Etiological Factors Involved With Metabolic Syndrome
Mona Morstein, ND
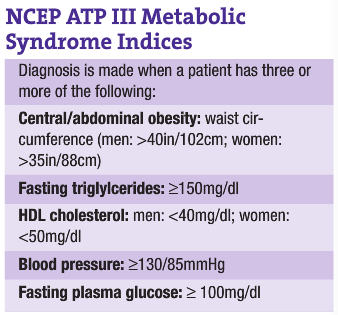
Although allopathic physicians recently have been debating whether metabolic syndrome is actually a syndrome, the rest of the world seems solidly ensconced in the belief that it is. The World Health Organization (WHO) was first to come out with guidelines for diagnosing metabolic syndrome in 1998, but the criteria mainly used now are those instituted by the Adult Treatment Panel (ATP) III by the National Cholesterol Education Program (NCEP; see accompanying sidebar). However, some additional guidelines are gaining ground as well, such as a triglyceride/HDL ratio of >3 and elevated fasting/postprandial insulin levels. Several recent studies have used postprandial insulin – a guideline many NDs have been using for years – as a method for analyzing insulin resistance.
Metabolic syndrome is immediately tied to insulin resistance; in fact, it is the insulin resistance and the resultant biochemical, hormonal and physiological changes induced in the body that cause the development of the metabolic syndrome indices.
Ten etiological factors exist for a person developing insulin resistance, putting them at considerable risk for metabolic syndrome: genetics; feast or famine/physiological development; high carbohydrate diet; diet drinks and food; high saturated fat diet; nutritional deficiencies; lack of exercise; obesity; hormonal imbalances; and environmental toxicities. I will briefly discuss each of these.
Genetics
Genetics is a type of evolutionary Sword of Damocles, and whether or not it falls, initiating disease in an individual, is unknown. What we mostly know from genetics is that if a person has an unhealthy lifestyle, then the illnesses they have a higher chance of developing are those that previous vertical relatives suffered from. Thus, if a person has obese relatives with Type II diabetes, and if he or she develops obesity, doesn’t exercise and so forth, there is evidence that that person has a higher risk for developing insulin resistance, metabolic syndrome and diabetes.
Feast-or-Famine Populations
Historically, food has been an uncertainty. Up until the 19th century, food has never been a guarantee in the world. Even now, only Westernized cultures have organized food growth and delivery to ensure a continued supply year-round. Drought, floods, diseased food, wars, over-hunting, hailstorms and other natural disasters, and so forth constantly wreaked havoc on a population’s capacity to ensure there was enough food and calories to maintain life and thrive. Even when the weather cooperated, it was easier to provide food during spring, summer and fall than during the long, cold months of winter. Thus, it was an evolutionary benefit to the human species for some people to be able to gain weight more easily when food was bountiful; they would be more likely to survive if and when the food source to the community was cut off, and during the normal limitations on food during the winter. As these cultures found themselves losing their native lifestyles and accompanying exercise, along with consuming a higher carbohydrate diet, they soared to the top of the diabetes epidemics. Many cultures with feast-or-famine lifestyles, such as Native Americans and the Pacific Islanders, are at the highest risk of developing obesity, metabolic syndrome and diabetes.
High-Carbohydrate Diet
Drs. Gross and Liu conducted a meta-analysis to discern which food in the last 30 years has been the leading factor in the Western development of obesity. Their conclusion: high fructose corn syrup. This sweetener came into American culture in the 1970s, and not long after began the rise in obesity among Americans, which now has reached incredible proportions: 60% of the population is documented as being overweight, and up to 20%-30% of that demographic is considered to be obese. The pediatric population, historically lean, has its own epidemic of obesity. When “high carbohydrate” is being used as a cause for metabolic syndrome, study authors are not referring to whole grains, fruits and vegetables; instead, refined sugars and flours are the causative agents. The intake of refined sugar has increased to about 150 pounds per year in the last century, up from five pounds around 1900. A study from WHO shows that when children were given different diets – all containing the same number of calories – the only incidence where children gained weight was with the diet highest in sugar.
