longer controlled by the past and freely choosing their responses in each moment.
Limbic System
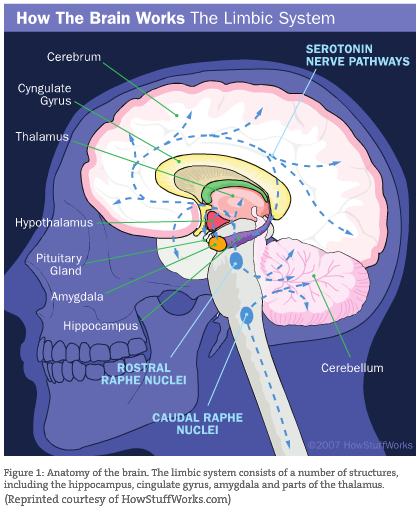
The system of the brain most relevant to this exploration is the limbic system. Here lies the origin of our emotional world, the beginnings of the sensation and expression of emotional feelings. More specifically, the amygdala is responsible for the ability to recognize fear, for the sensations associated with fear and the ability to express it. This almond-shaped structure sits on either side of the midline, just atop the brainstem. It becomes active during emotionally charged events and records them. As such, the amygdala governs a great deal: how we behave and make decisions; how we seek out safe marriages or continue to choose familiar, unstable ones; why we seek the security of a well-built home. Of course, cultural and contemporary influences impact these choices as well, but the direction of our decisions generally originates from our earliest emotional impressions. This inheritance makes its impact felt throughout our lives, and continues to shape and create our daily routine and habits.
The amygdala offers an important protective role, reminding us not to repeat mistakes. In a condition such as post-traumatic stress disorder (PTSD), the function of the amygdala becomes dysfunctional. This mental disorder often presents with a low-grade to paralyzing state of fear, manifesting both in physical and psychological symptoms. This has long-lasting, deleterious effects on the physiology of the body. PTSD arises following extreme exposure to stress, which is relative to the individual. What creates this hyper-reactivity? Are certain types of people more susceptible to traumatic events or their sequelae? How do we characterize these conditions, and how is the amygdala involved? Can these fear responses be de-conditioned? How can we help patients to move on from a traumatic event? These questions constitute the clinical focus of this article series.
 The Triune Brain
The Triune Brain
A look into the brain requires first an understanding of our origins. The modern human brain is composed of three distinct, albeit interrelated and interdependent, layers, which are the compositions of distinct evolutionary stages. The brainstem, the most primitive layer, finds its analogue in the reptilian brain and controls motor and vital functions necessary for survival and homeostasis, including arousal, reproductive drive, sensation, instinctual movement and impulse – the heart of sensorimotor or physiologic experience. The next layer, the limbic system, anatomically surrounds the brainstem and encompasses the capacity for parent-child bonding and enduring family units. It regulates the perceptual experience of incoming sensory information, memory, some social behavior and learning, and is associated with the experience and expression of emotions, including the desire for social-emotional contact. The third layer is the neo-cortex, which enables cognition, comprehension, self-awareness, decision-making and conceptual thinking (MacLean, 1985).
The human brainstem is almost fully functional at birth. The limbic system and neo-cortex are slower to mature and develop, and both are experience dependent. This means that all structures of the limbic system (amygdala, septal nuclei, hippocampus, etc.; see Figure 1) and the neo-cortex require considerable social, emotional, perceptual and cognitive stimulation during the first several years of life for normal and healthy development. The literature is replete with case studies of what happens when there is not sufficient stimulation for healthy neural development in these systems, in addition to what happens in abnormal and neglectful environments: Some neural connections wither and die; others persist that typically should atrophy. The initial years of an infant’s life are foundational for proper brain development. It is also apparent that this selective pressure and need for interaction continues throughout a person’s existence (Sapolsky, 2003). This key statement will become evident as we explore the continuing plasticity and dynamism of the brain throughout a person’s life.
Amygdala: Early Development
During much of the first year of life, a child will indiscriminately seek emotional contact and will smile at the approach of anyone. The need for social stimulation is so persistent that infants will desperately seek contact even with mothers who violently reject and physically abuse them (Joseph, 1992). If they don’t get this contact, they may die. Various accounts reiterate the research demonstrating that during the first three to five years of life, when the limbic system and neo-cortex are maturing, a nurturing environment is essential for sustaining and shaping a healthy human being (Joseph, 1999; Lewis et al., 2001).
