Mycotoxins and Men
LAUREN TESSIER, ND
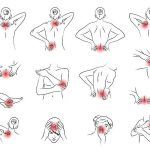
Healthcare accessibility and delivery is an important issue in our current conversation. The disparities between cohorts and their healthcare utilization have been deeply studied; various minority groups suffer at the hand of poor healthcare delivery; of this there is no debate.1,2 To add an extra layer of complication, the male sex, which accounts for approximately 50.4% of the global population,3 fail to seek care as often as the female sex.4 Researchers postulate that projected societal concepts of masculine roles and ideology have a profound effect on male healthcare utilization.5 This concerning paradigm of healthcare inequality does not exist in the vacuum of primary care and emergency services; take my mold and environmental medicine specialty practice, for example: men account for only 16% of my patient population. Consider for a moment this number, in conjunction with the claims that anywhere from 50%6 to 68%7 of homes in the United States present with some form or sign of dampness or water damage. Moreover, 85% of commercial buildings studied by the EPA demonstrated a history of water damage, while 45% demonstrated current water damage.8 Needless to say, when only 16% of care is delivered to men, we not only need to wonder why, but we also need to be at the ready to assist any man who may be struggling as a result of exposure. While men may suffer from the commonplace mold-illness symptoms of fatigue, brain fog, myalgia, GI distress, joint pain, and immune system dysregulation, etc, they may also experience complaints arising from the disruption of the male endocrine system.
Mycotoxins & the Endocrine System
While it is well known that mycotoxin exposure results in oxidative damage to tissues, one must be mindful of the other means by which mycotoxins can wreak havoc in the human system. Research has demonstrated disruptive effects of mycotoxins on the endocrine system, including aberrant functionality as a result of altered metabolism of endogenous hormones.9-11 Not only does this disruption occur via anabolism11; it also occurs in the catabolic process. Animal studies have demonstrated that mycotoxins are capable of altering components of both Phase 1,12-14 and Phase 2 detox pathways.15-23 As endogenous hormones are catabolized by such pathways, it is possible that mycotoxins are therefore able to alter their metabolism, resulting in elevated levels of hormones and/or partially metabolized hormonal products. While metabolism is important to consider, one should also be aware of aberrant hormonal signaling that may arise from mycotoxin exposure. Research has demonstrated the ability of mycotoxins to alter nuclear receptor transcription10,24 as well as receptor stimulation and blockade.25 Given the ubiquitous nature of mycotoxins – both in our food26 and the built environment27-30 – and with the possibility of systemic exposure as a result of consumption,31 inhalation,32-34 or transdermal exposure,35-36 clinicians should be at the ready to address mold illness in the general population.
Mycotoxins & Testosterone
As one-half of our population has a system that largely depends on proper testosterone balance, one needs to be mindful of the ways in which mold exposure can appear clinically in this cohort. Testosterone is responsible for numerous bodily functions, including sexual differentiation, muscle, bone and body mass, and other less obvious processes, such as erythropoiesis.37 Proper testosterone balance is clearly necessary for overall health, as evidenced by research demonstrating correlations between reduced testosterone levels and increased morbidity and mortality in men.38
Testosterone and androgen deficiency may manifest as complaints of low libido, decreased body hair, gonadal atrophy, infertility, decreased occurrence of spontaneous erections, sleep difficulties, failure to develop secondary sex characteristics, osteopenia or osteoporosis, fatigue, gynecomastia, muscle mass reduction, climacteric events, depressed mood, cognitive difficulties, anemia, obesity, and decreased stamina and strength.39 Testosterone is produced primarily by the testicular Leydig cells,40 with a smaller portion produced by the adrenal glands.41 Studies have demonstrated that some mycotoxins interfere with the functionality of the 17-beta-hydroxysteroid dehydrogenase class of enzymes,11 which are required for proper androgenic metabolism, including testosterone production. Moreover, animal research suggests that Leydig cell testosterone production is negatively impacted by mycotoxins such as enniatin b,42 zearalenone,43,44 ochratoxin A,44 citrinin,44-46 T-2,44,47 and cytochalasin B.48 Furthermore, animal ancillary adrenal testosterone production is reduced in the presence of enniatin b42 and zearalenone.10
