Sleeping With Your Stress: Sleep Apnea
Sussanna Czeranko, ND, BBE
Sleep consumes about a third of our lives. It is no wonder, then, that “sleep medicine,” like so many other aspects of human experience, has been medicalized and monetized within biomedicine. There are numerous sleep disorders that have been researched and that drive a massive market of therapies, devices, pharmaceuticals, and procedures. There is a growing and complex lexicon of terminology to assimilate, from apnea-hypopnea index to uvulopalatopharyngoplasty and zeitgeber. We are already familiar with such diagnostic terminology as insomnia, narcolepsy, obstructive sleep apnea (OSA), gastroesophageal reflux disease, arousal disorders, dyssomnia, parasomnia, Klein-Levin syndrome, sleep paralysis, hypersomnia, parasomnia, periodic limb movement disorder, chronic obstructive pulmonary disease, chronic obstructive pulmonary disease emphysema, night-sleep terrors, night sweats, nyctophobia, bruxism (enter the dental profession), and restless legs syndrome, to name a few. Surrounding these medical treatments, diagnoses, and terminology is a massive industry of drugs, including zaleplon, clonazepam, methylphenidate, pemoline, paroxetine, fluoxetine hydrochloride, temazepam, protriptyline hydrochloride, zolpidem, and zopiclone, also to name a few. Keeping the sector’s wheels turning and the revenue flowing, a research machine is under way with professional journals and books (eg, SLEEP, Vigilia-Sueño, and Focus, a journal for respiratory care and sleep medicine managers and educators), sleep-related foundations and associated organizations (eg, the National Sleep Foundation), and even the American Automobile Association for Traffic Safety. Sleep research sites abound such as the Sleep Research Laboratory (United Kingdom), Computational Models of Sleep Spindles and Thalamic Cell Activity (Quebec, Canada), and the Molecular Onirology Laboratory (France), once again to name a few. There are dozens of sleep disorder centers all over the globe, from Argentina to the United States.
Because I have a strong, professional interest in breathing therapies, the intersection of my naturopathic tools with the bulky and populated offerings of so-called sleep medicine has proven challenging. Selecting and ordering from this spiraling continuum, we will want to emerge with naturopathic treatment options most particularly for sleep apnea that are effective and in keeping with our whole-person approach to health.
The subject of sleep apnea embraces 2 huge disciplines, namely, pulmonology and the new branch referenced earlier, called sleep medicine. It is impossible to capture in summary all the salient points in these 2 vast areas within the confines of one article; however, I intend to unravel some of the conflicting information occurring in the research field and to present the merits of breathing therapy as a treatment option for the naturopathic profession.
Bradley reports: “Respiratory sleep medicine began in 1965 with the original polysomnographic description of obstructive sleep apnea [OSA] by [H.] Gastaut and colleagues,”1(p363) when the presence of apnea during sleep in a subgroup of “Pickwickian” patients was observed. Since this first study, understanding the pathogenesis of the different forms of sleep apnea has seen much progress. Central sleep apnea (CSA) and OSA and their many variant forms are seen from children to the elderly. Young and his colleagues noted that apnea and hypopnea “cause acute adverse effects, including oxyhemoglobin desaturation, fluctuations in blood pressure and heart rate, increased sympathetic activity, cortical arousal, and sleep fragmentation.”2(p2012) Dr William C. Dement documented the first sleep center of its kind, set up in 1970 at Stanford University, Stanford, California.3 In that first year, there were 3 studies published, and since then the number of studies found in a PubMed search on this topic has risen to 20 845. Sleep apnea has in less than 5 decades become a major contender in chronic disease research and treatment, as can be seen not only by the rise in sleep study clinics but also in insurance coverage, presenting statistics, and even over-the-counter medication markets.
