Chronic Major Depression: Rapid Improvement Using Naturopathic Therapies
Student Scholarship – Second Place Case Study
Courtney K. Pickworth, BA
Lai Chim Chan, ND
Major depressive disorder (MDD) is a significant public health concern associated with increased functional disability and mortality.1 Patients with depression have at least a 27-times-greater likelihood of death by suicide compared to the general population.2 The current estimate of lifetime prevalence of unipolar depression (MDD and persistent depressive disorder [PDD]) is 18%, and the 12-month prevalence is 6%.1 Additionally, MDD is often chronic and patients are highly likely to experience relapse.1
There are several working theories regarding the underlying causes of depression. MDD likely represents a set of heterogeneous disorders that result in depressed mood and associated symptoms.1 One theory is that certain individuals are unable to synthesize or utilize mood-related neurotransmitters appropriately; this is perhaps because of genetically-linked or epigenetic enzyme deficiencies, environmental exposures to neurologically active toxicants, or physiological or psychological trauma resulting in changes in neural networking.3,4 Another theory posits an association between depressed mood and the hypothalamic-pituitary-adrenal (HPA) axis; studies have found an association between overproduction of corticotropin-releasing hormone (CRH) and depression, possibly leading to suppression of neurogenesis.5,6
Another etiological theory that has emerged within recent decades is that depression is related to inflammation. Evidence from a meta-analysis of studies from 1967 to 2008 suggests that MDD is associated with higher mean levels of systemic inflammatory markers, such as high-sensitivity C-reactive protein (hs-CRP) and the proinflammatory cytokines interleukin (IL)-6 and IL-1.8 This theory is also supported by several review articles that suggest many possible underlying mechanisms of action for this relationship, including disruption of neurotransmitter synthesis pathways as well as systemic inflammation including oxidative stress.8-12 Inflammatory states have been associated with treatment-resistant depression, suggesting that addressing underlying inflammation may be the key to treatment success. This concept is supported by results of randomized trials that demonstrated the ability of pharmaceutical anti-inflammatory agents, such as infliximab, to improve symptoms and disease course in patients with depression.13,14
The first-line treatment for severe depression is the selective serotonin reuptake inhibitor (SSRI) class of medications. The proposed mechanism of action for this drug class is an induced increase in serotonergic activity.15 Common side effects of SSRIs include sexual dysfunction (17%), drowsiness (17%), weight gain (12%), insomnia (11%), anxiety (11%), dizziness (11%), and headaches (10%).16 Importantly, SSRIs are effective in only 50% of primary care patients, and the Number Needed to Treat (NNT) for depression symptom improvement is 6.16 Given that this standard-of-care treatment can be limited in its efficacy and tolerance, patients will often present to naturopathic physicians requesting alternatives to SSRIs. In this article, we present a case report of chronic, severe MDD in which naturopathic therapies were effectively used to improve mood.
Presenting Concerns & Clinical Findings
A 29-year-old female presented to the NUNM clinic in July 2018, seeking alternative approaches for depression and anxiety. The patient reported she had been experiencing depression for the duration of her memory and that her depressed mood might be related to childhood sexual abuse from a relative, though this incident was not discussed in detail during the visit. Her mood dysregulation had historically been managed with pharmaceuticals and counseling; however, she reported having had an adverse reaction (heart palpitations) to SSRIs (name of med not recalled) prescribed to her in early 2018. She had never been hospitalized for MDD or for any other mental illness.
At this first visit, she reported severe depression (9/10 on a self-reported 1-10 scale of depression, with 10 being the highest). She was experiencing sleep changes (reduced sleep duration), feelings of guilt and worthlessness, low energy, cognitive difficulties, psychomotor retardation, and suicidal ideation. She denied a plan or intent associated with this suicidal ideation. Her self-reported cognitive difficulties manifested as “brain fog” and memory loss (both short- and long-term), which she attributed to her lifelong depressed mood. The patient was not currently experiencing changes in appetite associated with her depression. She had also been experiencing anxiety during the past year, which was new for her. There was no identifiable incident or factor that could have contributed to her worsened mood regulation within the past year.
She reported dissatisfaction with her social life, occupation, and motivation to complete daily tasks. She also suffered from sleep dysregulation due to being a night-shift worker. She ate a standard American diet and lived a sedentary lifestyle, though she had enjoyed engaging in physical activity in the past. She denied drug use, but occasionally drank alcohol. She reported a family history of depression, including her sister and several members on her mother’s side of the family. Besides 1 month of counseling and the aforementioned previous trial of SSRIs, she had not been treated for her depressed mood or anxiety.
