CLINICAL ROUNDS IN FUNCTIONAL AND NUTRITIONAL MEDICINE- Part 5:Food Intolerance
David M. Brady, ND, DC, CCN, DACBN
Part Five in the Clinical Rounds series. These clinical rounds are real case studies from my practice. It is my aim to present interesting cases to facilitate thought and discussion about novel diagnostic and therapeutic techniques for a myriad of clinical conditions that are likely to appear in your offices.
Patient Presentation and History
A 38-year-old female presented with the primary complaint of a severe facial rash. Her entire symptom/complaint list was as follows:
- Severe facial rash
- Pruritis (itching)
- Fatigue
- Frequent colds, flu, and laryngitis
- Asthma
The onset of her symptoms was approximately 1.5 years before presentation, with the exception of her asthma, which dated back to childhood. I particularly remember my medical assistant coming to me after she had taken the patient’s vital signs and saying to me, “You are not going to believe the facial dermatitis that this poor woman has.” When I entered the room my immediate impression was that this woman was having a major skin reaction to either a contact or food allergen. Upon completing her medical history I learned that she had been seen by multiple physicians at the Yale College of Medicine and was actually the focus of a case discussion between the departments of dermatology and allergy at Yale.
Prior Management
Standard patch testing was performed on the patient at Yale, which included various contacts, molds, and foods. The only positives were lanolin, carbol mix, and black rubber mix, all common ingredients in cosmetics. She did not think that these were the cause since she did not customarily wear many cosmetics and total discontinuation did not resolve her problem. She was specifically told that she was not allergic to any foods. She was subsequently put on topical steroid cream, which showed only mild improvement, mostly with the itching. However, the effects diminished over time and eventually it did not provide any benefit at all. She was then given oral steroids in the low-potency class without results. Steroids in the high-potency class did not fare much better. Eventually, she was taken off all medications and told to just use Vaseline on her rashes as a lubricant. She was essentially out of options. She then was told about our integrative medical practice by a friend and presented to us.
Physical Examination
The patient had a well-demarcated eczematous appearing rash involving the forehead, periorbital region, cheeks, upper arms, and back. Her face appeared “raw” with cracks that appeared to be bleeding. She was obviously very distressed and stated, “I am afraid to leave my house because I look like a monster.” EENT examination revealed a reddened oropharynx without tonsillar exudate and obvious candidiasis along the tongue and buccal mucosa. On follow-up questioning, she did admit to frequent vaginal yeast infections and perianal itching. Mild lymphadenopathy was noted in the cervical chains. Ear, eye, and thyroid exams were normal. Heart evaluation revealed a normal rate and rhythm without murmur, and lung examination revealed normal breath sounds. Abdominal examination was essentially normal with the exception of mild tenderness to deep palpation in the extreme quadrants.
Initial Impressions
The presence of this type of skin disorder always causes the functional medicine practitioner to consider an allergy-related problem. The prior workup by the conventional allergists and dermatologists seems to have ruled out a topical contact allergy, making food allergy a more likely etiology. Since intestinal hyperpermeability (leaky gut) can cause a dramatic increase in the antigenic and toxic load into systemic circulation, mucosal gut disorders and hepatic detoxification insufficiency must also be considered as strong contributing factors. The oral thrush, reddened oropharynx, fatigue, and chronic infections may be due to immunosuppression from the multiple courses of steroids or the constant demand placed on the immune system from the chronic ingestion of antigenic foods.
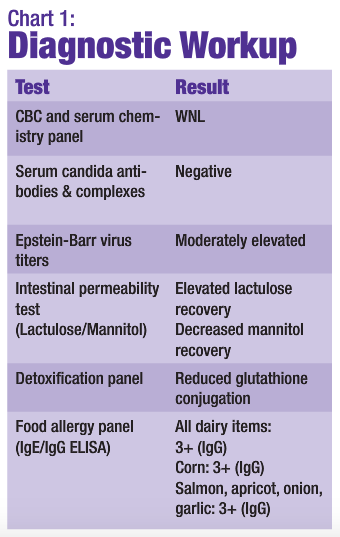 Discussion of Diagnostics
Discussion of Diagnostics
The CBC was performed in order to evaluate the patient for anemia due to the fatigue, as well as to check infectious status. The patient did not appear to be anemic or to have an acute infection. Serum chemistries did not reveal any significant internal pathology. The normal candida serum antibodies and complexes may seem odd given the obvious oral thrush and history of vaginal yeast infections. However, this is seen quite frequently when the yeast is confined mainly to the GI tract and has not become systemic. EBV titers were ordered because of the long-standing fatigue and the patient’s history of a severe case of mononucleosis as a teenager. Elevated titers may be contributing to the patient’s fatigue and immunosuppression, and the activation of the virus may be related to the steroid use.
The intestinal permeability study showed that lactulose, a large, normally nonabsorbable sugar, was passing through a “leaky” intestinal mucosa. The smaller sugar, mannitol, was not being absorbed at normal levels, suggesting some degree of malabsorption. Although it may seem counterintuitive to have leaky gut and malabsorption simultaneously, it is actually seen quite frequently. While the large lactulose is finding its way through the gaps between damaged mucosal cells, the smaller mannitol is not being actively absorbed through the cells as it should be because of inflammatory damage of the gastrointestinal villi. This inflammatory damage results in a loss of mucosal surface area and malabsorption. The net effect is a gut that is “leaky” to large molecules (i.e., antigenic proteins and large toxins), while a malabsorption of smaller molecules (i.e., micronutrients) also exists.