While systemic testosterone levels are demonstrably reduced in animals exposed to zearalenone,43 and T-2,49-52 production and systemic levels of androgenic hormones are not the only factors complicated by mycotoxin exposure. Animal research has shown that mycotoxins such as beauvericin, deoxynivalenol, and zearalenone and their metabolites act antagonistically at androgen receptors.53,54 Moreover, as the United States slides slowly into the void of estrogen dominance as a result of xenoestrogen exposure, we should not turn a blind eye to the estrogenic effects of mycotoxins on the male system. One of the most well-known xenoestrogenic mycotoxins is zearalenone and its family of metabolites.53 Their ability to stimulate estrogen receptors55,56 is a result of their structural resemblance to 17-beta-estradiol.57 Similar to zearalenone and its metabolites, the deoxynivalenol metabolite, 3-acetyl-deoxynivalenol, also acts agnostically at the estrogen receptor.53 Further complicating the estrogen and testosterone balance, zearalenone and its metabolites are not only able to stimulate receptors, but may also promote an increase in adrenal cortical estradiol production.10
Mold Exposure & Male Fertility
It is estimated that approximately 2.5-12% of the male population is infertile, with the highest rates occurring in Europe and Africa.58 With infertility on the rise, one should be careful to consider the possible etiology, including environmental exposure. It has been suggested in the literature59 that mycotoxins could be the cause of infertility in some countries where foodborne exposure is elevated. In fact, 2 studies of infertile men have demonstrated elevated levels of aflatoxin in their semen, compared to fertile controls.60,61 Such suggestions are not unfounded, as we know that Leydig cells are impacted by mycotoxin exposure. As these cells are responsible for testosterone production, they are also imperative to spermatogenesis. Animal studies have confirmed altered functionality and even cytotoxic effects in Leydig cells as a result of exposure to the mycotoxins citrinin,45 deoxynivalenol,62 ochratoxin A,62 T-2,47,63-68 aflatoxin,40,69 and zearalenone.70-73 Also necessary for spermatogenesis are the Sertoli cells, which have been documented in animal studies to be negatively affected by citrinin,74 fumonisin B1,75 ochratoxin A,76 T-2,77 and zearalenone.78-82 Moreover, the animal literature clearly documents altered in-vivo spermatogenesis in animals exposed to zearalenone,83,84 T-2,85 ochratoxin A,86 patulin,87 fumonisin B1,88-90 deoxynivalenol,91 citrinin,46 and aflatoxin B1.92-93 Reductions in viable sperm count have also been documented in animals exposed to zearalenone,94 deoxynivalenol,91,95 and T-2.49,50,96 Decreased motility in the presence of ochratoxin A,82 zearalenone,43,94 T-2,49,51,85 and other trichothecenes97 – and, in some instances, even germ cell apoptosis96 – have also been documented. Many of these changes have been reported in conjunction with testicular atrophy in animals exposed to zearalenone,83,98 and T-2.96
Increased Susceptibility & Protection
Animal studies suggest that unique susceptibility to mycotoxicity should be considered in the male population. For example, male rodents have demonstrated a reduced ability to renally clear deoxynivalenol from the system.99,100 Studies have shown elevated plasma and organ concentrations of deoxynivalenol in male rodents,101 without clear correlation to any sex-related variances in the major mechanism of detoxification via glucuronidation.99 While it is unclear whether the same findings apply to male humans or to other mycotoxins, it is still a point that should be considered when navigating the clinical approach to and prognosis of male clients. That said, we are aware that there are sex-correlated dimorphic differences in the human expression of Phase 1 pathways such as CYP3A5,102 CYP3A4,103,104 and CYP1A2.103 This is an important consideration, as we are aware that many mycotoxins are metabolized by some of these same pathways (keeping in mind that some of these pathways also result in intermediates that increase cytotoxicity)105; examples include: aflatoxin B1, which in humans is metabolized by human CYP1A2,105 -3A4,105,106 -2B1,107 -2c11,107 -3A1,107 -3A2,107 and -2A1106; ochratoxin A, which is metabolized by CYP1A1, -1A2, -2C9, and -3A4108; ennantin B, which is metabolized by CYP3A4, -1A2, and -2C1912; and aflatoxin G1, which is metabolized by CYP1A2, -3A5, and -3A4.198,110
Some animal studies demonstrate the protective role of testosterone in response to mycotoxin-induced damage; this includes the hormone’s protective role in cases of T-2-toxin-induced adrenocortical necrosis111 and aflatoxin-induced RBC hemolysis.112 On the other hand, animal studies also demonstrate that testosterone may be related to an increased incidence of deoxynivalenol-induced IgA nephropathy113,114 and anorexia,115 and also ochratoxin-induced liver and kidney damage.116 These findings are not limited to animal studies, as a human cohort study demonstrated a correlation between plasma ochratoxin A levels and C-reactive protein and cardiovascular risk score in men, though not in women.117
While much of this information comes from animal research – as does most of the mycotoxin literature – it does raise some interesting considerations regarding the management of our male clients, especially those suffering from mycotoxin exposure.