Physical examination of heart, lung, abdomen, HEENT (head, eyes, ears, nose, throat), and peripheral pulses was unremarkable. She did, however, present with the blunt affect typical of severe depression.
Diagnostic Assessment
According to the Diagnostic & Statistical Manual of Mental Disorders V (DSM V), major depressive disorder (MDD) is diagnosable based upon clinical picture alone if the episode is not attributable to the direct physiological effects of a substance or other medical condition.17 The patient reported that recent blood tests ordered by her primary care physician were normal. Current blood work considerations included a complete blood count and thyroid-stimulating hormone; however, we suspected that the likelihood of abnormalities in these areas being the cause of her symptoms was low.18 Unfortunately, we were unable to obtain the lab results to confirm. She also denied current use of any medications or substances that might explain her symptoms.
At the initial office visit, she has a PHQ-9 score of 24 (range: 0 to 27) and a GAD-7 score of 16 (range: 5 to >15), indicating both severe depression and anxiety, respectively. We inferred from her previous treatment with SSRIs and her personal report of a history of depression that MDD was the working diagnosis. Indeed, based upon the presence of 7 out of 8 major symptom criteria for MDD, and the chronicity of the complaint, the patient was diagnosed with severe, recurrent MDD without psychotic features.
Therapeutic Interventions
Given the severity of the patient’s depression, it was important to review with the patient the standard-of-care option of SSRIs. However, given her previous adverse reaction and her preference for natural treatment, we recommended a well-known mood regulation supplement, 2 grams of fish oil per day, an exercise regimen, and sleep hygiene practices.
The recommended supplement is a combination of nutrients and botanicals designed to improve mood by providing neurotransmitter and adrenal support. Ingredients in this supplement include vitamins C, B5, B6, B9, B12, and iodine; amino acids and neurotransmitters L-tyrosine, 5-hydroxytryptophan, and gamma-aminobutyric acid (GABA); and the herbs Eleutherococcus senticosus and Rhodiola rosea. Several ingredients in this formula are evidence-based. Vitamin C supports adrenal gland function and reduces oxidative stress known to be present in depression.12 Additionally, B vitamins are essential for energy and executive function important in depression, including neurotransmitter synthesis (GABA, serotonin, and norepinephrine). A recent review summarized considerable evidence that supplementation with B vitamins improves depressive symptoms in both animal and human studies.19 Inclusion of the amino acids and neurotransmitters is based on evidence suggesting that tryptophan and phenylalanine (a precursor to tyrosine) are consumed by the body in greater quantities during inflammatory states. As such, it has been posited that depletion of these amino acids contributes to the phenotype of inflammation-based depression.20 A recent trial of otherwise-healthy young adults found that eating a diet high in tryptophan improved mood by reducing depressive symptoms and anxiety1; supplementation with tryptophan would logically have the same effect, though there are no current randomized