Sleep Apnea Present in 1 in 5
There are about 75 medicalized sleep disorders currently generating a $30 billion sleep medication market.4 Apnea as a diagnosis has become a major concern because of its prevalence and impact. An estimated 50 to 70 million US adults have a sleep or wakefulness disorder of one kind or another.5 Obstructive sleep apnea, for example, is the most prevalent form and is “characterized by intermittent complete and partial airway collapse, resulting in frequent episodes of apnea and hypopnea.”2(p2013) One in five adults, it is reported, has mild OSA, and 1 in 15 has moderate to severe OSA.2 Central sleep apnea is when the brain temporarily stops sending the message to respiratory muscles to breathe.
An apnea index of 5 per hour or greater is considered abnormal and indicative of sleep apnea.6 Apnea itself is defined broadly as absent airflow for 10 seconds or more.7 However, research data point to some patients who have had an apnea event where they stopped breathing for a couple of minutes. At one time, OSA and CSA were distinct pathologies; however, it is currently recognized that the overlap between them is too great to think of each as separate. Malhotra and Owens contend that “the majority of respiratory events are, in fact, hypopneas, in which obstructive versus central physiology is often difficult to distinguish clinically.”8(p1169) Although OSA and CSA apparently overlap clinically, the terminology differentiates these 2 apneas. Obstructive sleep apnea focuses on the site of the airway collapse and abnormalities in the upper airway soft-tissue structures.9 Central sleep apnea has developed a concept of “loop gain, which is a measure of the stability or instability in the ventilatory control system.”8(p1169)
The symptoms and characteristics of sleep apnea syndrome can be life-threatening and have been associated with cardiovascular morbidity and mortality,10 as well as with excessive daytime sleepiness, loud snoring, and restless and nonrestorative sleep.11 These latter symptoms did not get recognized as a sleep-disordered breathing until the mid-1970s. In one of the first articles on sleep apnea syndrome, by Guilleminault6 in 1985, 34 of 35 patients were men, and half of the patients suffered from hypertension. Lavie states in a different study, “In years to come the association between sleep apnoea syndrome and the cardiovascular system could become the driving force behind sleep medicine.”11(p5)
The Control of Breathing
If our health is not affected by lung disease, our awareness of breathing is not top of mind, lying under the threshold of consciousness. We simply breathe automatically whether we are awake, asleep, or under anesthesia. Our notion is that we breathe in oxygen for life and we exhale carbon dioxide as a waste gas. It is broadly accepted that oxygen is the fuel of our body, and it is less well understood that carbon dioxide is not the presumed simple waste product but is as essential as oxygen. The fact of the matter is, as Appleyard has indicated, “[I]t turns out that under most circumstances, moment-to-moment control of breathing is to maintain a very stable level of carbon dioxide with the systemic arterial blood.”12(p2) The quantity and quality of ventilation are tightly regulated to maintain both oxygen and carbon dioxide levels within narrow limits and to minimize the work required to accomplish this.13
The rhythm, rate, and depth of breathing are determined by a complex set of feedback loops located in a group of specialized neurons in the brainstem. The dorsal respiratory group, named for its location in the medulla, is predominantly active during inspiration and determines the basic rhythm of respiration. The ventral respiratory group lies ventrally in the medulla and contains both inspiration and expiration neurons.14
Oxygen’s impact to alter respiration patterns is insignificant in comparison with carbon dioxide. For example, the normal Po2 is 90 to 95 mm Hg, and Pco2 is 40 mm Hg.12 It takes a significant drop in Po2 (below 60 mm Hg) to stimulate breathing; however, this is not true for Pco2.15 The slightest change in Pco2 will cause changes in ventilation.12 The Pco2 changes result in breathing variants such as Cheynes-Stokes respiration, hypoventilation, and chronic hyperventilation syndromes.
Breathing patterns are generated via a complex system of feedback loops involving peripheral chemoreceptors located in the carotid and aortic bodies that detect changes in arterial blood Po2 and Pco2 and pH.14 As mentioned earlier, of these 3 elements, Pco2 is the most significant. Although carbon dioxide levels are monitored by both central and the periphery chemoreceptors, there is an additional neuronal area, a chemosensitive location beneath the ventral surface of the medulla, that is highly sensitive to changes in either blood Pco2 or hydrogen ion concentrations.16 When carbon dioxide levels are low in arterial blood, the chemosensitive area or the respiratory center will slow the breathing rate. If carbon dioxide levels are high, the rate increases to blow off the excess.