References:
- Hardeman RR, Murphy KA, Karbeah J, Kozhimannil KB. Naming Institutionalized Racism in the Public Health Literature: A Systematic Literature Review. Public Health Rep. 2018;133(3):240-249.
- Ben J, Cormack D, Harris R, Paradies Y. Racism and health service utilisation: A systematic review and meta-analysis. PLoS One. 2017;12(12):e0189900
- Ritchie H, Roser M. Gender Ratio. June 2019. OurWorldInData.org. Available at: https://ourworldindata.org/gender-ratio. Accessed August 16, 2020.
- Schlichthorst M, Sanci LA, Pirkis J, et al. Why do men go to the doctor? Socio-demographic and lifestyle factors associated with healthcare utilisation among a cohort of Australian men. BMC Public Health. 2016;16(Suppl 3):1028.
- Himmelstein MS, Sanchez DT. Masculinity impediments: Internalized masculinity contributes to healthcare avoidance in men and women. J Health Psychol. 2016;21(7):1283-1292.
- Spengler JD, Jaakkola JJ, Parise H, et al. Housing characteristics and children’s respiratory health in the Russian Federation. Am J Public Health. 2004;94(4):657-662.
- Maier WC, Arrighi HM, Morray B, et al. Indoor risk factors for asthma and wheezing among Seattle school children. Environ Health Perspect.1997;105(2):208-214.
- Girman JR, Baker BJ, Burton LE. Prevalence of Potential Sources of Indoor Air Pollution in U.S. Office Buildings. Proceedings of Indoor Air. 2002(9):438-443.
- Pfeiffer E, Diwald TT, Metzler M. Patulin reduces glutathione level and enzyme activities in rat liver slices. Mol Nutr Food Res. 2005;49(4):329-336.
- Frizzell C, Ndossi D, Verhaegen S, et al. Endocrine disrupting effects of zearalenone, alpha- and beta-zearalenol at the level of nuclear receptor binding and steroidogenesis. Toxicol Lett. 2011;206(2):210-217.
- Krazeisen A, Breitling R, Möller G, Adamski J. Phytoestrogens inhibit human 17beta-hydroxysteroid dehydrogenase type 5. Mol Cell Endocrinol. 2001;171(1-2):151-162.
- Fæste CK, Ivanova L, Uhlig S. In vitro metabolism of the mycotoxin enniatin B in different species and cytochrome p450 enzyme phenotyping by chemical inhibitors. Drug Metab Dispos. 2011;39(9):1768-1776.
- Osselaere A, Li SJ, De Bock L, et al. Toxic effects of dietary exposure to T-2 toxin on intestinal and hepatic biotransformation enzymes and drug transporter systems in broiler chickens. Food Chem Toxicol. 2013;55:150-155.
- Meissonnier GM, Laffitte J, Loiseau N, et al. Selective impairment of drug-metabolizing enzymes in pig liver during subchronic dietary exposure to aflatoxin B1. Food Chem Toxicol. 2007;45(11):2145-2154.
- Limonciel A, Jennings P. A review of the evidence that ochratoxin A is an Nrf2 inhibitor: implications for nephrotoxicity and renal carcinogenicity. Toxins (Basel). 2014;6(1):371-379.
- Dai C, Xiao X, Sun F, et al. T-2 toxin neurotoxicity: role of oxidative stress and mitochondrial dysfunction. Arch Toxicol. 2019;93(11):3041-3056.
- Chaudhary M, Rao PVL. Brain oxidative stress after dermal and subcutaneous exposure of T-2 toxin in mice. Food Chem Toxicol. 2010;48(12):3436-3442.
- Ramyaa P, Krishnaswamy R, Padma VV. Quercetin modulates OTA-induced oxidative stress and redox signalling in HepG2 cells – up regulation of Nrf2 expression and down regulation of NF-κB and COX-2. Biochim Biophys Acta. 2014;1840(1):681-692.