Stool analysis was deferred because of the lack of overt GI symptoms. It was to be considered if the initial therapeutic strategy did not produce satisfactory results. Hepatic detoxification did not appear to be significantly impaired at this point, but the glutathione phase II conjugation pathway was a bit sluggish.
The initial food allergy panel was performed via ELISA IgE/IgG methodology. It was obvious that the patient had a major problem with dairy. All dairy-related items such as American cheese, casein, cheddar cheese, cottage cheese, cow’s milk, goat’s milk, lactalbumin, mozzarella cheese, Swiss cheese, and yogurt were graded as 3+ IgG responses. Further questioning of the patient based on the laboratory results revealed that her childhood included chronic ear infections and antibiotic use. Her parents always made her drink milk, and even to this day she eats a bowl of vanilla ice cream almost every evening as a “comfort food.” She rents a room in the house of a Mexican American family who cooks most of her meals for her. The Mexican-influenced diet is very high in dairy and corn (another one of her 3+ foods). Could overexposure to these foods combined with a leaky gut result in a severe cyclic food allergy and many of her symptoms?
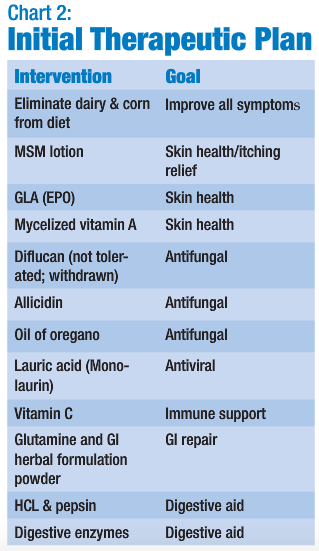 Initial Therapeutic Plan
Initial Therapeutic Plan
The initial therapeutic strategy was meant to provide rejuvenation of the skin, improve intestinal function and hepatic detoxification, enhance immune function, and combat the candidiasis and viral challenge.
The patient did not respond well at all to the Diflucan. It was decided to put her on a very brief course of the medication because of the frank oral thrush. However, she experienced headache, and just complained of feeling sick when she took it. It was withdrawn and she was then put on natural antifungal products (Allicidin, pre-formed and stabilized allicin extract from garlic, and oil of oregano).
Follow-up: Four Weeks
- Facial rash 50% improvement
- Less fatigue
- No apparent oral thrush
- Normal pharynx
- No lymphadenopathy
Follow-up: Twelve Weeks
- Facial rash 100% resolved
- Neck & arm rashes 100% resolved
- No candida infections
- No respiratory, throat, or ear infections
- Improved energy & vitality
Clinical Management (long term)
- Elimination of dairy from diet
- Reintroduction and rotation of corn
- Multivitamin
- Antioxidant complex
- GLA (EPO)
Follow-up: Ten Months
- Intermittent return of facial rash
On a 10-month follow-up visit the patient complained that the rash was just starting to return. She had been attempting to slowly rotate corn back into her diet. At this point it was decided to retest the patient for food allergy. The test performed uses whole blood, as opposed to serum alone. Rather than just checking for IgE and IgG antibodies related to certain food proteins, it actually analyzes cellular changes that occur to leukocytes when they are exposed to challenge foods. The patient’s results were as follows:
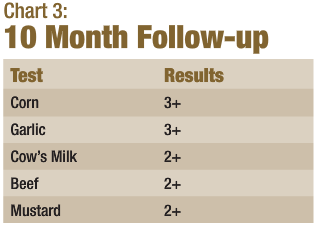 Additional Discussion
Additional Discussion
It is interesting to note that cow’s milk was no longer the most reactive substance, probably because of her strict avoidance for an extended period. The attempt at reintroduction of corn may be reflected in the very strong reaction to corn. Garlic was also still significantly positive. Additional substances were found to be reactive, such as beef and mustard. The patient was informed that reintroduction of corn was probably not possible and she was instructed to completely eliminate dairy, corn, garlic, beef, and mustard from her diet. She was also advised to consider elimination of other members of the Allium family, such as onions and leeks. She was given the option of attempting provocation-neutralization therapy for her food intolerance; however, it was my opinion that it was not likely to be very effective, so she declined. The patient was also kept on her multivitamin antioxidant complex and essential fatty acids. It was decided to reintroduce a small dose of HCL and pancreatic enzymes with meals in an attempt to more adequately digest proteins into less antigenic forms. She was more than willing to follow this supplement program and to simply eliminate these foods if it meant that she would not have to suffer the discomfort and embarrassment of her previous condition.
Conclusion
This patient has not had a return of her rash or other symptoms to date. She has become a strong advocate of my practice and has referred multiple patients. Her case was chosen to illustrate the importance of the accurate detection and management of food intolerance in our patients with chronic health problems. This case also serves to outline the functional medicine integrated approach to the management of panallergic patients. Intestinal health, digestive function, detoxification, and often adrenal function all need to be evaluated and addressed in order to comprehensively treat these conditions.

David M. Brady, ND, DC, CCN, DACBN is a naturopathic physician, board-certified clinical nutritionist, and doctor of chiropractic. He is the chief medical officer of Designs for Health, Inc. and serves as a technical consultant to Metametrix Clinical Laboratory. He is also presently the director of the Human Nutrition Institute at the University of Bridgeport, and is an associate professor of clinical sciences at the University of Bridgeport, Colleges of Naturopathic Medicine and Chiropractic in Bridgeport, Connecticut. Dr. Brady also maintains a private practice at The Center for the Healing Arts in Orange, Connecticut, where he specializes in functional and metabolic medicine.