As Allen Schore details in his book, Affect Regulation and the Origin of the Self (1994), dysfunctional or negative interactions with the primary caregiver result in permanent neurochemical and anatomical changes of the limbic structures of the brain. This has enduring implications on personality development and can play a causative role in a wide variety of clinical disorders (Schore, 1994). The synaptic projections of the amygdala in particular are profoundly reliant on upbringing. The size, function, connection and strength of these projections are determined by environmental input, and microscopic changes in relation to varying external sensory stimuli have been detailed by numerous studies. This includes alterations in the neurochemistry, cell membrane, anatomical structure and signaling capabilities of single neurons within the amygdala.
The amygdala is the first limbic structure of the brain to fully develop after birth, usually by one year of age. During this impressionable time, infants begin to discriminate between familiar faces and strangers. The inklings of independence begin as we see the emergence of self. Children will start to recognize their own image in the mirror, and increasingly seek positive reinforcement. They will begin to test boundaries, discovering the difference between what is safe and what is not safe through the eyes and reactions of their caretaker. It is apropos that these developmental milestones occur when the amygdala is maturing, guiding infants’ recognition of the familiar and secure boundaries of their world while increasing their sense of attachment and sensitivity to affection, mood and environment. Note that while these structures of the brain are maturing, they are dependent on input from other systems in the body that are also developing. The endocrine and digestive systems in particular play a critical role in determining a child’s physiological and psychological sense of self, and must be considered in a whole-systems approach to medicine.
Amygdala: Connection and Function
The amygdala is composed of two almond-shaped, fingernail-sized structures on the innermost part of either temporal lobe. It is connected to many other structures within the limbic system and also extends outward to command centers in the brainstem and the cortex.
The amygdala itself is a composite of four differing clusters of neurons: the central nuclei, the medial nuclei, the cortical and basomedial nuclei, and the lateral and basolateral nuclei (Swanson and Petrovich, 1998).
The central nucleus is most closely linked with the brainstem and is highly involved in manipulating the body’s response to emotional stimuli through the autonomic nervous system. When we encounter something we perceive as dangerous, the danger signal is first conveyed to our central nucleus in the amygdala, which activates the brainstem and initiates a sequence of responses: sweaty palms, adrenaline, pounding heart, the impulse to take flight. Blood is rerouted to the organs most essential to our survival.
It is important to mention that while many activities of the so-called autonomic nervous system are involuntary, some are decidedly not. Breathing, for example, can in part be consciously controlled. Not only can some autonomic functions be mindfully controlled, they can also exert powerful feedback onto the limbic system. In the same way that the central nucleus of the amygdala wields top-down regulation of the body’s responses, the body can exert a reciprocal bottom-up influence on the brain. This suggests the significant potential for conscious self-regulation even during times of high stress. It explains, at least in part, why meditative practices have a profound effect on well-being.
The medial nucleus connects to the accessory olfactory system, which evolutionarily is associated with the detection of pheromones. Whether humans are as influenced or responsive to pheromones is controversial; however, their use among insects, many vertebrates and even plants has been particularly well documented.
The cortical and basomedial nuclei of the amygdala directly link with the main olfactory system. In addition to the perception of odor, this system must be able to create a representation of the odor, distinguish a new odor and pair the odor with a memory of what the odor represents.
The lateral and basolateral nuclei communicate predominantly with the frontotemporal and prefrontal cortex, which is involved with the cognitive processing of emotion. It is this set of neurons that produces the conscious feeling of fear. The cortex, a relatively recently evolved brain structure, offers a distinct, self-conscious line of defense against fear. The ability to think about our actions before we impulsively react provides a buffer to the fear response. However, while it takes only 12 milliseconds for an auditory stimulus to reach the amygdala, it takes up to three times as long to reach the cortex. This is a significant lapse of time, in which fears could explode and someone might get a blow to the head.
In addition to the branches that these nuclei have extending outward to their respective regions of the brain, each of the subdivisions is highly interconnected within the amygdala.
Amygdala: In Emotional Memory
The amygdala is highly activated when incoming sensory information is linked with emotional content. The amygdala enhances memory depending on the profoundness and emotional value of an event. Because of its central position, it can modulate perceptual sensitivity to incoming information. It sits next to and is integrally linked with the hippocampus, the part of the brain associated with recalling details of a past event. As the amygdala is activated in new circumstances and situations, it tells the hippocampus “Hey! Pay attention! We’ve got some important information coming in here!”