- Huang L, Duan C, Zhao Y, et al. Reduction of Aflatoxin B1 Toxicity by Lactobacillus plantarum C88: A Potential Probiotic Strain Isolated from Chinese Traditional Fermented Food “Tofu.” PLoS One. 2017;12(1):e0170109.
- Guerre P, Eeckhoutte C, Burgat V, Galtier P. The effects of T-2 toxin exposure on liver drug metabolizing enzymes in rabbit. Food Addit Contam. 2000;17(12):1019-1026.
- Yılmaz S, Kaya E, Comakli S. Vitamin E (α tocopherol) attenuates toxicity and oxidative stress induced by aflatoxin in rats. Adv Clin Exp Med. 2017;26(6):907-917.
- Choi KC, Chung WT, Kwon JK, et al. Chemoprevention of a flavonoid fraction from Rhus verniciflua Stokes on aflatoxin B1-induced hepatic damage in mice. J Appl Toxicol. 2011;31(2):150-156.
- Yilmaz S, Kaya E, Karaca A, Karatas O. Aflatoxin B1 induced renal and cardiac damage in rats: Protective effect of lycopene. Res Vet Sci. 2018;119:268-275.
- Marketon JI, Sternberg EM. The glucocorticoid receptor: a revisited target for toxins. Toxins (Basel). 2010;2(6):1357-1380.
- Rogowska A, Pomastowski P, Sagandykova G, Buszewski B. Zearalenone and its metabolites: Effect on human health, metabolism and neutralisation methods. Toxicon. 2019;15(162):46-56.
- Marin S, Ramos AJ, Cano-Sancho G, Sanchis V. Mycotoxins: occurrence, toxicology, and exposure assessment. Food Chem Toxicol. 2013;(60):218-237.
- Salo MJ, Marik T, Mikkola R, et al. Penicillium expansum strain isolated from indoor building material was able to grow on gypsum board and emitted guttation droplets containing chaetoglobosins and communesins A, B and D. J Appl Microbiol. 2019;127(4):1135-1147.
- Bennett JW, Inamdar AA. Are Some Fungal Volatile Organic Compounds (VOCs) Mycotoxins? Toxins (Basel). 2015;7(9):3785-3804.
- Bloom E, Grimsley LF, Pehrson C, et al. Molds and mycotoxins in dust from water-damaged homes in New Orleans after hurricane Katrina. Indoor Air. 2009;19(2):153-158.
- Brasel TL, Martin JM, Carriker CG, et al. Detection of airborne Stachybotrys chartarum macrocyclic trichothecene mycotoxins in the indoor environment. Appl Environ Microbiol. 2005;71(11):7376-7388.
- Oyelami OA, Maxwell SM, Adelusola KA, et al. Aflatoxins in the autopsy brain tissue of children in Nigeria. Mycopathologia.1995;132:35-38.
- Thurman JD, Creasia DA, Trotter RW. Mycotoxicosis caused by aerosolized T-2 toxin administered to female mice. Am J Vet Res. 1988;49(11):1928-1931.
- Creasia DA, Thurman JD, Jones LJ 3rd, et al. Acute inhalation toxicity of T-2 mycotoxin in mice. Fundam Appl Toxicol. 1987;8(2):230-235.
- Creasia DA, Thurman JD, Wannemacher RW Jr, Bunner DL. Acute inhalation toxicity of T-2 mycotoxin in the rat and guinea pig. Fundam Appl Toxicol. 1990;14(1):54-59.
- Kemppainen BW, Riley RT, Pace JG. Skin Absorption as a Route of Exposure for Aflatoxin and Trichothecenes. Journal of Toxicology: Toxin Reviews. 1988;7(2):95-120.
- Boonen J, Malysheva SV, Taevernier L, et al. Human skin penetration of selected model mycotoxins. Toxicology. 2012;301(1-3):21-32.
- Bhasin S, Jasuja R. Reproductive and Nonreproductive Actions of Testosterone. Enc Endocr Dis. 2019;2:721-734.
- Cunningham GR, Toma SM. Clinical review: Why is androgen replacement in males controversial? J Clin Endocrinol Metab. 2011;96(1):38-52.
- Bhasin S, Cunningham GR, Hayes FJ, et al. Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2010;95(6):2536-2559.
- Adedara IA, Nanjappa MK, Farombi EO, Akingbemi BT. Aflatoxin B1 disrupts the androgen biosynthetic pathway in rat Leydig cells. Food Chem Toxicol. 2014;65:252-259.
