SIBO: The Finer Points of Diagnosis, Test Interpretation, and Treatment
ALLISON SIEBECKER, ND, MSOM, LAC
STEVEN SANDBURG-LEWIS, ND, DHANP
One of our major goals is educating physicians about effective treatments for irritable bowel syndrome (IBS). In our last article on small intestine bacterial overgrowth (SIBO), we explained the basics of this major cause of IBS. As a follow-up, we will now discuss the fine points of diagnosis and test interpretation (with case examples) as well as diet, probiotics, repair, and prevention.
Diagnosis of SIBO
There are 2 tests that can diagnose SIBO: endoscopy with culture, and hydrogen/methane breath testing. Neither stool testing nor urine organic acid testing can diagnose SIBO. The most common method of assessing SIBO is hydrogen/methane breath testing because it offers the most accurate and detailed information while also being non-invasive and inexpensive. In comparison, endoscopy, while offering a direct measurement, has several limitations. It is invasive, expensive, and can only sample the proximal small intestine, since endoscopy doesn’t typically extend beyond the duodenum.1 This is a significant limitation since distal SIBO is thought to be most common.2 Additionally, culturing cannot accurately reflect the anaerobic bacteria present in SIBO since most anaerobic bacteria cannot be cultured.3 Similarly, organic acid testing, which can indirectly indicate bacterial overgrowth by the presence of urinary hippurate, p-hydroxybenzoate, and other bacterial metabolites, cannot distinguish the location of overgrowth between the distal small intestine and the proximal large intestine, nor offer the details provided in a breath test.4 Stool tests can only suggest large intestine bacterial overgrowth, although they can show the fat malabsorption that often results from SIBO.
Bacterial overgrowth produces excess quantities of hydrogen and/or methane gas.5, 6 These gases are not produced by humans but are the metabolic byproducts of fermentation of carbohydrates by intestinal bacteria.7 The breath test measures these gases and is therefore an indirect test; however, it specifies which gases are present, as well as the location and severity of the SIBO. This information is often essential for treatment and assessing prognosis. Moreover, the majority of research studies on SIBO employ the breath test.
After collection of a fasting baseline specimen, a solution of lactulose, a non-absorbable synthetic sugar, is ingested as the substrate for bacterial fermentation. Only bacteria, not humans, produce the enzymes to digest lactulose. It takes lactulose approximately 2 hours to traverse the small bowel. Serial breath specimens are taken every 15-20 minutes during this time to reflect the quantity of small intestine bacteria, and for a third hour, which reflects the large intestine. Though lactulose transit time through the small intestine is debated in the literature, a minimum of 90 minutes is generally agreed upon to properly reflect SIBO.2 Glucose may also be used as a test substrate, but because of its rapid absorption in the proximal small intestine, it fails to identify distal SIBO.2 If glucose testing is negative, a lactulose test is still required to test for distal SIBO.
The test requires a 24-hour prep diet and an overnight fast. Preparation for the test varies from lab to lab, but a typical prep diet is limited to white rice, fish/poultry/meat, eggs, hard cheeses, clear beef or chicken broth (not bone broth or bouillon), oil, salt, and pepper. The purpose of the prep diet is to obtain a clear reaction to the test solution by reducing the presence of fermentable foods. In some cases, 2 days of prep diet may be needed to sufficiently reduce baseline gases to negative. Antibiotics should not be used for at least 2 weeks prior to an initial test, although some sources recommend 4 weeks.7 If a patient is on continuous antibiotics and SIBO is suspected, initial breath testing may be performed without halting antibiotics.
Testing may be performed at a facility with a breath testing machine or at home with a kit which is mailed in for analysis. (Refer to www.siboinfo.com/testing.) Not all labs test for methane, as instrumentation varies. Methane testing is important because treatment can differ for methane versus hydrogen.