In order to understand the concepts of respiration and its stability, a model using loop gain was created. To demystify the pieces, Dr John Brons, longtime professor of anatomy and physiology at National College of Natural Medicine (Portland, Oregon), kindly explained the variables of this new model. The terms loop gain, plant gain, and controller gain have explicit meanings. Loop gain, when high, describes the respiratory instability in response to a perturbation. Plant gain is the body’s response to increase ventilation to reduce elevated levels of Pco2. Controller gain is dependent upon the sensitivity of the respiratory center to make changes in Pco2.7 If a patient has a high loop, his or her response to a mild elevation in Pco2 would be with “sufficient ventilation to result in hypocapnia (‘over-shoot’), rather than simply bringing the system back to the original state (eucapnia).”7(p270) People with high loop gain have very unstable breathing patterns.
The rate of metabolic carbon dioxide production, rather than the rate of oxygen consumption, determines the link between metabolism and ventilation.12 The role of carbon dioxide in pH is that it is acidic, and if hypocapnia (low Pco2) occurs, the body experiences respiratory alkalosis. The body’s pH levels are stringently monitored by respiration to maintain levels as close to 7.4 at all times. Respiratory alkalosis leads to significant consequences such as restricting oxygen off-loading at the tissue level,17 as implied in the Bohr effect.
The delivery of oxygen to cells of the body requires hemoglobin as the carrier. The following factors facilitate the release of oxygen to the tissues: (1) decreased pH, (2) increased blood Pco2, (3) increased levels of 2-3-diphosphoglycerate, and (4) increased temperature.12
Bohr Effect and Hyperventilation
We are familiar with the oxygen-hemoglobin dissociation curve, otherwise known as the Bohr effect. This curve describes the affinity between hemoglobin and oxygen. The factor that is worth reviewing is that the level of carbon dioxide in arterial blood Pco2 determines the affinity of oxygen to hemoglobin. If Pco2 levels are low, the leftward shift causes oxygen to bind tightly to hemoglobin, and less oxygen is delivered to the tissues. A simple analogy to understand the Bohr effect is as follows: the more we breathe, the less oxygen is available, and the more breathless and hypoxic we become. In other words, when we hyperventilate, breathe deeply at rest, or even breathe through our mouth, carbon dioxide levels drop below normal, which increases blood pH to become more alkaline, in turn causing nerve and muscle cells to be irritable. Hyperventilation leads to a paradoxical sense of breathlessness, creating (inappropriately) a deeper and faster breath pattern with more hyperventilation. A vicious cycle ensues.18 Hyperventilation leads to hypocapnia, which leads to a direct effect on cerebral circulation. With respect to this cycle, Lum observed: “Hypocapnia causes immediate vasoconstriction leading to cerebral hypoxia.”19(p379) Low carbon dioxide leads to hypoxic conditions that result in a host of symptoms. Let us take a moment to pay especially close attention to sleep apnea.
There has been a surge of interest in recent years to understand the sleep stages and the respiratory cycle in its minute detail. When reviewing the literature of sleep medicine research, I was startled to discover that the equipment to study and monitor sleep and breathing has become indeed very sophisticated and complicated as devices aiding in determining respiration during sleep. My other discovery was that these researchers are so intent on studying breathing patterns during sleep that they have invariably lost the patient as a whole person in their searches. It is something like not seeing the forest for the trees. They do not, for example, study the relationship between breathing habits and sleep apnea itself. Before addressing that relationship, let us review the importance of breathing rate. May I propose, in fact, that breathing rates are the key to understanding and treating sleep apnea and breathing sleep disorders.
Although the human body is governed by normal values such as a body temperature of 37°C or 98.6°F, blood content, and other markers, breathing rates do not have a definitive normal value in the medical literature.20 However, every naturopathic and allopathic medical student studies the physiology of breathing. Let us pause for a short review.