The amygdala also dictates our ability to discern and express subtle social and emotional nuances. It is the sensory gateway to the emotions – perhaps as some researchers suggest, the true seat of emotional and social intelligence (LeDoux, 1996). Studies on a number of patients with localized damage to the amygdala report specific impairments in the recognition of facial expressions of fear (Adolphs et al., 1996; Broks et al., 1998). Recognition of other emotions was left intact. Judgment of trustworthiness and approachability of unfamiliar adults from facial photographs was also skewed; patients with damage to the amygdala considered strangers to be more approachable and trustworthy compared to the control group (Adolphs et al., 1998). One patient with bilateral amygdala damage was unable to recognize vocal signs of fear and anger (Scott et al., 1997). This research suggests the amygdala is necessary for the perception and recognition of fear as well as its sensation and expression.
Of relevance to our present discussion is the way in which the amygdala is affected by life events. Trauma is often used to describe an event like a car crash or a beating, but psychiatrists and social scientists use the term to describe what takes place inside after these moments pass. Some studies show that chronic daily stress can exert just as profound an influence on the body as a major traumatic event, highlighting the fact that our society as a whole may be suffering from a silent epidemic of post-traumatic stress. This is particularly valid after September 11, 2001.
We accumulate our fears in flashbulb memories stored in the amygdala, which in turn keeps the brain and body hyper-aroused, prepared for the next attack. For some people, nightmares, flashbacks and unbidden thoughts can be triggered by seemingly ordinary events. Victims of trauma may dissociate or shut down aspects of their personality. Together, these experiences manifest themselves in what has come to be called post-traumatic stress disorder.
Next issue’s article will discuss PTSD in detail, and will offer related case studies treated from a naturopathic viewpoint.
 Kelly Green Jennings, ND, MSOM is a graduate of NCNM. She has treated 1,000+ patients over her last five clinical years. Her specialties include chronic disease, cancer treatment, sports-related injuries, nutritional counseling, physical and emotional recovery from trauma and family medicine, among others. She is presently writing a breast cancer manual for holistic practitioners designed to help physicians help their patients with supportive treatment options. She has mentored with some of the top doctors in the Pacific Northwest. She currently works at Urban Wellness Group in Portland.
Kelly Green Jennings, ND, MSOM is a graduate of NCNM. She has treated 1,000+ patients over her last five clinical years. Her specialties include chronic disease, cancer treatment, sports-related injuries, nutritional counseling, physical and emotional recovery from trauma and family medicine, among others. She is presently writing a breast cancer manual for holistic practitioners designed to help physicians help their patients with supportive treatment options. She has mentored with some of the top doctors in the Pacific Northwest. She currently works at Urban Wellness Group in Portland.
References
MacLean PD: The Triune Brain in Evolution: Role in Paleocerebral Functions. New York, 1990, Plenum Press.
MacLean PD: Brain evolution relating to family, play, and the separation call, Arch Gen Psychiatry 42: 405-417, 1985.
http://www.ahaf.org/alzdis/about/AnatomyBrain.htm
Sapolsky RM: Stress and plasticity in the limbic system, Neurochemical Research, November; 28(11):1735-1742, 2003.
Joseph R: The limbic system: emotion, laterality, and unconscious mind, Psychoanal Rev 79:405-456, 1992.
Joseph R: Environmental influences on neural plasticity, the limbic system, emotional development and attachment: a review. Child Psychiatry Hum Dev 29(3):189-208, 1999.
Lewis T et al: A General Theory of Love. New York, 2001, Vintage Books.
Schore Allen N: Affect regulation and the origin of the self. Philadelphia, 1994, Lawrence Erlbaum Associates, pp. 10, 13.
Swanson LW and Petrovich GD: What is the amygdala?, Trends Neurosci 21:323-331, 1998.
Killen A: Geography of feeling. Available from www.salon.com/books/it/1999/04/07/neurology/index.html.
LeDoux JE: The Emotional Brain: The Mysterious Underpinnings of Emotional Life. New York, 1996, Simon & Schuster.
Adolphs R et al: Cortical systems for the recognition of emotion in facial expressions, J Neurosci 16:7678-7687, 1996.
Broks P et al: Face processing impairments after encephalitis: amygdala damage and recognition of fear, Neuropsychologia 36:59-70, 1998.
Adolphs R et al: The human amygdala in social judgment, Nature June 4; 393:470-474, 1998.
Scott SK et al: Impaired auditory recognition of fear and anger following bilateral amygdala lesions, Nature Jan 16; 385:254-257, 1997.