Interpretation of the test may vary widely among practitioners.2 There is no agreed-upon criteria, a situation which we hope to see remedied. It’s very possible that a patient may be considered positive by one doctor/lab and negative by another. The criteria provided by the machine manufacturer for a positive test are as follows:8
• A rise over lowest preceding value in hydrogen production of 20 parts per million (ppm) or greater within 120 minutes after ingesting lactulose
• A rise over lowest preceding value in methane production of 12 ppm or greater within 120 minutes after ingesting lactulose
• A rise over lowest preceding value in the combined sum of hydrogen and methane production of 15 ppm or greater within 120 minutes after ingesting lactulose
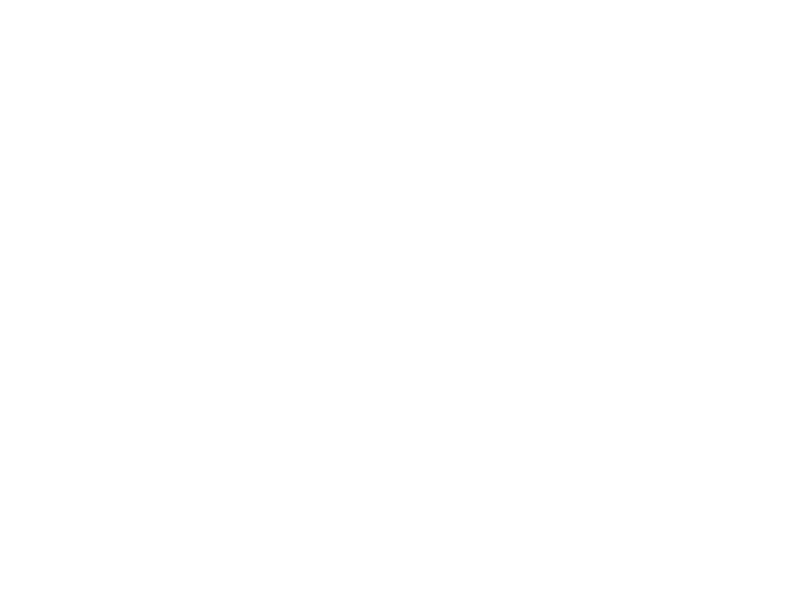
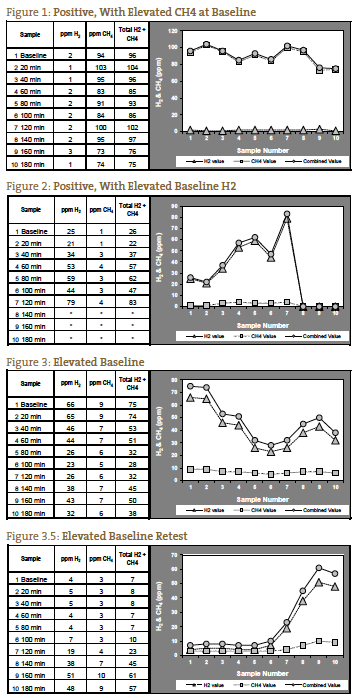
We have found that an absolute level of gases at or above the positive ppm levels provided by QuinTron, without a rise over baseline or lowest preceding value, correlates well with clinical SIBO. This is especially true for methane gas, which can have a pattern of an elevated baseline (> 12 ppm) that remains elevated for the duration of the test (Figure 1). In cases such as these, methane may only rise 5 ppm, but the ppm level is consistently above the positive cutoff. Interpretation of elevated hydrogen or methane on the baseline specimen (pre-lactulose ingestion) is controversial, but we prefer to consider a high baseline value to be a positive test9, 10 (Figure 2) unless gas levels fall after baseline and continue to diminish or remain low during the first 2 hours, indicating improper prep diet (Figures 3 and 3.5).
The classic positive for SIBO has been considered to be a double peak, with the first peak representing the SIBO and the second peak representing the normal abundance of large intestine bacteria (Figure 4). This is an infrequent presentation in our experience. More often we see 1 peak which rises even higher in the third hour, representing distal SIBO followed by the normal large intestine bacteria (Figure 5).
If the measured gases do not rise until after 120 minutes, it is possible that this is due to a prolonged transit time, which we have seen in patients with severe constipation. In such a patient with the expected symptom picture for constipation-type SIBO, a significant rise at 140 minutes may be interpreted as a positive test (Figure 6). Figure 7 represents a negative test; note the scale on the left of the graph is reduced to reflect the lower gas levels. Figures 1 through 7 are case examples provided by NCNM’s lab.
Breath testing may be used in pediatric cases, so long as the child can properly follow instructions to blow into the collection device. For those under 3 years old, testing is best done in office/lab, due to differences in collection methods versus at-home kits. Pediatric lactulose dosing is 1g/kg body weight, with a maximum of 10 g (22 lbs and above receive the maximum adult dose of 10 g).11 Lactulose kits can only be ordered by prescribing physicians, since lactulose is a prescription item.