The dorsal respiratory group generates the rhythm of our respiration. Guyton and Hall16 describe the inspiratory ramp signal and its determination of the breathing rhythm. They explain: “The nervous signal that is transmitted to the inspiratory muscles, mainly the diaphragm, is not an instantaneous burst of action potentials. Instead, in normal respiration, it begins weakly and increases steadily in a ramp manner for about 2 seconds. Then it ceases abruptly for approximately the next 3 seconds, which turns off the excitation of the diaphragm and allows elastic recoil of the lungs and the chest wall to cause expiration. Next, the inspiratory signal begins again for another cycle.”16(p505)
When the numbers are added up, the resting respiratory rate is about 12 breaths per minute. Dr Konstantin Buteyko, who spent 50 years of his life studying breathing, established definitively that a healthy breathing range was 8 to 12 breaths per minute. Recently, when faced with contradictory information regarding respiratory rate norms, I consulted an online medical site. The MD returned a reply quickly informing me that the normal respiratory rate in a healthy person is 15 to 25 breaths per minute, confirming the norms forwarded by a nursing colleague. These values do not coincide with physiology textbooks nor with patients who struggle with sleep apnea. We need to revisit why there is so much variation in defining the healthy normal respiratory rate in adults at rest, from 12 to 24 breaths per minute for younger individuals and from 16 to 25 in the elderly.21 The connection between hyperventilation and stress is a critical one for physicians to review.
Our breathing during the day has a huge impact on our breathing at night. In the 1980s, researchers were conducting experiments on chronic hyperventilation syndrome and stress, which manifested symptoms in any organ or in any body system. Dubbed as the “fat folder syndrome,” patients would travel from physician to physician in search of a diagnosis and treatment of a number of symptoms that seemed completely unrelated. Consequently, the patient saw many specialists and had a thick case file. Chronic hyperventilation became that diagnosis.19
The Himalayan Institute also studied the rising epidemic of stress; Nuernberger redefined stress as “a state of prolonged arousal of the sympathetic nervous system and expanded the concept to include overdominance of the parasympathetic system.”22(p11) The sympathetic nervous system stimulates inhalation, and the passive exhale is under the parasympathetic control. The sympathetic-driven breathing pattern that arises from “fight or flight” is predominantly thoracic breathing. The desired breathing pattern is diaphragmatic. Nuernberger explains, “The respiratory rate is far lower for diaphragmatic dominated breathing than for thoracic dominated breathing.”22(p12)
The relationship between the autonomic nervous system and breathing can be triggered by stress. A hyperventilation provocation test was used, and subjects were asked to hyperventilate; within 2 to 3 minutes, symptoms associated with hyperventilation would occur.23 Hyperventilation or voluntary overbreathing can reduplicate symptoms within a few seconds to a few minutes.19 If a provocation test can cause symptoms related to hyperventilation at 18 breaths per minute, it is worrisome that allopathic medicine is not quite sure what a healthy breathing rate is.
The hyperventilation experienced during the day by patients with sleep apnea is, in fact, not studied by sleep clinics. Classically defined, “hyperventilation syndrome is a condition in which minute ventilation exceeds metabolic demands resulting in hemodynamic and chemical changes.”24 Cluff reports that “hyperventilation [or overbreathing] is a perfectly normal reaction to stress.”25(p855) The presentation of hyperventilation is diverse. Breathing that is rapid or irregular, sighing respirations with widely varying tidal volumes, and, in particular, excessive thoracic movements are signs of hyperventilating.23 Other manifestations of hyperventilation include mouth breathing and yawning.
The Himalayan Institute conducted a survey of 153 patients in an intensive coronary care unit.26 The findings showed that all patients exhibited the dominant pattern of thoracic breathing both in the waking and the sleeping states. Seventy-fix percent of the myocardial infarction patients habitually breathed through the mouth. Of those who were mouth breathers, 70% exhibited consistent open-mouth snoring. Significantly, none of the nose breathers manifested either open-mouth snoring or apnea. Nuernberger27 concludes that thoracic or chest breathing is associated with sympathetic arousal and thoracic breathing patterns.