Diet Drinks and Food
Recently published studies illustrate that people using “diet” foods (those with artificial sweeteners) actually have a higher risk of developing obesity. These match studies in the past showing that people consuming diet beverages actually ate more food than those drinking non-diet ones. While the exact physiological reason has not been wholly elucidated, the research seems to be clear, and patients need to be cautioned that imbibing a large amount of diet beverages puts them at risk of weight gain.
High Saturated Fat
In cultures such as the Japanese, where historically 70% of their diet has been carbohydrate based, they did not begin seeing problems with weight gain and diabetes until saturated fat became common in their diets through the addition of Western fast food. Saturated fats are clearly associated with high total and LDL cholesterol and triglylcerides. On the other hand, one wonders if the problems from saturated fat stem more from the lack of balancing essential fatty acids in the diet than the actual inclusion of saturated fats. Historically, meat was one of the main sources of essential fatty acids in the human diet, as grass-fed animals produce a great deal of essential fatty acids in their meat; in fact, almost half the fat in animals fed their natural diet can be essential fatty acids, as well as conjugated linoleic acid, a type of fat shown to lower the risk of weight gain and provide some anticarcinogenic protection. But with modern agri-industry processing of meat, especially the feedlot phenomenon and grain feeding of animals, modern meat contains an artificially elevated amount of saturated fat and an almost total lack of essential fatty acids. It seems that a combination of both increased saturated fat intake and lack of essential oils in the diet are contributing factors to weight gain and diabetes. Last, the focus on removing trans fats from the diet is helpful, as trans fats affect the body in ways similar to saturated fats. Of course, unfortunately, the FDA allows companies to prevaricate on their nutrition labels; they may write “contains 0% trans fat” if a serving contains <.5 grams. As people naturally eat more than the serving size, they can still get substantial levels of trans fats in the diet while thinking they are receiving none. For example, if a serving size contains 0.4g, and a person eats four times the serving size (which is feasible given the size of servings), a person might unknowingly eat 1.6g of trans fats. Thus, NDs must train patients to ignore the trans fats percentage on the upper part of the nutrition label and instead search for words in the ingredient section that correspond to trans fats in the food: vegetable fat, vegetable shortening and partially hydrogenated oils.
Nutritional Deficiencies
Numerous nutrients are needed in the body for proper glucose regulation to occur, insulin sensitivity to be maintained, metabolic burning to occur efficaciously, blood pressure to be maintained and lipid levels to be optimal. The Standard American Diet, high in sugar and refined flours, low in fiber, and low in fruits and vegetables, has been proven deficient in numerous vital nutrients: essential fatty acids, zinc, chromium, magnesium, vitamin D and others. Amounts of nutrients in food today has decreased due to agri-industry farming; organic farming consistently shows higher levels of nutrients in its foods. The FDA recommends fiber intake of 25-35g/day, and Americans typically eat 10-12g. The American dietary fiber deficiency is problematic regarding insulin resistance and metabolic syndrome, as fiber can help lower glucose levels and appetite, and increase satiety. The surprising epidemic of vitamin D deficiency is a concern, as vitamin D helps promote insulin sensitivity.
Lack of Exercise
Our technological Western civilization has innately less exercise defining its daily lifestyle: Cars, washing machines, vacuum cleaners and supermarkets have reduced the amount of exercise that historically was common. People do not have to walk as a form of transportation, do not have to grow or hunt their own food, do not have to use washboards to clean clothes, do not have to lug coal upstairs to heat their homes or large chunks of ice for their iceboxes. Schools have dropped exercise from their standard class schedules, and the allure of computers and televisions keep kids and adults inside instead of outside playing games and being active. Exercise promotes weight loss and lowers blood pressure; increases HDL cholesterol; lowers glucose blood levels; and increases insulin sensitivity. All patients must be guided to include both aerobic and anaerobic exercise in their lives.