- Antoniou-Tsigkos A, Zapanti E, Ghizzoni L, et al. Adrenal Androgens. Last updated January 5, 2019. Endotext. Available at: https://www.ncbi.nlm.nih.gov/books/NBK278929. Accessed August 16, 2020.
- Kalayou S, Ndossi D, Frizzell C, et al. An investigation of the endocrine disrupting potential of enniatin B using in vitro bioassays. Toxicol Lett. 2015;233(2):84-94.
- Del Fabbro L, Jesse CR, de Gomes MG, et al. The flavonoid chrysin protects against zearalenone induced reproductive toxicity in male mice. Toxicon. 2019;165:13-21.
- Fenske M, Fink-Gremmels J. Effects of fungal metabolites on testosterone secretion in vitro. Arch Toxicol. 1990;64(1):72-75.
- Liu S, Wang D, Zhang J, et al. Citrinin reduces testosterone secretion by inducing apoptosis in rat Leydig cells. Toxicol In Vitro. 2012;26(6):856-861.
- Qingqing H, Linbo Y, Yunqian G, Shuqiang L. Toxic effects of citrinin on the male reproductive system in mice. Exp Toxicol Pathol. 2012;64(5):465-469.
- Yang J, Zhang Y, Jing A, et al. Effects of T-2 toxin on testosterone biosynthesis in mouse Leydig cells. Toxicol Ind Health. 2014;30(10):873-877.
- Murono EP, Lin T, Osterman J, Nankin HR. The effects of cytochalasin B on testosterone synthesis by interstitial cells of rat testis. Biochim Biophys Acta. 1980;633(2):228-236.
- Wu J, Yang C, Liu J, et al. Betulinic Acid Attenuates T-2-Toxin-Induced Testis Oxidative Damage Through Regulation of the JAK2/STAT3 Signaling Pathway in Mice. Biomolecules. 2019;9(12):787.
- Yang JY, Zhang YF, Liang AM, et al. Toxic effects of T-2 toxin on reproductive system in male mice. Toxicol Ind Health. 2010;26(1):25-31.
- Kovács M, Tornyos G, Matics Z, et al. Subsequent effect of subacute T-2 toxicosis on spermatozoa, seminal plasma and testosterone production in rabbits. Animal. 2011;5(10):1563-1569.
- Kovács M, Tornyo G, Matics Z, et al. Effect of chronic T-2 toxin exposure in rabbit bucks, determination of the No Observed Adverse Effect Level (NOAEL). Anim Reprod Sci. 2013;137(3-4):245-252.
- Demaegdt H, Daminet B, Evrard A, et al. Endocrine activity of mycotoxins and mycotoxin mixtures. Food Chem Toxicol. 2016;96:107-116.
- García-Herranz V, Valdehita A, Navas JM, Fernández-Cruz ML. Cytotoxicity against fish and mammalian cell lines and endocrine activity of the mycotoxins beauvericin, deoxynivalenol and ochratoxin-A. Food Chem Toxicol. 2019;127:288-297.
- Kowalska K, Habrowska-Górczyńska DE, Piastowska-Ciesielska AW. Zearalenone as an endocrine disruptor in humans. Environ Toxicol Pharmacol. 2016;48:141-149.
- Malekinejad H, Colenbrander B, Fink-Gremmels J. Hydroxysteroid dehydrogenases in bovine and porcine granulosa cells convert zearalenone into its hydroxylated metabolites alpha-zearalenol and beta-zearalenol. Vet Res Commun. 2006;30(4):445-453.
- Al-Jaal BA, Jaganjac M, Barcaru A, et al. Aflatoxin, fumonisin, ochratoxin, zearalenone and deoxynivalenol biomarkers in human biological fluids: A systematic literature review, 2001-2018. Food Chem Toxicol. 2019;129:211-228.
- Agarwal A, Mulgund A, Hamada A, Chyatte MR. A unique view on male infertility around the globe. Reprod Biol Endocrinol. 2015;13:37.
- El Khoury D, Fayjaloun S, Nassar M, et al. Updates on the Effect of Mycotoxins on Male Reproductive Efficiency in Mammals. Toxins (Basel). 2019;11(9):515.
- Ibeh IN, Uriah N, Ogonor JI. Dietary exposure to aflatoxin in human male fertility in Benin City, Nigeria. Int J Fertil Menopausal Stud.1994;39(4):208-214.