Cluff,25 who studied chronic hyperventilation, concluded that hyperventilation caused an excessive amount of carbon dioxide to be lost during exhalation. He noted, “A single deep breath may cause a momentary fall of 20-25% in the level of carbon dioxide in the blood, while sustained over breathing can rapidly drop it to half and maintain it at this level.”25(p855) As Cluff further indicates, hyperventilation leads to erratic breathing patterns that cause wildly fluctuating Pco2.25 If it is as simple as one deep breath disrupting carbon dioxide levels and breathing patterns during the day, surely at night sleep apnea is simply taking stress to bed.
When stress is not in the picture, our breathing when we go to bed slows down, causing minute ventilation to decrease because of a reduction in tidal volume and breathing rate. Cherniack concludes, “During all stages of sleep there is a decrease in the tone of most skeletal muscles that seems to partly spare the diaphragm.”10(p326) Our breathing during healthy sleep is slower, and the depth of breathing is reduced less than when we are awake. If hyperventilation occurs during our stressful days, it continues into the night during sleep.
Conventional Treatment
Sleep apnea has evolved into a huge business, involving hundreds of sleep study clinics for the purpose of diagnosing and treatment, which in turn involves the sale of equipment and supplies and recurrent drug prescriptions. According to a colleague, hundreds of sleep studies occur in our town every night, and the general outcome of these nightly stays is the prescription of a device such as the continuous positive airway pressure (CPAP). Until the introduction of the CPAP in 1981 by Sullivan and associates, who revolutionized the treatment of OSA,1 tracheostomy had been considered to be the only effective therapy for sleep apnea.10 The patient enrolls in the sleep clinic and may watch a video to soften the impact of the actual sleep study. The video shows patients what the procedure entails and what kind of CPAP devices are available. Having had the opportunity to preceptor in a sleep laboratory, I could not help but think that the patient’s respiration was not only being monitored but also the whole patient was being prepared for the purchase of a CPAP machine. The sleep study is routinely conducted with the patient laying on his or her back, predisposing a night of snoring and sleep apnea.
The 3 major components of monitoring respiration during sleep include measurement of airflow, measurement of respiratory effort, and measurement of arterial oxygen saturation.7 Polysomnography has become the current standard for evaluating sleep apnea and other sleep-related dysfunctional breathing, which is established with the use of “electroencephalographic, electro-oculographic, and submental (chin) electromyographic criteria.”7(p661) Characteristic patterns from the electrodes are recorded when the patient is awake with his or her eyes closed, as well as during sleep. The duration of time taken to fall asleep, time to enter REM sleep, any movements, breathing pattern, and sleep architecture are all recorded using a computer. Less than 50% of patients meeting polysomnographic criteria for OSA complain of sleepiness, which is the usual indication for therapy.28 Young et al produced a landmark study when examining the frequency of episodes of apnea and hypopnea in men and women; their findings showed that “the prevalence of undiagnosed sleep disordered breathing is high among men and is much higher than previously suspected among women.”28(p1230)
As an ND student 20 years ago, I was aware that sleep apnea was just emerging as a condition. One treatment I became aware of in the 1990s involved sewing a ping-pong ball into the back of a garment worn at night such as the back of the pajama top. Little did I know then that this was exactly what the early 20th-century NDs prescribed. The current and most prevalent option for sleep apnea is a CPAP device, which is invasive and disruptive to those who have to wear them, or surgery. Not coincidentally (in my view), the CPAP forces the wearer to breathe nasally, a step in the right direction, albeit mechanistic and reductionist in the extreme. The long-term compliance rate for the CPAP is poor. Naturopathic medicine has alternative, noninvasive approaches that do not include high-cost apparatus or recurrent drug expenditures. We can help patients restore a healthy breathing pattern during the day with breathing exercises so that they are breathing correctly at night. May I suggest a number of questions to assist in assessment, followed by a brief introduction to the noninvasive therapeutic breathing approach called “the Buteyko method”? Observe your patients and see how are they breathing: (1) Are they breathing with their diaphragm or chest muscles? (2) Is their breathing noisy and audible? (3) Do they sigh or yawn a lot? (4) Are they breathing with their nose or mouth? When listening to a patient’s breathing, is his or her mouth open? (5) Do the mouth breathers use chapped lip or lipstick products? (6) What is the patient’s respiratory rate per minute?