controlled trials confirming this assumption. Furthermore, a review published in 1984 discussed mechanistic models supporting the use of tyrosine for depression; however, there have been no further clinical trials or reviews on this topic.22 Finally, the herbs included in this formula are known to support concentration, mood, and resilience to stress, according to both animal studies and clinical trials.23,24 The prescribed dose of this product was 2 capsules twice per day, as recommended by the manufacturer.
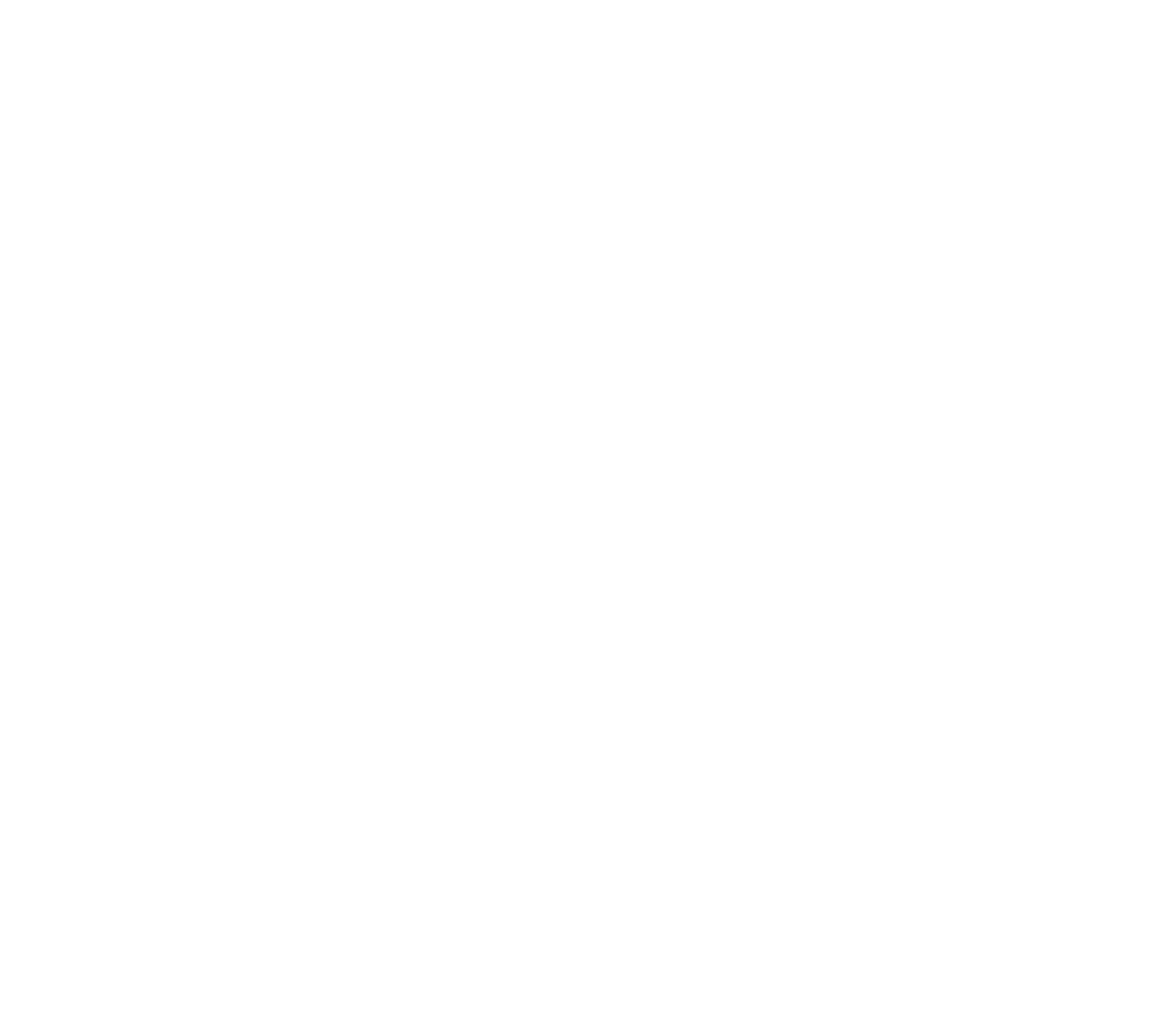
Fish oil (with a high EPA/DHA ratio) at 2 grams per day was recommended for its additional anti-inflammatory action. Multiple recent systematic reviews and meta-analyses compiled clinical evidence and made strong positive recommendations for supplementation with EPA-rich omega-3-fatty acids for depressive symptoms.25 We also recommended that the patient engage in moderate-to-high-intensity exercise (aerobic or anaerobic) for 3-5 days per week, which is proven to improve depression symptoms.26,27 Finally, we made several standard sleep hygiene recommendations (Figure 1) based upon the patient’s reported exhaustion and night-shift work, which in and of itself is associated with increased risk of depression.28 A recent randomized clinical trial of adolescents demonstrated improvement of depression symptoms with sleep hygiene advice similar to those given to our patient29; however, there are no clinical trials of adults with MDD that specifically investigate the relationship between sleep hygiene advice and depressive symptoms.
Figure 1. Sleep Hygiene Recommendations
Two-Month Follow-up
The patient returned to clinic for a follow-up appointment 8 weeks later (September 2018). She reported significant symptom relief, stating, “I’m happy.” She reported being compliant with the recommendations for the entire duration, which she believed contributed to her success. She did not have difficulty with following our recommendations except for exercising, which she had just restarted within the previous 2 weeks.
The patient presented noticeably happier and clearer in her affect; she made more eye contact, showed no signs of psychomotor retardation, and smiled during the visit. We repeated the PHQ-9 and GAD-7 at this visit, which delivered scores of 2 and 3, respectively. This fact caused the patient – who had felt depressed for much of her life and had completed these forms many times over the years – to exclaim, “This is the lowest score I’ve ever had!” She was thrilled with her progress and planned to follow up in 6 weeks to check in.
Current Day
Unfortunately, the patient has not returned to the NUNM Clinic since her second follow-up. Hence, we are unable to report whether she has been able to sustain a full remission, which would require symptom improvement for 4-6 months.30
The student author of this article was able to reach the patient by phone in November 2018. She reported recent stressful life events, including going through a divorce that has caused her mental health to be “up and down” at the time of the call. The patient denied suicidal ideation and reported increased resilience compared to her previous depressive episodes. However, the student was unable to determine whether the patient was still complying with our previous treatment recommendations.