Dietary Treatment
Diets used to treat SIBO reduce bacterial load and fermentation of carbohydrates, as well as aid tissue healing. They do this by decreasing polysaccharides, oligosaccharides and disaccharides via the elimination of all grains, starchy vegetables, lactose, and sweeteners other than honey. Legumes are eliminated initially. We have found that using the Specific Carbohydrate Diet™ (SCD) or its variant, the Gut and Psychology Syndrome™ diet (GAPS) as the core diet, with the incorporation of the fruit and vegetable recommendations from the Low FODMAP™ diet (Table 1) is an effective approach. (See Table 2 for SIBO Diet Resources.) The Low FODMAP diet is an IBS treatment diet that is a result of investigating the levels of fermentable carbohydrates in foods; it has a success rate of 76% for IBS.12 The FODMAP diet is not specifically designed for SIBO and therefore does not eliminate polysaccharide and disaccharide sources such as grains, starch, starchy vegetables, and sucrose. Eliminating these poly- and disaccharides is essential in SIBO. In SIBO, well-absorbed carbohydrates, foods that usually go to feed the host, feed instead the increased small intestine bacteria, creating symptoms and fueling more bacterial growth1 (Figure 8).
Any diet will need to be individualized by trial and error over time. Providing a food chart or particular diet prescription merely offers a place to start.
Low-carbohydrate diets are weight loss diets. Particular attention must be paid to those who are borderline or underweight. If a SIBO diet leads to excessive weight loss, this dietary strategy will need to be altered to allow for more carbohydrates. In these circumstances one or more of the other 3 treatment options described in our previous article should be considered, along with white rice, glucose and other carbohydrate sources.
Probiotics
Probiotics are a controversial intervention in SIBO because lactobacilli have been cultured in SIBO13 and there is concern about adding to the bacterial overload. This is particularly the case when there is decreased motility due to a dysfunctional migrating motor complex (MMC). Despite this concern, the few probiotic studies that have focused directly on SIBO have shown good results, with an eradication rate of 47% from Bacillus clausii as the only treatment,14 64% success rate from Lactobacillus casei Shirota as the only treatment,15 and a clinical improvement of 82% from Lactobacillus casei and L. plantarum, Streptococcus faecalis, and Bifidobacter brevis as the only treatment.16 Probiotic yogurt containing Lactobacillus johnsonii normalized cytokine responses, reducing the low-grade, chronic inflammation found in SIBO, after 4 weeks of supplementation.17 We have seen good results in our SIBO patients using various multi-strain and single probiotics, as well as homemade lactose-free yogurt and cultured vegetables.
A key point for the use of probiotic supplements in SIBO is to avoid prebiotics as main ingredients. Prebiotics are fermentable food for bacteria which can exacerbate symptoms during active SIBO and encourage bacterial growth post-SIBO. Common prebiotics found in probiotic supplements include: FOS (fructo-oligosaccharide), MOS (mannan-oligosaccharide), GOS (galacto-oligosaccharide), inulin, and arabinogalactan. Prebiotics may be individually tolerated in the small amounts used as base ingredients.
Intestinal Permeability
Studies examining the rate of mucosal healing post-SIBO found that intestinal permeability normalized in 75%-100% of SIBO patients within four weeks following successful antibiotic treatment.18,19 For those whose permeability does not normalize, supplements may aid in the process of healing.
Mucilaginous herbs are traditionally employed for mucosal healing, including Glycyrrhiza glabra (licorice), Ulmus fulva (slippery elm), Aloe vera, and Althea officinalis (marshmallow); however, their use post-SIBO is controversial due to their mucopolysaccharide content which could encourage bacterial regrowth. Specific nutrients we have used include colostrum (2-6 g QD), L-glutamine (375-1500+ mg QD), zinc carnosine (75-150 mg QD), vitamins A and D, often given as cod liver oil (1 tbsp QD), curcumin (400 mg to 3 g QD), resveratrol (250 mg to 2 g QD), glutathione, as oral liposomal (50-425 mg QD) or the glutathione precursor N-acetylcysteine (200-600 mg QD. Supplements are given for 1 to 3 months, or may be continued long term. Higher dosages of curcumin and resveratrol are given for 2 weeks for the purpose of down-regulating NF-Κβ, a mediator of increased intestinal permeability, followed by more moderate maintenance levels.20, 21,22
Prevention
Supplements
Betaine hydrochloric acid or herbal bitter supplements, which encourage hydrochloric acid (HCl) secretion23 may be used to decrease the load of ingested bacteria. When considering HCl supplementation, Heidelberg pH testing is the gold standard.