Dr Konstantin Buteyko
Buteyko breathing exercises teach people with sleep apnea to take charge of their breathing at night. Peter Kolb, an engineer and a long-time advocate of Buteyko breathing, writes: “Buteyko therapy simply reverses this process [sleep apnea] by relaxation of the respiratory muscles accompanied by deliberate volitional reduction in breathing over time.”29(p). Snoring decreases Pco2, which is followed by apnea, and the body waits to build up adequate Pco2 that signals lungs to take another breath.
Dr Buteyko spent 50 years of his professional life studying breathing and developing breathing exercises to counteract the effects of stress and hyperventilation. Buteyko himself comments: “On this basis the method of volitional normalization of deep-type breathing or the method of volitional control has been developed. The essence of this technique is that a patient, by the exertion of will, deliberately diminishes the respiratory depth by relaxing the respiratory muscles till he feels a slight deficit of air. The method can be assimilated by adults who do not suffer mental disorders and by children aged above three.”30(p3)
Dr Buteyko treated over 100 000 patients with his deliberate volitional breathing method (DVBM). Buteyko trained many MDs in his approach, noting that a common mistake for beginners learning DVBM was that they “restrict the depth of breathing not by relaxation but by tension, which as a rule aggravates their condition.”31(p60) Rather, as pointed out by Souliagin,31 there are 3 rules for DVBM: (1) Reduce the volume of air during inhalation so that a slight hunger of air is felt. (2) The exhalation is effortless, requiring no muscular control. (3) Let your body feel as relaxed as possible. Buteyko proposed that “Any skeletal muscle tension leads to the breath deepening.”31(p60)
Another observation made by Buteyko breathing educators about snorers and those with sleep apnea is that they are prone to mouth breathing at night and often sleep on their backs. Buteyko prescribed nasal breathing at all times. He advocated sealing the mouth at night, along with the DVBM exercises, as great remedies for snoring.32 To seal the mouth, paper surgical tape (0.5-in size) or 3M surgical tape is recommended. The tape used is about 3-in long, with one end folded over to make a small tab. The patient places the tape diagonally across the mouth before retiring to bed. Caution is needed in the morning when removing the tape because the adhesive over night becomes very tacky and adheres to the skin. Patients are cautioned to peel off the night tape very slowly and carefully.