Discussion
Though the patient was lost to follow-up, this case is an excellent example of successful treatment of patients with severe MDD who do not tolerate SSRIs or who decline SSRIs for any other reason. The combination of targeted supplementation with lifestyle recommendations supported her health through multiple mechanisms.
However, this case is not without limitations. The authors must acknowledge the brief timeline and the fact that the patient was lost to follow-up. While we do believe that she has maintained some improvement, based upon her phone call, we are unable to confirm that she has followed her treatment protocol. We also acknowledge some reliance on the patient’s self-report of being up-to-date on screening labs to arrive at her diagnosis. Despite these limitations, we believe that the patient’s rapid response merited this case report, and we are proud of the progress made.
Recalling the Therapeutic Order, we reflect on the notion that this treatment plan focuses on the bottom half of our pyramid, emphasizing gentle and effective therapies compared with pharmaceuticals that can have detrimental side effects in the long term (Figure 2).31,32 Specifically, we were able to establish her foundations of health with the exercise and sleep hygiene practices as well as stimulate the body’s ability to heal and support weakened systems with the supplements. We believe this treatment regimen may be an effective method for naturopathic physicians to employ, and more research regarding the efficacy of this protocol in the form of a comparative effectiveness study is warranted.
Figure 2. Naturopathic Therapeutic Order

References:
- Krishnan R. Roy-Byrne PP, Solomon D, eds. Unipolar depression in adults: Epidemiology, pathogenesis, and neurobiology. Last updated February 13, 2019. UpToDate Web site. https://tinyurl.com/y5ttl5go. Accessed November 4, 2018.
- Angst F, Stassen HH, Clayton PJ, Angst J. Mortality of patients with mood disorders: follow-up over 34-38 years. J Affect Disord. 2002;68(2-3):167-181.
- aan het Rot M, Mathew SJ, Charney DS. Neurobiological mechanisms in major depressive disorder. CMAJ. 2009;180(3):305-313.
- Price JL, Drevets WC. Neurocircuitry of mood disorders. Neuropsychopharmacology. 2010;35(1):192-216.
- Vreeburg SA, Hoogendijk WJ, van Pelt J, et al. Major depressive disorder and hypothalamic-pituitary-adrenal axis activity: results from a large cohort study. Arch Gen Psychiatry. 2009;66(6):617-626.
- Gillespie CF, Nemeroff CB. Hypercortisolemia and depression. Psychosom Med. 2005;67 Suppl 1:S26-S28.
- Howren MB, Lamkin DM, Suls J. Associations of depression with C-reactive protein, IL-1, and IL-6: a meta-analysis. Psychosom Med. 2009;71(2):171-186.
- Patel A. Review: the role of inflammation in depression. Psychiatr Danub. 2013;25 Suppl 2:S216-S223.
- Kiecolt-Glaser JK, Derry HM, Fagundes CP. Inflammation: depression fans the flames and feasts on the heat. Am J Psychiatry. 2015;172(11):1075-1091.
- Kohler O, Krogh J, Mors O, Benros ME. Inflammation in Depression and the Potential for Anti-Inflammatory Treatment. Curr Neuropharmacol. 2016;14(7):732-742.
- Berk M, Williams LJ, Jacka FN, et al. So depression is an inflammatory disease, but where does the inflammation come from? BMC Med. 2013;11:200.
- Liu T, Zhong S, Liao X, et al. A Meta-Analysis of Oxidative Stress Markers in Depression. PLoS One. 2015;10(10):e0138904.
- Tyring S, Gottlieb A, Papp K, et al. Etanercept and clinical outcomes, fatigue, and depression in psoriasis: double-blind placebo-controlled randomised phase III trial. Lancet. 2006;367(9504):29-35.
- Raison CL, Rutherford RE, Woolwine BJ, et al. A randomized controlled trial of the tumor necrosis factor antagonist infliximab for treatment-resistant depression: the role of baseline inflammatory biomarkers. JAMA Psychiatry. 2013;70(1):31-41.
- Hirsch M, Birnbaum RJ. Selective serotonin reuptake inhibitors: Pharmacology, administration, and side effects. Last updated January 31, 2018.UpToDate Web site. https://tinyurl.com/yy87o225. Accessed December 7, 2018.
- Kovich H, Dejong A. Common Questions About the Pharmacologic Management of Depression in Adults. Am Fam Physician. 2015;92(2):94-100.