Obesity
A problematic catch-22 for patients is that insulin resistance causes abdominal weight gain, and abdominal weight gain causes and worsens insulin resistance. Both are key factors in the further development of metabolic syndrome. Insulin is known as the “fat-building hormone,” and higher levels of it circulating in the body direct the cells to make and store fat, reducing the metabolic burning of the cells. It is designed to be an energy storage hormone. The abdominally obese patient dumps a great deal of fatty acids into the portal venous system in the middle of the night, which flows to the liver. The liver has no sensors for glucose, only for insulin levels. The high amount of fatty acids hitting the liver causes it to become insulin resistant; thus, with the liver unable to record insulin levels, it mistakenly believes insulin levels are low. Low insulin trips the liver into producing glucose through gluconeogenesis and glycogenolysis; this is one reason morning glucose levels are elevated in the insulin-resistant person, and higher levels of insulin invariably will be produced to deal with the liver’s glucose output. Other factors guiding elevated morning glucose levels are the secretion of cortisol, adrenaline and growth hormone during the night. Since fat induces insulin resistance at the cell wall, and insulin resistance causes patients to gain and maintain their fat, breaking the cycle in all possible manners is essential. Patients need to engage in a proper diet, supplement and exercise regimen to decrease the insulin resistance and enable weight to be lost.
 Hormone Imbalances
Hormone Imbalances
The main hormone imbalances associated with possibly causing or enhancing insulin resistance and/or metabolic syndrome include: high or low cortisol levels, low thyroid hormone, low growth hormone, low or high testosterone, elevated estrogens and low DHEA. Although NDs tend to focus only on elevated cortisol as an inducer of glucose expression and a resultant insulin secretion, we need to be cognizant that low cortisol levels will interfere with thyroid activation of metabolic burning in the cells, and so we should not assume a cortisol imbalance, but instead do testing to verify if one exists. High insulin levels can throw off sex hormones, and those hormones also can induce insulin resistance. Ordering a hormone panel as indicated or appropriate with patients may help uncover imbalances significant enough to warrant treatment. A physician should also realize that by reversing the insulin resistance, many hormones have the potential for becoming more balanced innately, without needing to be treated individually.
Environmental Toxicities
The WHO has written comprehensive articles regarding the association of lead and arsenic toxicities with an increased occurrence of Type II diabetes. In addition, associative studies show that Type II patients at times have increased levels of chemical toxins, such as PCBs, but whether the diabetes prevented the excretion of the PCBs or the PCBs caused the diabetes is not clear. Whether these chemicals and heavy metals are causing insulin resistance or are affecting the cells in some other manner is unknown at this time, but the results should be followed up with more investigation.
Given the numerous etiological factors acting as obstacles to cure and clearly involved with the development and promotion of metabolic syndrome, it is logical and pragmatic for physicians to perform a comprehensive intake and appropriate testing when working with these patients. By uncovering all of the imbalances in patients, the chances of success in reversing their syndrome and preventing them from progressing to diabetes is markedly increased.
 Mona Morstein, ND graduated from NCNM in 1988, and completed a one-year family residency there. Moving to Great Falls, Mont., Morstein practiced medicine in her own clinic for 13 years, during which time she had a cable access TV show and was a regular writer in the Great Falls Tribune on natural medicine. She joined SCNM as an associate professor in 2002 and now is chair of nutrition and clinical supervisor, as well. Morstein particularly enjoys working with pre-diabetic and diabetic patients, GI conditions and women’s health. She is an avid hiker, a serious bibliophile, has written a book on Sherlock Holmes, and is a huge fan of the old TV show, “The Avengers.”
Mona Morstein, ND graduated from NCNM in 1988, and completed a one-year family residency there. Moving to Great Falls, Mont., Morstein practiced medicine in her own clinic for 13 years, during which time she had a cable access TV show and was a regular writer in the Great Falls Tribune on natural medicine. She joined SCNM as an associate professor in 2002 and now is chair of nutrition and clinical supervisor, as well. Morstein particularly enjoys working with pre-diabetic and diabetic patients, GI conditions and women’s health. She is an avid hiker, a serious bibliophile, has written a book on Sherlock Holmes, and is a huge fan of the old TV show, “The Avengers.”
References
Gross LS et al: Increased consumption of refined carbohydrates and the epidemic of type 2 diabetes in the United States: an ecological assessment, Am J Clin Nutr 79:774-9, 2004.
WHO: Executive Summary of WHO on Diet, Nutrition and the Prevention of Disease, Bulletin of the WHO 81(8), March 2003.