Shut Your Mouth and Save Your Life
Another who observed the consequences of sleeping on the back and mouth breathing was George Catlin. Catlin, famous for his paintings of the First Nation’s people in the mid-19th century, began his career as a lawyer, did a 180-degree turn, and became an ethnographer and painter.33 He wrote Shut Your Mouth and Save Your Life in 1870 (available online at Google books), which records his responses to what he described as “the deplorable mortality, the numerous diseases and deformities, in [supposedly] civilized communities.”34(p1) The mortality of children in densely populated urban areas was atrocious, for example, in the mid-19th century. He reported: “In London and other large towns in England, and cities of the Continent, on an average, one half of the human Race die before they reach the age of five years, and one half of the remainder die before they reach the age of twenty five, thus leaving but one in four to share the chances of lasting from the age of twenty-five to old age.”34(p2)
These realities in the civilized world so alarmed him that Catlin decided to study indigenous populations as a contrast and as a potential source of answers to this tragic human circumstance. He traveled throughout preindustrial Canada, the American subcontinent with its states and territories, and South America, eventually visiting 150 tribes and coming into contact with 2 million people whom he described as follows: “Living in their primitive State, and practicing their native modes, I offer myself as a living witness, that whilst in that condition, the Native Races in North and South America are a healthier people, and less subject to premature mortality (save from the accidents of War and the Chase, and also from Small-pox and other pestilential diseases introduced amongst them), than any Civilized Race in existence.”34(p3)
Among other characteristics of their lifestyles, Catlin observed that the civilized were primarily mouth breathers and that they had a number of diseases correlated to this kind of breathing pattern. The detail of his observations drilled down even to notes about snoring: “Most often I observed these urban dwellers breathing through t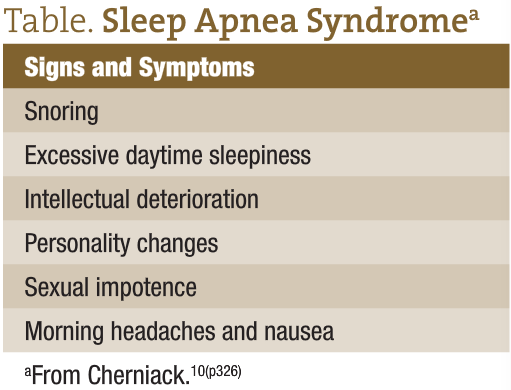 he mouth, which is generally the cause of snoring.”34(p8)
he mouth, which is generally the cause of snoring.”34(p8)
Buteyko researchers have developed a number of taxonomies related to breathing habits. Among these observations, they have noted the following symptoms associated with mouth breathing described: oral cavities, enlarged tonsils and tonsillitis, crooked teeth, sleep disorders (snoring, sleep apnea, urination during the night, nightmares, waking unrefreshed, and dry mouth), receding chin, facial deformities, bad breath, nasal congestion, and sinusitis (nasal breathing promotes nitric oxide). A related list by Cherniack10 of signs and symptoms associated with sleep apnea is also worth noting (Table).
Conclusion
The expansion of research about problems our patients are having with sleep has contributed abundant new ideas and tools to treat these disorders. It may well be, however, that the complex equipment, pharmaceuticals, and surgery that have been introduced into the treatment protocols and approaches can be softened considerably for patients with a whole-person approach, which begins with breath training such as Buteyko. What is clear is that, in an age where environmental toxicity and lifestyle stress are driving more and more individuals to sleep clinics, the sheer momentum and volume of presentations demand more effective, less invasive, less expensive, and less reductionist approaches to helping people not take their stress to bed at night.

Dr Sussanna Czeranko ND BBE
Sussanna Czeranko, ND, BBE a naturopathic physician licensed in Ontario, Canada, and in Oregon practicing since 1994 incorporates “nature cure” approaches systematically into primary care by including balneotherapy, breathing therapy, and nutrition. As the rare books curator at National College of Natural Medicine, Portland, Oregon, she is currently compiling an 11-volume series titled In Their Own Words, based on the Benedict Lust journals published early in the last century. As the founder of the Breathing Academy, a training institute for NDs, she facilitates the incorporation of the scientific model of breathing therapy called Buteyko into their practices.
References
1. Bradley TD. Respiratory sleep medicine: a coming of age. Am J Respir Crit Care Med. 2008;177:363-364.
2. Young T, Skatrud J, Peppard PE. Risk factors for obstructive sleep apnea in adults. JAMA. 2004;291(16):2013-2016.
3. A brief history of sleep research. Updated February 3, 1999. http://www.stanford.edu/~dement/history.html. Accessed January 15, 2013.
4. Randall D. On how animals sleep, the real Olympic advantage, and why men rest easy: David Randall in conversation with Brian Bethune. Maclean’s Magazine. 2012;125(31):13.
5. Institute of Medicine. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. Washington, DC: National Academies Press; 2006.