- American Psychiatric Association. Depressive Disorders. In: Diagnostic and Statistical Manual of Mental Disorders, Fifth Ed. Washington, DC: American Psychiatric Association Publishing; 2013.
- Lyness JM. Unipolar depression in adults: Assessment and diagnosis. Last updated September 13, 2016. UpToDate Web site. https://tinyurl.com/y6topkds. Accessed December 7, 2018.
- Mikkelsen K, Stojanovska L, Apostolopoulos V. The effects of vitamin B in depression. Curr Med Chem. 2016;23(38):4317-4337.
- Strasser B, Sperner-Unterweger B, Fuchs D, Gostner JM. Mechanisms of Inflammation-Associated Depression: Immune Influences on Tryptophan and Phenylalanine Metabolisms. Curr Top Behav Neurosci. 2017;31:95-115.
- Lindseth G, Helland B, Caspers J. The effects of dietary tryptophan on affective disorders. Arch Psychiatr Nurs. 2015;29(2):102-107.
- Gelenberg AJ, Gibson CJ. Tyrosine for the treatment of depression. Nutr Health. 1984;3(3):163-173.
- Panossian A, Wikman G. Evidence-based efficacy of adaptogens in fatigue, and molecular mechanisms related to their stress-protective activity. Curr Clin Pharmacol. 2009;4(3):198-219.
- Sarris J, Murphy J, Mischoulon D, et al. Adjunctive Nutraceuticals for Depression: A Systematic Review and Meta-Analyses. Am J Psychiatry. 2016;173(6):575-587.
- Mocking RJ, Harmsen I, Assies J, et al. Meta-analysis and meta-regression of omega-3 polyunsaturated fatty acid supplementation for major depressive disorder. Transl Psychiatry. 2016;6:e756.
- Kvam S, Kleppe CL, Nordhus IH, Hovland A. Exercise as a treatment for depression: A meta-analysis. J Affect Disord. 2016;202:67-86.
- Balchin R, Linde J, Blackhurst D, et al. Sweating away depression? The impact of intensive exercise on depression. J Affect Disord. 2016;200:218-221.
- Lee A, Myung SK, Cho JJ, et al. Night Shift Work and Risk of Depression: Meta-analysis of Observational Studies. J Korean Med Sci. 2017;32(7):1091-1096.
- Dewald-kaufmann JF, Oort FJ, Meijer AM. The effects of sleep extension and sleep hygiene advice on sleep and depressive symptoms in adolescents: a randomized controlled trial. J Child Psychol Psychiatry. 2014;55(3):273-283.
- Kennedy S. Full remission: a return to normal functioning. J Psychiatry Neurosci. 2002;27(4):233-234.
- Zeff J, Snider P, Pizzorno JE. Section I: Philosophy of Natural Medicine. In: Textbook of Natural Medicine, 3rd ed. St Louis, MO: Elsevier; 2006.
- Jakubovski E, Varigonda AL, Freemantle N, et al. Systematic Review and Meta-Analysis: Dose-Response Relationship of Selective Serotonin Reuptake Inhibitors in Major Depressive Disorder. Am J Psychiatry. 2016;173(2):174-183.
 Courtney K. Pickworth, BA, is a 4th-year medical student studying naturopathic medicine and integrative medical research. “Katie”’s background is in clinical research, including a 2-year post-baccalaureate fellowship at the National Institutes of Health focusing on the relationship between psychological and physical health. Katie is a highly involved, passionate member of the NUNM community and hopes to continue as a physician-scientist after graduating in 2019.
Courtney K. Pickworth, BA, is a 4th-year medical student studying naturopathic medicine and integrative medical research. “Katie”’s background is in clinical research, including a 2-year post-baccalaureate fellowship at the National Institutes of Health focusing on the relationship between psychological and physical health. Katie is a highly involved, passionate member of the NUNM community and hopes to continue as a physician-scientist after graduating in 2019.
***
 Lai Chim Chan, ND, is an assistant professor at the College of Naturopathic Medicine at the National University of Natural Medicine (NUNM). Dr Chan is Course Director for the Cardiology and Pulmonology block in the ND program at NUNM. She serves as the cardiology and pulmonology attending physician at the NUNM Health Centers, in addition to providing naturopathic primary care in private practice at the Center for Natural Medicine.
Lai Chim Chan, ND, is an assistant professor at the College of Naturopathic Medicine at the National University of Natural Medicine (NUNM). Dr Chan is Course Director for the Cardiology and Pulmonology block in the ND program at NUNM. She serves as the cardiology and pulmonology attending physician at the NUNM Health Centers, in addition to providing naturopathic primary care in private practice at the Center for Natural Medicine.