Meal Spacing
In addition to prokinetic agents (discussed in our January 2013 article), spacing meals 4 to 5 hours apart, ingesting nothing other than water, allows the migrating motor complex (MMC) to sweep the small intestine clean of bacteria at night and between meals.24 We have found this to be very helpful clinically. If a low-carb SIBO diet does not correct hypoglycemia, this strategy will need to be altered to allow for more frequent meals.
Current perspectives on test interpretation and treatment strategies will be discussed at the 2014 SIBO Symposium, January 18-19th in Portland OR, and will also be available via live and recorded webinar (www.sibosymposium.com).
 Allison Siebecker, ND, MSOM, LAc is a graduate of National College of Natural Medicine (Portland, Oregon), where she specializes in treating small intestinal bacterial overgrowth (SIBO) and is adjunct professor of advanced gastroenterology. She is currently writing a book on SIBO. Visit her educational SIBO website at www.siboinfo.com.
Allison Siebecker, ND, MSOM, LAc is a graduate of National College of Natural Medicine (Portland, Oregon), where she specializes in treating small intestinal bacterial overgrowth (SIBO) and is adjunct professor of advanced gastroenterology. She is currently writing a book on SIBO. Visit her educational SIBO website at www.siboinfo.com.
 Steven Sandberg-Lewis, ND, DHANP, has been a practicing naturopathic physician since his graduation from National University of Natural Medicine (NUNM) in 1978. He has been a professor at NUNM since 1985, teaching a variety of courses but primarily focusing on gastroenterology and GI physical medicine. His clinic rotations are particularly popular among NUNM doctoral students. In addition to supervising clinical rotations he also maintains a part-time practice at 8Hearts Health and Wellness in Portland, Oregon.
Steven Sandberg-Lewis, ND, DHANP, has been a practicing naturopathic physician since his graduation from National University of Natural Medicine (NUNM) in 1978. He has been a professor at NUNM since 1985, teaching a variety of courses but primarily focusing on gastroenterology and GI physical medicine. His clinic rotations are particularly popular among NUNM doctoral students. In addition to supervising clinical rotations he also maintains a part-time practice at 8Hearts Health and Wellness in Portland, Oregon.
He is a popular international lecturer at functional medicine seminars, presents webinars, writes articles for NDNR and the Townsend Letter and is frequently interviewed on issues of digestive health and disease. He is the author of the medical textbook Functional Gastroenterology: Assessing and Addressing the Causes of Functional Digestive Disorders, Second Edition, 2017, which is available at amazon.com. In 2010 he co-founded the SIBO Center at NUNM which is one of only four centers in the USA for Small Intestine Bacterial Overgrowth diagnosis, treatment, education and research. In 2014 he was named one of the “Top Docs” in Portland monthly magazine’s yearly healthcare issue and in 2015 was inducted into the OANP/NUNM Hall of Fame.
Within gastroenterology, he has special interest and expertise in inflammatory bowel disease (including microscopic colitis), irritable bowel syndrome (including post-infectious IBS), Small Intestine Bacterial Overgrowth (SIBO), hiatal hernia, gastroesophageal and bile reflux (GERD), biliary dyskinesia, and chronic states of nausea and vomiting.
Many of the patients referred to Dr. Sandberg-Lewis have digestive conditions that have defied diagnosis and effective resolution. Often these patients desire naturopathic treatment options in lieu of the courses of treatments they have previously undergone. He understands diseases of the gastrointestinal tract, but also can assess function and often find successful treatments to regain a balance in the digestive system.
Dr. Sandberg-Lewis lives in Portland with his wife, Kayle. His interests include mandolin, guitar and voice; cross country skiing; writing and lecturing.
References
1. Lin HC. Small intestinal bacterial overgrowth: a framework for understanding irritable bowel syndrome. JAMA. 2004;292(7):852-858.
2. Shah ED, Basseri RJ, Chong K, Pimentel M. Abnormal breath testing in IBS: a meta-analysis. Dig Dis Sci. 2010;55(9):2441-2449.