- Uriah N, Ibeh IN, Oluwafemi FT. A study on the impact of aflatoxins on human reproduction. Afr J Reprod Health. 2001;5(1):106-110.
- Eze UA, Huntriss J, Routledge MN, Gong YY. Toxicological effects of regulated mycotoxins and persistent organochloride pesticides: In vitro cytotoxic assessment of single and defined mixtures on MA-10 murine Leydig cell line. Toxicol In Vitro. 2018;48:93-103.
- Wang J, Yang C, Yuan Z, et al. T-2 Toxin Exposure Induces Apoptosis in TM3 Cells by Inhibiting Mammalian Target of Rapamycin/Serine/Threonine Protein Kinase(mTORC2/AKT) to Promote Ca2+Production. Int J Mol Sci. 2018;19(11):3360.
- Yang JY, Zhang YF, Li YX, et al. l-arginine protects against oxidative damage induced by T-2 toxin in mouse Leydig cells. J Biochem Mol Toxicol. 2018;32(10):e22209.
- Yang JY, Zhang YF, Li YX, et al. Effects of t-2 toxin on the regulation of steroidogenesis in mouse leydig cells. Toxicol Ind Health. 2016;32(10):1801-1807.
- Jian YY, Yong FZ, Xiang PM, et al. T-2 toxin inhibits gene expression and activity of key steroidogenesis enzymes in mouse leydig cells. Toxicol In Vitro. 2015;29:1166-1171.
- Zhang YF, Su PK, Wang LJ, et al. T-2 toxin induces apoptosis via the Bax-dependent caspase-3 activation in mouse primary Leydig cells. Toxicol Mech Methods. 2018;28(1):23-28.
- Yuan Z, Matias FB, Yi JE, Wu J. T-2 toxin-induced cytotoxicity and damage on TM3 Leydig cells. Comparative biochemistry and physiology. Comp Biochem Physiol C Toxicol Pharmacol.2019;181-182:47-54.
- Austin KJ, Cockrum RR, Jons AM, et al. Renin mRNA is upregulated in testes and testicular cells in response to treatment with aflatoxin B1. Theriogenology. 2012;77(2):331-7.e77.
- Lin P, Chen F, Sun J, et al. Mycotoxin zearalenone induces apoptosis in mouse Leydig cells via an endoplasmic reticulum stress-dependent signalling pathway. Reprod Toxicol. 2015;52:71-77.
- Liu Q, Wang Y, Gu J, et al. Zearalenone inhibits testosterone biosynthesis in mouse Leydig cells via the crosstalk of estrogen receptor signaling and orphan nuclear receptor Nur77 expression. Toxicol In Vitro. 2014;28(4):647-656.
- Wang Y, Zheng W, Bian X, et al. Zearalenone induces apoptosis and cytoprotective autophagy in primary Leydig cells. Toxicol Lett. 2014;226(2):182-191.
- Li Y, Zhang B, Huang K, et al. Mitochondrial proteomic analysis reveals the molecular mechanisms underlying reproductive toxicity of zearalenone in MLTC-1 cells. Toxicology. 2014;324:55-67.
- Aydin Y, Orta Yilmaz B, Yildizbayrak N, et al. Evaluation of citrinin-induced toxic effects on mouse Sertoli cells. [published online ahead of print, 2019 May 29]. Drug Chem Toxicol. 2019;1-7. [Epub ahead of print. 2019 May 29]
- Ewuola EO. Organ traits and histopathology of rabbits fed varied levels of dietary fumonisin B(1). J Anim Physiol Anim Nutr (Berl). 2009;93(6):726-731.
- Park H, Park HS, Lim W, Song G. Ochratoxin A suppresses proliferation of Sertoli and Leydig cells in mice. Med Mycol. 2020;58(1):71-82.
- Karacaoğlu E, Selmanoğlu G. T-2 toxin induces cytotoxicity and disrupts tight junction barrier in SerW3 cells. Environ Toxicol Pharmacol. 2017;56:259-267.
- Koraïchi F, Inoubli L, Lakhdari N, et al. Neonatal exposure to zearalenone induces long term modulation of ABC transporter expression in testis. Toxicology. 2013;310:29-38.
- Zheng W, Pan S, Wang G, et al. Zearalenone impairs the male reproductive system functions via inducing structural and functional alterations of sertoli cells. Environ Toxicol Pharmacol. 2016;42:146-155.