6. Guilleminault C. Sleep apnea: the clinical syndrome and historical perspective. Med Clin North Am. 1985;69:1187-1203.
7. Berry RB. Fundamentals of Sleep Medicine. Philadelphia, PA: Elsevier Saunders; 2012:101, 237, 270, 382, 661.
8. Malhotra A, Owens RL. What is central sleep apnea? Respir Care. 2010;55(9):1168-1178.
9. Dempsey JA, Veasey SC, Morgan BJ, O’Donnell CP. Pathophysiology of sleep apnea. Physiol Rev. 2010;90:47-112.
10. Cherniack NS. Respiratory dysrhythmias during sleep. N Engl J Med. 1981;305(6):325-330.
11. Lavie P. Who was the first to use the term Pickwickian in connection with sleepy patients? History of sleep apnoea syndrome. Sleep Med Rev. 2008;12(1):5-17.
12. Appleyard RF. Respiratory Physiology. Chicago, IL: National University of Health Sciences; 2006:2, 9, 16, 48.
13. White DP. Pathogenesis of obstructive and central sleep apnea. Am J Respir Crit Care Med. 2005;172(11):1363-1370.
14. Rhoades RA. The control of ventilation. In: Rhoades RA, Tanner GA, eds. Medical Physiology. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2003:364, 369.
15. Carroll RG. Elsevier’s Integrated Physiology. Philadelphia, PA: Elsevier & Mosby; 2007:113.
16. Guyton AC, Hall JE. Textbook of Medical Physiology. Philadelphia, PA: Elsevier Saunders; 2011:505, 507.
17. Laffey JG, Kavanagh BP. Carbon dioxide and the critically ill: too little of a good thing? Lancet. 1999;354(9186):1283-1286.
18. Clarke J. Resting breath pattern II. Res Bull Himalayan Int Inst. 1981;2(2):10-11.
19. Lum LC. Hyperventilation: the tip and the iceberg. J Psychosom Res. 1975;19(5-6):375-383.
20. Cretikos MA, Bellomo R, Hillman K, Chen J, Finfer S, Flabouris A. Respiratory rate: the neglected vital sign. Med J Aust. 2008;188:657-659.
21. McFadden JP, Price RC, Eastwood HD, Briggs RS. Raised respiratory rate in elderly patients: a valuable physical sign. Br Med J. 1982;284:626-627.
22. Nuernberger P. Stress II. Res Bull Himalayan Int Inst. 1981;3(3-4):11-12.
23. Lum LC. Hyperventilation and anxiety state. J R Soc Med. 1981;74(1):1-4.
24. Kern B, Rosh AJ. Hyperventilation syndrome. 2009. eMedicine. Emedicine.medscape.com.25. Cluff RA. Chronic hyperventilation and its treatment by physiotherapy: discussion paper. J R Soc Med. 1984;77(10):855-862.
26. Hymes A, Nuernberger P. Breathing patterns found in heart attack patients. Res Bull Himalayan Int Inst. 1980;2(2):10-11.
27. Nuernberger P. Therapeutic value of breath. Res Bull Himalayan Int Inst. 1979;Inaugural Issue, Fall:11.
28. Young T, et al. p. 1230-5.
29. Kolb P. Summary of Buteyko’s theory on asthma. 2001. http://www.buteyko.ie/images/pdf/Kolb_P_(2001)_Summary_of_Buteykos_Theory_on_Asthma.pdf. Accessed January 16, 2013.
30. Buteyko KP. Basic principles of Buteyko therapy. http://www.members.westnet.com.au/pkolb/but_bov.htm. Accessed January 15, 2013.
31. Souliagin SS. Common mistakes observed while using DVBM. http://www.members.westnet.com.au/pkolb/souliagi.htm. Accessed January 16, 2013.
32. Buteyko KP. Sealing up the mouth. In: Buteyko’s Book. http://www.buteyko.ie/images/pdf/Dr_Buteykos_Book.pdf. Accessed January 16, 2013.
33. Stool SE. (1983). George Catlin on mouth breathing. Trans Stud Coll Physicians Phila. 1983;5(2):123-128.
34. Catlin G. Shut Your Mouth and Save Your Life. London, England: N. Truebner & Co; 1870:1-3, 8.