3. Khoshini R, Dai SC, Lezcano S, Pimentel M. A systematic review of diagnostic tests for small intestinal bacterial overgrowth. Dig Dis Sci. 2008;53(6):1443-1454.
4. Lord RS, Bralley JA. Clinical applications of urinary organic acids. Part 2. Dysbiosis markers. Altern Med Rev. 2008;13(4):292-306.
5. Riordan SM, Kim R. Bacterial overgrowth as a cause of irritable bowel syndrome. Curr Opin Gastroenterol. 2006;22(6):669-673.
6. Koide A, Yamaguchi T, Odaka T, et al. Quantitative analysis of bowel gas using plain abdominal radiograph in patients with irritable bowel syndrome. Am J Gastroenterol. 2000;95(7):1735-1741.
7. Eisenmann A, Amann A, Said M, et al. Implementation and interpretation of hydrogen breath tests. J Breath Res. 2008;2(4):046002.
8. Protocols and Interpretation Help, Hydrogen/Methane Breath Tests. Milwaukee, WI: QuinTron Instrument Company, Inc; 2013.
9. Quigley EM, Quera R. Small intestinal bacterial overgrowth: roles of antibiotics, prebiotics, and probiotics. Gastroenterology. 2006;130(2 Suppl 1):S78–S90.
10. Pimentel M, Lin HC, Enayati P, et al. Methane, a gas produced by enteric bacteria, slows intestinal transit and augments small intestinal contractile activity. Am J Physiol Gastrointest Liver Physiol. 2006;290(6):G1089-G1095.
11. QuinTron catalog and Information. Milwaukee, WI: QuinTron Instrument Company Inc; 2012:22.
12. Staudacher HM, Whelan K, Irving PM, Lomer MC. Comparison of symptom response following advice for a diet low in fermentable carbohydrates (FODMAPs) versus standard dietary advice in patients with irritable bowel syndrome. J Hum Nutr Diet. 2011;24(5):487–495.
13. Bouhnik Y, Alain S, Attar A, et al. Bacterial populations contaminating the upper gut in patients with small intestinal bacterial overgrowth syndrome. Am J Gastroenterol. 1999;94(5):1327–1331.
14. Gabrielli M, Lauritano EC, Scarpellini E, et al. Bacillus clausii as a treatment of small intestinal bacterial overgrowth. Am J Gastroenterol. 2009;104(5):1327-1328.
15. Barrett JS, Canale KE, Gearry RB, et al. Probiotic effects on intestinal fermentation patterns in patients with irritable bowel syndrome. World J Gastroenterol. 2008;14(32):5020-5024.
16. Soifer LO, Peralta D, Dima G, Besasso H. Comparative clinical efficacy of a probiotic vs. an antibiotic in the treatment of patients with intestinal bacterial overgrowth and chronic abdominal functional distension: a pilot study. Acta Gastroenterol Latinoam. 2010;40(4):323-327.
17. Schiffrin EJ, Parlesak A, Bode C, et al. Probiotic yogurt in the elderly with intestinal bacterial overgrowth: endotoxaemia and innate immune functions. Br J Nutr. 2009;101(7):961-966.
18. Lauritano EC, Valenza V, Sparano L, et al. Small intestinal bacterial overgrowth and intestinal permeability. Scand J Gastroenterol. 2010;45(9):1131-1132.
19. Riordan SM, McIver CJ, Thomas DH, et al. Luminal bacteria and small-intestinal permeability. Scand J Gastroenterol. 1997;32(6):556-563.
20. Ruland J. Return to homeostasis: downregulation of NF-κB responses. Nat Immunol. 2011;12(8):709-714.
21. Al-Sadi RM, Ma TY. IL-1beta causes an increase in intestinal epithelial tight junction permeability. J Immunol. 2007;178(7):4641-4649.
22. Csaki C, Mobasheri A, Shakibaei M. Synergistic chondroprotective effects of curcumin and resveratrol in human articular chondrocytes: inhibition of IL-1beta-induced NF-kappaB-mediated inflammation and apoptosis. Arthritis Res Ther. 2009;11(6):R165.
23. Bowman G. The Gut, the Brain and the Functional GI Disorders. Functional Gastroenterology Seminar: Level 1. NCNM; Winter, 2010:19. [Class sponsored by Seven Waves Wellness.]
24. Pimentel M. A New IBS Solution. Sherman Oaks, CA: Health Point Press; 2006.