- Xu ML, Hu J, Guo BP, et al. Exploration of intrinsic and extrinsic apoptotic pathways in zearalenone-treated rat sertoli cells. Environ Toxicol. 2016;31(12):1731-1739.
- Cai G, Si M, Li X, et al. Zearalenone induces apoptosis of rat Sertoli cells through Fas-Fas ligand and mitochondrial pathway. Environ Toxicol. 2019;34(4):424-433.
- Zhang TY, Wu RY, Zhao Y, et al. Ochratoxin A exposure decreased sperm motility via the AMPK and PTEN signaling pathways. Toxicol Appl Pharmacol. 2018;340:49-57.
- Kim IH, Son HY, Cho SW, et al. Zearalenone induces male germ cell apoptosis in rats. Toxicol Lett. 2003;138(3):185-192.
- Yang J, Zhang Y, Wang Y, et al. Toxic effects of zearalenone and zearalenol on the regulation of steroidogenesis and testosterone production inmouse Leydig cells. Toxicol In Vitro. 2007;21(4):558-565.
- Yang JY, Zhang YF, Liang AM, et al. Toxic effects of T-2 toxin on reproductive system in male mice. Toxicol Ind Health. 2010;26(1):25-31.
- Gharbi A, Trillon O, Betbeder AM, et al. Some effects of ochratoxin A, a mycotoxin contaminating feeds and food, on rat testis. Toxicology. 1993;83(1-3):9-18.
- Selmanoğlu G. Evaluation of the reproductive toxicity of patulin in growing male rats. Food Chem Toxicol. 2006;44(12):2019-2024.
- Gbore FA. Reproductive organ weights and semen quality of pubertal boars fed dietary fumonisin B1. Animal. 2009;3(8):1133-1137.
- Gbore FA, Egbunike GN. Testicular and epididymal sperm reserves and sperm production of pubertal boars fed dietary fumonisin B(1). Anim Reprod Sci. 2008;105(3-4):392-397.
- Ewuola EO, Egbunike GN. Effects of dietary fumonisin B1 on the onset of puberty, semen quality, fertility rates and testicular morphology in male rabbits. Reproduction. 2010;139(2):439-445.
- Sprando RL, Collins TF, Black TN, et al. Characterization of the effect of deoxynivalenol on selected male reproductive endpoints. Food Chem Toxicol. 2005;43(4):623-635.
- Supriya C, Girish BP, Reddy PS. Aflatoxin B1-Induced Reproductive Toxicity in Male Rats: Possible Mechanism of Action. Int J Toxicol. 2014;33(3):155-161.
- Hasanzadeh S, Rezazadeh L. Effects of aflatoxin B1 on the growth processes of spermatogenic cell series in adult male rats. Comp Clin Path. 2012;22(4):555-562.
- Long M, Yang S, Wang Y, et al. The Protective Effect of Selenium on Chronic Zearalenone-Induced Reproductive System Damage in Male Mice. Molecules. 2016;21(12):1687.
- Sprando RL, Pestka J, Collins TF, et al. The effect of vomitoxin (Deoxnivalenol) on testicular morphology, testicular spermatid counts and epididymal sperm counts in IL-6KO [B6129-IL6 [tmlKopf] (IL-6 gene deficient)] and WT [B6129F2 (wild type to B6129-IL6 with an intact IL-6 gene)] mice. Food Chem Toxicol. 1999;37(11):1073-1079.
- Yang X, Zhang X, Zhang J, et al. Spermatogenesis disorder caused by T-2 toxin is associated with germ cell apoptosis mediated by oxidative stress. Environ Pollut. 2019;251:372-379.
- Alm K, Dahlbom M, Säynäjärvi M, et al. Impaired semen quality of AI bulls fed with moldy hay: a case report. Theriogenology. 2002;58(8):1497-1502.
- Mirocha CJ, Schauerhamer B, Christensen CM, et al. Incidence of zearalenol (Fusarium mycotoxin) in animal feed. Appl Environ Microbiol. 1979;38(4):749-750.
- Pestka JJ, Clark ES, Schwartz-Zimmermann HE, et al. Sex Is a Determinant for Deoxynivalenol Metabolism and Elimination in the Mouse Toxins (Basel). 2017;9(8):240. [Published correction in Toxins (Basel). 2019;11(5).].
- Wan D, Huang L, Pan Y, et al. Metabolism, distribution, and excretion of deoxynivalenol with combined techniques of radiotracing, high-performance liquid chromatography ion trap time-of-flight mass spectrometry, and online radiometric detection. J Agric Food Chem. 2014;62(1):288-296.
- Clark ES, Flannery BM, Pestka JJ. Murine Anorectic Response to Deoxynivalenol (Vomitoxin) Is Sex-Dependent. Toxins (Basel). 2015;7(8):2845-2859.
- Thangavel C, Boopathi E, Shapiro BH. Inherent sex-dependent regulation of human hepatic CYP3A5. Br J Pharmacol. 2013;168(4):988-1000.
- Dhir RN, Dworakowski W, Thangavel C, et al. Sexually dimorphic regulation of hepatic isoforms of human cytochrome p450 by growth hormone. J Pharmacol Exp Ther. 2006;316(1):87-94.
- Thangavel C, Boopathi E, Shapiro BH. Intrinsic sexually dimorphic expression of the principal human CYP3A4 correlated with suboptimal activation of GH/glucocorticoid-dependent transcriptional pathways in men. Endocrinology. 2011;152(12):4813-4824.
- Lewis CW, Smith JE, Anderson JG, Freshney RI. Increased cytotoxicity of food-borne mycotoxins toward human cell lines in vitro via enhanced cytochrome p450 expression using the MTT bioassay. Mycopathologia. 1999;148(2):97-102.
- Dohnal V, Wu Q, Kuča K. Metabolism of aflatoxins: key enzymes and interindividual as well as interspecies differences. Arch Toxicol. 2014;88(9):1635-1644.
- Kim BR, Kim DH, Park R, et al. Effect of an extract of the root of Scutellaria baicalensis and its flavonoids on aflatoxin B1 oxidizing cytochrome P450 enzymes. Planta Med. 2001;67(5):396-399.
- Fink-Gremmels J, Jahn A, Blom MJ. Toxicity and metabolism of ochratoxin A. Nat Toxins. 1995;3(4):214-220.
- Gorski JG, Hall SD, Jones DR, et al. Regioselective biotransformation of midazolam by members of the human CYP3A subfamily. Biochem Pharmacol. 1994;47(9):1643-1653.
- Kolars JC, Lown KS, Schmeidlin-Ren P, et al. CYP3A gene expression in human gut epithelium. Pharmacogenetics. 1994;4(5):247-258.
- Thurman JD, Creasia DA, Trotter RW. Effects of testosterone on the prevention of T-2 toxin-induced adrenocortical necrosis in mice. Am J Vet Res. 1989;50(6):942-944.
- Raval PJ, Verma RJ. Steroid hormones retard aflatoxin-induced cytotoxicity. Indian J Exp Biol. 1993;31(9):780-781.
- Pestka JJ. Mechanisms of deoxynivalenol-induced gene expression and apoptosis. Food Addit Contam Part A Chem Anal Control Expo Risk Assess. 2008;25(9):1128-1140.
- Greene DM, Azcona-Olivera JI, Murtha JM, et al. Effects of dihydrotestosterone and estradiol on experimental IgA nephropathy induced by vomitoxin. Fundam Appl Toxicol. 1995;26(1):107-116.
- Iverson F, Armstrong C, Nera E, et al. Chronic feeding study of deoxynivalenol in B6C3F1 male and female mice. Teratog Carcinog Mutagen. 1995;15(6):283-306.
- Mor F, Kilic MA, Ozmen O, et al. The effects of orchidectomy on toxicological responses to dietary ochratoxin A in Wistar rats. Exp Toxicol Pathol. 2014;66(5-6):267-275.
- di Giuseppe R, Bertuzzi T, Rossi F, et al. Plasma ochratoxin A levels, food consumption, and risk biomarkers of a representative sample of men and women from the Molise region in Italy. Eur J Nutr. 2012;51(7):851-860.

Lauren Tessier, ND, is a licensed naturopathic physician specializing in mold-related illness. She is a nationally known speaker and is the vice president of the International Society for Environmentally Acquired Illness (ISEAI) – a non-profit dedicated to educating physicians about the diagnosis and treatment of environmentally acquired illness. Dr Tessier’s practice, “Life After Mold,” in Waterbury, VT, draws clients from all around the world who suffer from chronic complex illness as a result of environmental exposure and chronic infections. Dr Tessier’s e-booklet, Mold Prevention: 101, has been widely circulated and its suggestions implemented by many worldwide. Facebook tagging: @lifeaftermold